PLR和NLR对非ST段抬高型急性冠状动脉综合征院内不良事件的预测
2019-09-10胡昌灿于海初孙桂霞郭俊杰刘晓川张晓东
胡昌灿 于海初 孙桂霞 郭俊杰 刘晓川 张晓东
[摘要] 目的 探討血液炎症标志物血小板/淋巴细胞比值(PLR)、中性粒细胞/淋巴细胞比值(NLR)与非ST段抬高型急性冠状动脉综合征(NSTE-ACS)风险分层及院内预后的相关性,评估PLR和NLR对院内心血管事件的预测价值。方法 选取NSTE-ACS病人372例,其中有心血管不良事件(MACE)组36例,无MACE组336例,比较两组基线临床资料、PLR、NLR的差异,评估PLR、NLR与院内MACE的相关性;应用Logistic回归分析NLR、PLR与NSTE-ACS病人院内MACE事件的相关性;通过受试者工作特征曲线(ROC曲线)分析PLR、NLR对院内MACE的预测价值,并比较预测价值大小。结果 与无MACE组比较,有MACE组年龄、尿酸、NLR、PLR、Gensini评分均明显升高,舒张压、肌酐清除率(Ccr)水平明显降低,差异有统计学意义(t=-4.879~4.345,P<0.01)。Logistic回归分析显示,NLR(r=1.322,95%CI=1.067~1.638)、PLR(r=1.012,95%CI=1.005~1.019)为NSTE-ACS病人发生院内MACE的独立预测因子。ROC曲线分析显示,PLR、NLR预测院内MACE发生的面积分别为0.739、0.737;应用MEDCALC的Delong方法分析二者的曲线下面积差异无统计学意义(P>0.05)。根据对院内MACE最大预测价值的PLR值分为两组,PLR>127.5组收缩压、Ccr显著低于PLR≤127.5组,PLR及Gensini评分指标显著高于PLR≤127.5组,差异有统计学意义(t=-2.61~20.74,P<0.05);PLR>127.5组院内MACE、急性心力衰竭及非致死性心肌梗死发生率显著高于PLR≤127.5组,差异均有统计学意义(χ2=10.46~31.77,P<0.05)。根据NLR值分为两组,NLR>2.0组较NLR≤2.0组肌钙蛋白-I(TnI)、总胆红素、谷草转氨酶(AST)、肌酐、NLR、Gensini评分显著增高,差异有统计学意义(t=2.30~16.91,P<0.05);NLR>2.0组院内MACE、急性心力衰竭及非致死性心肌梗死发生率均显著高于NLR≤2.0组(χ2=5.89~25.48,P<0.05)。结论 PLR与NLR均为NSTE-ACS发生院内MACE的独立预测因子,二者对院内MACE的预测价值相当。
[关键词] 急性冠状动脉综合征;血小板计数;中性粒细胞;淋巴细胞
[中图分类号] R542.2 [文献标志码] A [文章编号] 2096-5532(2019)04-0485-07
[ABSTRACT] Objective To investigate the correlation of two blood inflammatory markers, neutrophil-lymphocyte ratio (NLR) and platelet-lymphocyte ratio (PLR), with risk stratification and in-hospital prognosis of non-ST segment elevation acute coronary syndrome (NSTE-ACS), and to evaluate the predictive value of NLR and PLR for in-hospital cardiovascular events. Methods A total of 372 patients with NSTE-ACS were divided into major adverse cardiovascular events (MACE) group (n=36) and non-MACE group (n=336). Baseline clinical data, PLR, and NLR were compared between the two groups to evaluate the correlation of PLR and NLR with in-hospital MACE. Logistic regression was used to analyze the correlation of PLR and NLR with in-hospital MACE in patients with NSTE-ACS. The receiver operating characteristic (ROC) curve was used to evaluate the predictive value of PLR and NLR for in-hospital MACE and compare the predictive value between them. Results Compared with the non-MACE group, the MACE group had significantly increased age, uric acid level, NLR, PLR, and Gensini score as well as significantly reduced diastolic blood pressure and creatinine clearance rate (Ccr) (t=-4.879 to 4.345,P<0.01). The logistic regression analysis showed that NLR and PLR were independent predictors of in-hospital MACE in patients with NSTE-ACS (r=1.322,95%CI=1.067-1.638;r=1.012,95%CI=1.005~1.019). The area under the ROC curve for in-hospital MACE was 0.739 and 0.737 for PLR and NLR, respectively. There was no significant difference in the area under the curve between NLR and PLR according to the Delong method of MEDCALC (P>0.05). All the patients were divided into two groups according to the PLR or NLR values with the maximum predictive value for in-hospital MACE. The PLR>127.5 group had significantly lower systolic blood pressure and Ccr as well as significantly higher PLR and Gensini score than the PLR ≤127.5 group (t=-2.61 to 20.74,P<0.05). The PLR>127.5 group also had significantly higher incidence rates of in-hospital MACE, acute heart failure, and nonfatal myocardial infarction than the PLR ≤127.5 group (χ2=10.46-31.77,P<0.05). The NLR>2.0 group had significantly higher levels of troponin I, total bilirubin, aspartate transaminase, creatinine, NLR, and Gensini score than the NLR ≤2.0 group (t=2.30-16.91,P<0.05). The NLR>2.0 group also had significantly higher incidence rates of in-hospital MACE, acute heart failure, and nonfatal myocardial infarction than the NLR ≤2.0 group (χ2=5.89-25.48,P<0.05). Conclusion Both PLR and NLR are independent predictors of in-hospital MACE in patients with NSTE-ACS. They have similar predictive value for in-hospital MACE.
[KEY WORDS] acute coronary syndrome; platelet count; neutrophile granulocyte; lymphocytes
非ST段抬高型急性冠状动脉综合征(NSTE-ACS)为冠心病的常见类型,其发病率及致死率在我国均呈上升趋势,若NSTE-ACS早期进行危险分层、尽早干预则对改善其预后至关重要[1]。血小板/淋巴细胞比值(PLR)及中性粒细胞/淋巴细胞比值(NLR)为新型、容易检测的全身炎症反应标志物,近年有研究显示,PLR、NLR与NSTE-ACS冠状动脉病变严重程度、危险分层及预后显著相关[2-7]。但PLR与NLR对NSTE-ACS病人院内心血管不良事件(MACE)预测价值大小国内外鲜有研究。本研究回顾性分析2016年7月—2017年7月在青岛大学附属医院心内科住院NSTE-ACS病人372例的临床资料,旨在评估PLR、NLR与NSTE-ACS风险分层及院内预后的相关性,探讨PLR与NLR对院内心血管事件的预测价值。
1 资料和方法
1.1 研究对象
NSTE-ACS病人372例,男225例,女147例。NSTE-ACS诊断符合2016年中华医学会的《非ST段抬高急性冠状动脉综合征诊断和治疗指南》[1]。纳入标准:病人年龄18~85岁;均经冠状动脉造影(CAG)检查并证实至少存在1支冠状动脉血管狭窄>50%。排除标准:①临床资料不全;②合并急、慢性感染性疾病;③肝肾功能严重受损;④合并血液系统疾病、恶性肿瘤或自身免疫性疾病;⑤既往有冠状动脉介入治疗或冠状动脉旁路移植术(CABG)病史;⑥正在服用或既往长期服用影响血常规的药物;⑦近期接受重大外科手术或者创伤;⑧碘或碘造影剂过敏。
1.2 研究方法
1.2.1 临床资料采集 收集受试者入院时临床基线资料,包括年龄、性别、收缩压、舒张压、高血压史、糖尿病史及吸烟史,入院24 h内心肌酶检查结果,实验室检查指标包括三酰甘油(TG)、总胆固醇(TC)、谷丙转氨酶(ALT)、谷草转氨酶(AST)、低密度脂蛋白胆固醇(LDL-C)、高密度脂蛋白胆固醇(HDL-C)、肌酐、空腹血糖、尿酸等,血常规指标包括中性粒细胞计数、血小板计数、淋巴细胞计数、平均血小板体积(MPV)等,术前心脏彩超检查结果主要包括左心室射血分数(LVEF)。
1.2.2 CAG检查 所有受试者均采用Judkin法行选择性CAG,多体位投照,对左前降支、左回旋支、右冠状动脉中至少1支血管狭窄≥75%或左主干狭窄≥50%的病人行急诊或择期经皮冠状动脉介入(PCI)治疗处理罪犯血管,罪犯血管通过心电图、心脏超声及血管内超声等检查,由2位经验丰富的心内科介入医师评定。其中行PCI治疗359例;未达到上述标准仅行CAG后药物治疗3例;达到上述标准,但考虑冠状动脉病变严重行CABG治疗10例。
1.2.3 Gensini评分 按CAG结果,用Gensini评分标准[8]对冠状动脉及其分支病变严重程度进行评估。①根据狭窄程度进行评分:1%~25%为1分,26%~50%为2分,51%~75%为4分,76%~90%为8分,91%~99%为16分,100%为32分。②病变部位系数:左冠状动脉主干×5.0;前降支近段×2.5,中段×1.5;心尖支及第一对角支均×1.0,第二对角支×0.5;回旋支近段×2.5,鈍缘支、回旋支远段及后降支均×1.0,后侧支×0.5;右冠状动脉近、中、远段均×1.0,后降支×1.0。③病变的积分:以每条冠状动脉狭窄程度评分×该病变部位的系数。如病人有多处血管病变,则以各病变的评分总和为该病人冠状动脉病变严重程度的总积分。
1.2.4 院内主要MACE 包括全因死亡、急性心力衰竭、非致死性心肌梗死、新发恶性心律失常等的发生情况。
1.3 统计学方法
采用SPSS 24.0及MEDCALC软件进行统计学分析,计量资料结果以±s形式表示,各组间符合正态分布且方差齐的计量资料比较采用独立样本的t检验,方差不齐的采用t′检验;计数资料以频数或率表示,数据间比较采用卡方检验。应用单因素及多因素Logistic回归分析评估PLR、NLR与院内MACE的相关性;应用受试者工作特征曲线(ROC曲线)分别评估PLR、NLR对NSTE-ACS病人院内MACE的灵敏度和特异度,Delong方法对PLR、NLR的ROC曲线进行比较。以P<0.05为差异有统计学意义。
2 结 果
2.1 有无发生院内MACE病人临床特点比较
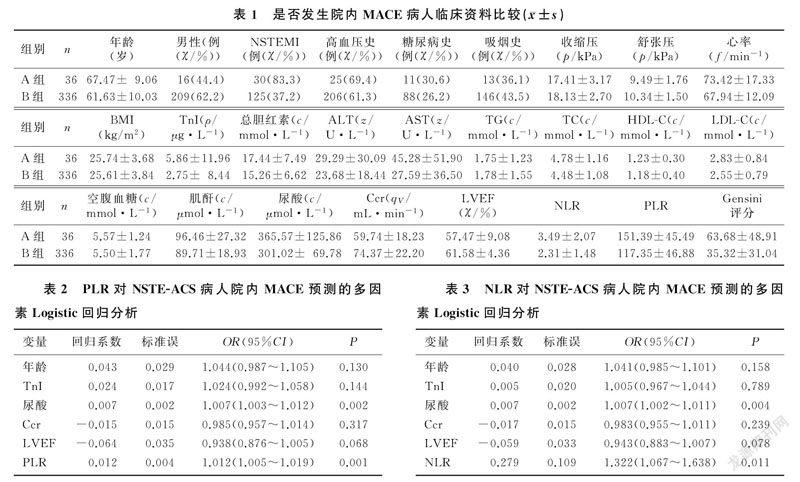
根据是否发生院内MACE,将372例NSTE-ACS病人分为有MACE组(A组)36例以及无MACE组(B组)336例。与无MACE组相比较,有MACE组年龄、尿酸、NLR、PLR、Gensini评分明显升高,舒张压、肌酐清除率(Ccr)水平明显降低,差异有统计学意义(t=-4.879~4.345,P<0.01)。两组高血压史、糖尿病史、吸烟史、总胆红素、ALT、TG、TC、HDL-C、LDL-C、空腹血糖、肌酐等指标比较差异无显著性(P>0.05)。见表1。
2.2 NLR、PLR与院内MACE发生的相关性
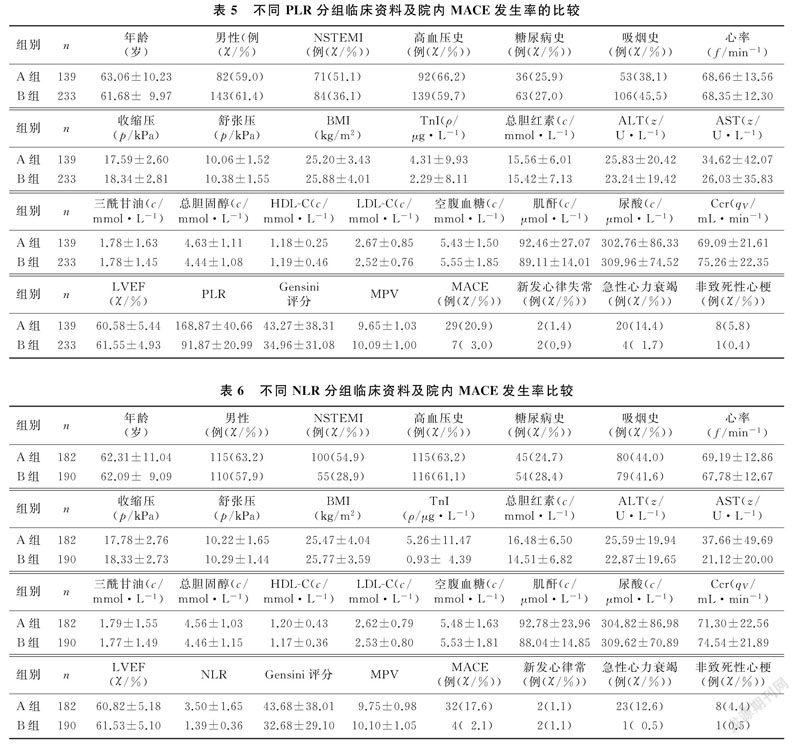
Spearman分析显示,NLR与PLR有相关性(ρ=0.634,P<0.01)。以NSTE-ACS病人是否发生MACE为因变量,以发生MACE为1、未发生MACE为0,年龄、高血压史、糖尿病史、TnI、空腹血糖、尿酸、Ccr、LVEF、PLR、NLR为自变量,先行单因素分析对自变量筛选。结果显示,年龄、TnI、尿酸、Ccr、LVEF、PLR、NLR与是否发生MACE正相关(r=0.906~1.388,P<0.05)。多因素Logistic回归分析显示,年龄、TnI、尿酸、Ccr、LVEF等为MACE的影响因素,PLR(OR=1.012,95%CI为1.005~1.019,P=0.001)、NLR(OR=1.322,95%CI为1.067~1.638,P=0.011)为发生院内MACE的独立预测因子。见图1和表2、3。
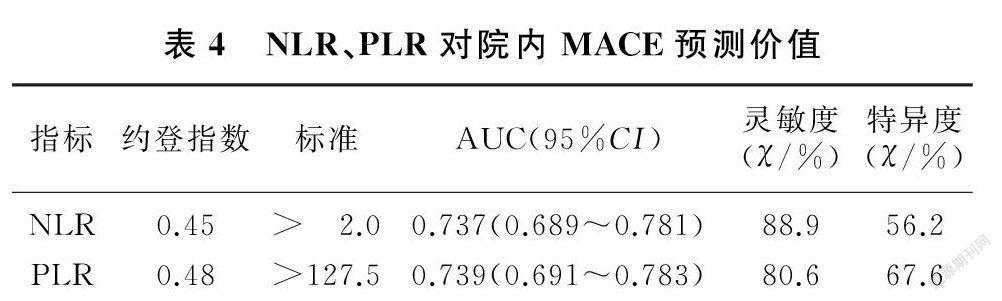
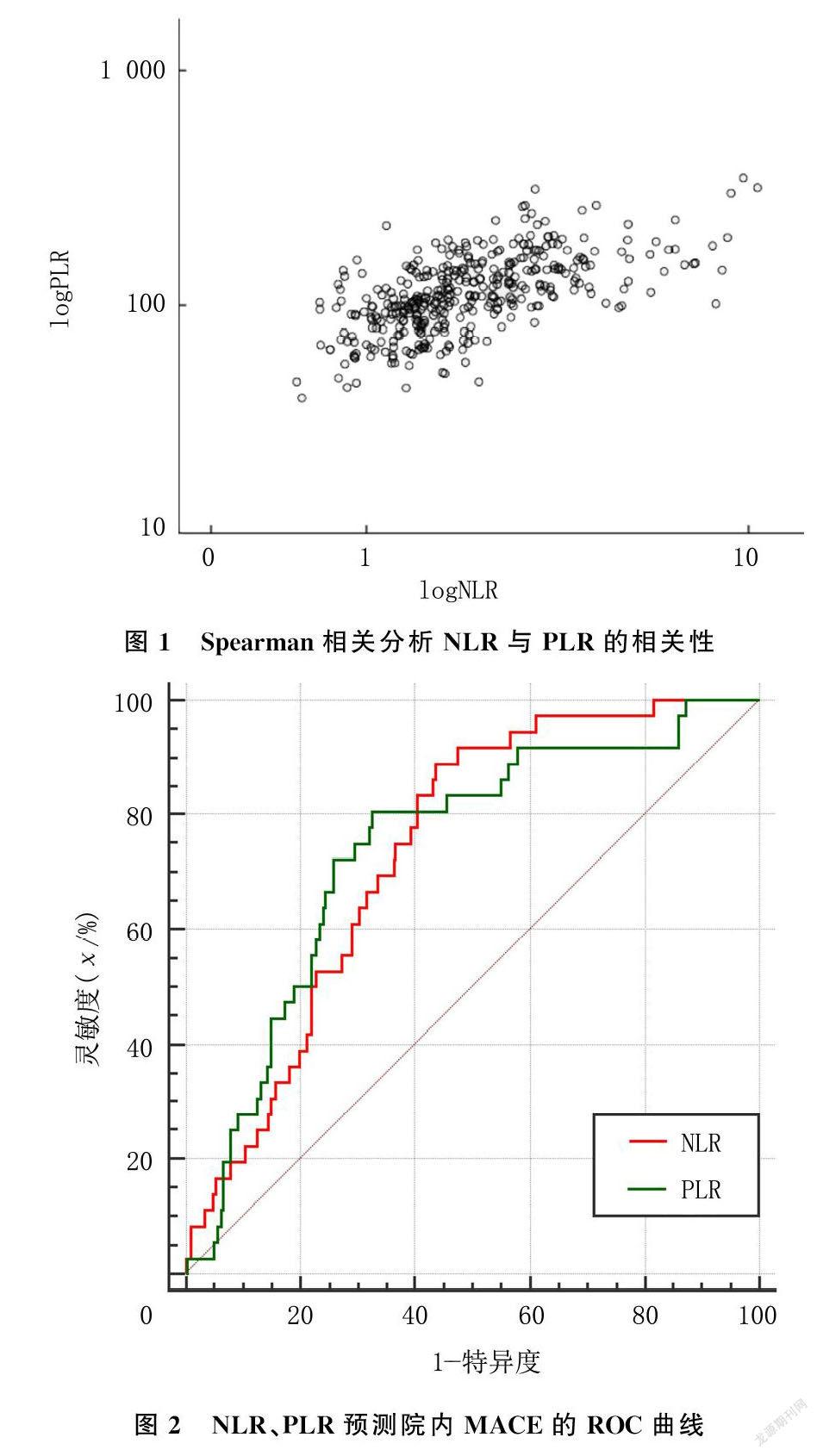
2.3 PLR、NLR对院内MACE发生的预测价值
ROC曲线分析显示,PLR、NLR的曲线下面积(AUC)分别为0.739、0.737(均大于0.5),对MACE具有一定的预测价值。应用Delong方法分析显示,PLR与NLR预测院内MACE发生的AUC相比较,差异无统计学意义(P=0.96),提示PLR与NLR对院内MACE的预测价值相当(图2)。当PLR=127.5时其对院内MACE的预测价值最大,灵敏度为80.6%,特异度为67.6%;当NLR=2.0时其对院内MACE事件的预测价值最大,灵敏度为88.9%,特异度为56.2%。见表4。
2.4 不同PLR、NLR值对临床相关指标及院内MACE的影响
根据对院内MACE最大预测价值的PLR值,
3 讨 论
急性冠状动脉综合征(ACS)是由于冠状动脉严重狭窄和(或)易损斑块破裂或糜烂所致的急性血栓形成,伴或不伴血管收縮、微血管栓塞,冠状动脉血流减低和心肌缺血而引起一系列临床症状的急性临床综合征[1]。ACS包括急性ST段抬高型心肌梗死(STEMI)、非ST段抬高型心肌梗死及不稳定型心绞痛。STEMI致死、致残率高,对STEMI病人早期再灌注治疗能有效降低发生心源性猝死风险,已成为普遍共识。同样,NSTE-ACS作为冠心病的严重类型,其发病率及致死率在我国呈上升趋势,因此对于NSTE-ACS早期进行危险分层、尽早干预,改善其预后至关重要[9]。
本研究结果显示,NSTE-ACS病人中PLR与NLR均为NSTE-ACS发生院内MACE的独立预测因子,二者对院内MACE的预测价值相当。
炎症反应参与冠状动脉粥样硬化的所有阶段。NLR、PLR作为重要的血液炎症反应标志物[10-11],与NSTE-ACS的发生、发展均密切相关[12-13]。发生NSTE-ACS时,坏死心肌和受损的基质产生损伤相关分子模式(DAMPs),从而激活补体级联反应,刺激Toll样受体/白细胞介素-1,导致核因子κB活化并诱导细胞因子、趋化因子和黏附分子,导致梗死区中性粒细胞和单核细胞聚集、外渗[14]。另一方面,发生NSTE-ACS时引起的应激反应及心肌损伤可导致肾上腺素、糖皮质激素升高,引起外周血白细胞升高,同时糖皮质激素会诱发细胞凋亡,引起淋巴细胞减少[5]。因此,NLR作为两种炎性因子的组合被认为是一项重要的血液炎症反应标志物[10]。
PLR最初作为一种炎症反应标志物,用来评估肿瘤病人的预后[15-16]。随着研究的不断深入,其逐渐被用来评估各种心血管疾病,如高血压、冠心病、外周动脉闭塞疾病病人的预后[17-20]。PLR与心血管疾病及不良事件预后相关的机制尚不明确,但PLR代表血小板比例的增高及淋巴细胞比例的减少。一方面有不少研究显示,各种刺激如系统感染、炎性状态、出血等的作用可促进一系列炎症递质,如白细胞介素-1(IL-1)、IL-3、IL-6等的释放,刺激巨核细胞增殖,引起血小板增多,导致血小板活化增加,进而形成血栓前状态[21-22]。活化的血小板可释放多种炎症递质,促进单核细胞的黏附和迁移,加剧炎症反应,在动脉粥样硬化的起始和发展过程中起到关键作用,同时在内皮损伤及斑块破坏的环境下加速动脉粥样斑块的不稳定性及血栓的形成[7]。另一方面,淋巴细胞反映的是一种静止的且可控的炎症通路[7]。炎症增加淋巴细胞的凋亡[23],引起淋巴细胞计数减少;同时,心肌缺血时,机体处于生理压力及应激状态,导致皮质醇及儿茶酚胺等激素水平增高也可引起淋巴细胞计数的减少[24]。因此,PLR作为两种炎性因子的组合,既反映了炎症反应,又反映了血栓形成过程,该指标被认为是一种重要的血液炎症反应标志物。而NLR、PLR因容易获得且检测价格便宜,在评估ACS病人冠状动脉病变程度和预测MACE方面的临床价值,已受到人们越来越多的关注[25]。
国内外大量的研究显示,NLR、PLR与冠状动脉狭窄程度及ACS的预后显著相关。KURTUL等[21]对1 016例经CAG确诊的ACS病人研究发现,高PLR病人的冠状动脉SYNTAX评分更高,提示PLR与冠状动脉粥样硬化的严重程度及复杂
SAHIN等[29]研究结果表明,根据SYNTAX评分,NLR是STEMI冠状动脉狭窄严重程度的独立预测因子。与SYNTAX评分一样,Gensini评分是评估冠心病复杂性和严重程度的有效的血管造影工具。CHEN等[30]研究发现,根据Gensini评分,NLR与冠心病病人冠状动脉狭窄严重程度密切相关。SAWANT等[31]对250例经过血运重建的STEMI病人1年的随访发现,NLR>7.4是预测短期(<30 d)及长期(1年)预后的一个良好的指标。GUL等[12]对诊断为NSTEMI及不稳定型心绞痛的病人进行长达3年的随访,发现低NLR病人的3年病死率为3%,而高NLR病人的3年病死率高达21.6%,差异有统计学意义;NLR=3.4是NSTEMI及不稳定型心绞痛病人3年病死率的最佳预测截断值,表明NLR为NSTEMI及不稳定型心绞痛病人3年病死率的独立预测因子。AYCA等[32]对450
虽然大量研究显示PLR与NLR对ACS预后都有一定的预测价值,但目前国内外还没有二者对NSTE-ACS病人院内MACE的预测价值比较的研究。本文Logistic分析的结果显示,PLR、NLR均为NSTE-ACS病人发生院内MACE的独立预测因子。进一步通过ROC曲线等分析发现,NLR、PLR对NSTE-ACS病人发生院内MACE预测的临床价值比较差异无统计学意义,提示二者对NSTE-ACS病人发生院内MACE的预测价值相当。究其原因,NLR及PLR中都有淋巴细胞计数的存在,且都反映了NSTE-ACS的炎症状态,故NLR与PLR并不是各自独立的,具有一定相关性。
综上所述,PLR与NLR均为NSTE-ACS病人发生院内MACE的独立预测因子,而且二者对院内MACE的预测价值相当。本研究还有一些不足之处。首先,本文研究为单中心、回顾性研究;其次,研究人群样本数量较少,发生院内MACE病人较少,今后需扩大样本量进一步研究。
[参考文献]
[1] 中華医学会心血管病学分会. 非ST段抬高型急性冠状动脉综合征诊断和治疗指南(2016)[J]. 中华心血管病杂志, 2017,45(5):359-376.
[2] DINIZ L R, DE LIMA S G, DE AMORIM GARCIA J M, et al. Neutrophil to lymphocyte ratio as a prognostic predictor in older people with acute coronary syndrome[J]. Angiology, 2019,70(3):264-271.
[3] DENTALI F, NIGRO O, SQUIZZATO A, et al. Impact of neutrophils to lymphocytes ratio on major clinical outcomes in patients with acute coronary syndromes: a systematic review and meta-analysis of the literature[J]. International Journal of Cardiology, 2018,266:31-37.
[4] CHOI D H, KOBAYASHI Y, NISHI T, et al. Combination of mean platelet volume and neutrophil to lymphocyte ratio predicts long-term major adverse cardiovascular events after percutaneous coronary intervention[J]. Angiology, 2019,70(4):345-351.
[5] 王阳,贾淑杰,池喆. 中性粒细胞/淋巴细胞比值与非ST段抬高急性冠脉综合征患者危险分层及预后的相关性[J]. 中华医学杂志, 2017,97(23):1784-1789.
[6] ANWAR W I, WIJAYA I P. Diagnostic accuracy of platelet/lymphocyte ratio for screening complex coronary lesion in different age group of patients with acute coronary syndrome[J]. Acta Medica Indonesiana, 2018,50(3):185-192.
[7] LEE Y S, BARADI A, PEVERELLE M, et al. Usefulness of Platelet-to-Lymphocyte ratio to predict long-term all-cause mortality in patients at high risk of coronary artery disease who underwent coronary angiography[J]. American Journal of Cardiology, 2018,121(9):1021-1026.
[8] MARINI A, NAKA K K, VAKALIS K, et al. Extent of coronary artery disease in patients undergoing angiography for stable or acute coronary syndromes[J]. Hellenic Journal of Car-diology, 2017,58(2):115-121.
[9] BOB-MANUEL T, IFEDILI I, REED G A, et al. Non-ST elevation acute coronary syndromes: a comprehensive review[J]. Current Problems in Cardiology, 2017,42(9):266-305.
[10] BALTA S, OZTURK C, BALTA I, et al. The Neutrophil-Lymphocyte ratio and inflammation[J]. Angiology, 2016,67(3):298-299.
[11] AKBOGA M K, CANPOLAT U, YAYLA C, et al. Association of platelet to lymphocyte ratio with inflammation and severity of coronary atherosclerosis in patients with stable coronary artery disease[J]. Angiology, 2016,67(1):89-95.
[12] GUL M, UYAREL H, ERGELEN M, et al. Predictive value of neutrophil to lymphocyte ratio in clinical outcomes of Non-ST elevation myocardial infarction and unstable angina pectoris a 3-year follow-up[J]. Clinical and Applied Thrombosis-Hemostasis, 2014,20(4):378-384.
[13] TASKESEN T, SEKHON H, WROBLEWSKI I, et al. Usefulness of mean platelet volume to predict significant coronary artery disease in patients with non-ST-elevation acute coronary syndromes[J]. The American Journal of Cardiology, 2017,119(2):192-196.
[14] FANG L, MOORE X L, DART A M, et al. Systemic inflammatory response following acute myocardial infarction[J]. Journal of Geriatric Cardiology: JGC, 2015,12(3):305-312.
[15] KRENN-PILKO S, LANGSENLEHNER U, THURNER E M, et al. The elevated preoperative platelet-to-lymphocyte ratio predicts poor prognosis in breast cancer patients[J]. British Journal of Cancer, 2014,110(10):2524-2530.
[16] TEMPLETON A J, ACE O, MCNAMARA M G, et al. Prognostic role of platelet to lymphocyte ratio in solid tumors: a systematic review and meta-analysis[J]. Cancer Epidemiology, Biomarkers & Prevention: a Publication of the American Association for Cancer Research, Cosponsored by the American Society of Preventive Oncology, 2014,23(7):1204-1212.
[17] ACAR G, KALKAN M E, AVCI A, et al. The relation of Platelet-Lymphocyte ratio and coronary collateral circulation in patients with stable angina pectoris and chronic total occlusion[J]. Clinical and Applied Thrombosis-Hemostasis, 2015,21(5):462-468.
[18] SUNBUL M, GERIN F, DURMUS E, et al. Neutrophil to lymphocyte and platelet to lymphocyte ratio in patients with dipper versus non-dipper hypertension[J]. Clinical and Experimental Hypertension (New York, N.Y.:1993), 2014,36(4):217-221.
[19] GARY T, PICHLER M, BELAJ K, et al. Platelet-to-Lymphocyte ratio: a novel marker for critical limb ischemia in peripheral arterial occlusive disease patients[J]. PLoS One, 2013,8(7): e67688.
[20] KUNDI H. The role of platelet-lymphocyte ratio in the severity of coronary artery disease assessed by the angiographic Gensini score[J]. Anatolian Journal of Cardiology, 2016,16(3):224.
[21] KURTUL A, MURAT S N, YARLIOGLUES M A, et al. Association of Platelet-to-Lymphocyte ratio with severity and complexity of coronary artery disease in patients with acute coronary syndromes[J]. American Journal of Cardiology, 2014,114(7):972-978.
[22] WU Y H, WU H, MUELLER C, et al. Baseline platelet count and clinical outcome in acute coronary syndrome[J]. Circulation Journal, 2012,76(3):704-711.
[23] HOTCHKISS R S, KARL I E. The pathophysiology and treatment of sepsis[J]. New England Journal of Medicine, 2003,348(2):138-150.
[24] LI Hui, ZHOU Yun, MA Yan, et al. The prognostic value of the platelet-to-lymphocyte ratio in acute coronary syndrome: a systematic review and meta-analysis[J]. Kardiologia Polska, 2017,75(7):665-672.
[25] WANG Xuedong, XIE Zulong, LIU Xinxin, et al. Association of platelet to lymphocyte ratio with non-culprit atherosclerotic plaque vulnerability in patients with acute coronary syndrome: an optical coherence tomography study[J]. BMC Cardiovascular Disorders, 2017,17(1):175-180.
[26] CETIN E H, CETIN M S, ARAS D A, et al. Platelet to lymphocyte ratio as a prognostic marker of in-hospital and long-term major adverse cardiovascular events in ST-segment elevation myocardial infarction[J]. Angiology, 2016,67(4):336-345.
[27] AZAB B, SHAH N, AKERMAN M, et al. Value of platelet/lymphocyte ratio as a predictor of all-cause mortality after non-ST-elevation myocardial infarction[J]. Journal of Thrombosis and Thrombolysis, 2012,34(3):326-334.
[28] OYLUMLU M, YILDIZ A, OYLUMLU M, et al. Platelet to lymphocyte ratio is a predictor of in-hospital mortality patients with acute coronary syndrome[J]. European Heart Journal, 2014,35(1):648-659.
[29] SAHIN D Y, ELBASAN Z, GR M, et al. Neutrophil to lymphocyte ratio is associated with the severity of coronary artery disease in patients with ST-segment elevation myocardial infarction[J]. Angiology, 2013,64(6):423-429.
[30] CHEN Juan, CHEN Manhua, LI Sha, et al. Usefulness of the Neutrophil-to-Lymphocyte ratio in predicting the severity of coronary artery disease: a gensini score assessment[J]. Journal of Atherosclerosis and Thrombosis, 2014,21(12):1271-1282.
[31] SAWANT A C, ADHIKARI P, NARRA S R, et al. Neutrophil to lymphocyte ratio predicts short-and long-term mortality following revascularization therapy for ST elevation myocardial infarction[J]. Cardiology Journal, 2014,21(5):500-508.
[32] AYCA B, AKIN F, CELIK O, et al. Neutrophil to lymphocyte ratio is related to stent thrombosis and high mortality in patients with acute myocardial infarction[J]. Angiology, 2015,66(6):545-552.
[33] CETIN M, KIZILTUNC E, ELALMIS O U, et al. Predictive value of neutrophil lymphocyte ratio and platelet lymphocyte ratio in patients with coronary slow flow[J]. Acta Cardiologica Sinica, 2016,32:307-312.
(本文編辑 黄建乡)