Post-oesophagectomy gastric conduit outlet obstruction following caustic ingestion, endoscopic management using a SX-ELLA biodegradable stent: A case report
2019-06-11MusbahiYKSViswanath
A Musbahi, YKS Viswanath
A Musbahi, YKS Viswanath, Upper GI Laparoscopic and Endoscopic Unit, James Cook University Hospital, Middlesbrough TS43BW, Cleveland, United Kingdom
Abstract
Key words:: Biodegradable; Stent; Oesophagectomy; Case report
INTRODUCTION
Benign upper gastrointestinal and oesophageal strictures secondary to caustic ingestion are rare and management remains challenging. They often present with symptoms such as chest pain, dysphagia and vomiting[1]. Symptomatic strictures often require endoscopic intervention usually via dilatation either using a balloon or bougie[2]. Patients with recurrent strictures are offered endoscopic stent using a biodegradable (BD) stent rather a self-expanding metallic stent. The later are associated with problems secondary to migration, erosions and the need for their removal. Surgical resection is often not justified in majority of these cases who later presents with recurrent benign stricture.
We report a patient with a back-ground history of psychiatric illness and who have undergone Ivor Lewis oesophagectomy with vagotomy for operable cancer 5 years prior. He presents with chest pain vomiting and weight loss with recent history of caustic ingestion. Endoscopy and imaging assessments revealed post-oes-ophagectomy gastric conduit outlet obstruction (POGO) and he failed to respond to initial endoscopy dilatations. Consequently, a decision to manage POGO with a BD stent was taken with a successful outcome.
CASE PRESENTATION
Chief complaints
We present a 69-year-old man with previous curative two stage Ivor Lewis oesophagectomy with concomitant pyloroplasty, 5 years prior for operable oes-ophageal adenocarcinoma.
History of past illness
He carried a past history of bipolar psychiatric illness requiring multiple emergency admissions with history of deliberate self-harm.
History of present illness
He presented to emergency ro om with history of caustic ingestion with symptoms of odynophagia, dysphagia, hematemesis, chest pain and vomiting. Patient was treated conservatively with high dose proton pump inhibitors, tranexamic acid, blood products, antibiotics, total parenteral nutrition initially followed by enteral nutrition.After initial endoscopic assessments, he was discharged on high dose proton pump inhibitors. Three months later, he represents with weight loss, chest pain and vomiting.
FINAL DIAGNOSIS
Subsequent assessments on endoscopy, CT, chest X ray (Figure 1A), contrast swallow(Figure 1B), a diagnosis of caustic stricture with fibrosis at pyloric channel of the gastric conduit was established (POGO, Enteral naso-jejunal feed was used to oversee his nutrition and allowed intake of his routine medication. Treatment with initial twoballoon dilatations and one bougie dilatation (Figure 2) failed with follow-on recurrence of vomiting. All along, at endoscopy he was found to have lot of fluid residue in the gastric conduit alongside negotiable pyloric channel with difficulty.This was due to angulation diaphragmatic hiatus and associated scarring on over one third of its circumference. He was then considered for the possibility of placement of a BD stent with definitive intent rather a removable metallic stent.
TREATMENT
Placement of BD stent; Under sedation, with midazolam (5 mg) and Alfentanyl (150 micrograms), a 24 mm SX-ELLA (019-10A-28/23/28-080) BD stent (Figure 3A) was placed over a guidewire under X-ray guidance. The deployed Ella BD stent had a diameter of 23 mm for the body and 28 mm for proximal and distal flare. A conclusion contrast stentogram confirmed satisfactory position of BD stent, so also on check completion endoscopy (Figure 3B and C). He was kept as an inpatient for 48 h with intravenous antiemetics and was allowed oral fluids and liquid diet for 6 wk.
OUTCOME AND FOLLOW-UP
Follow up at 8 wk and 6 mo revealed complete symptomatic resolution with improved nutritional status and subsequently he was discharged. Follow up X ray confirmed normal looking shadow of the decompressed conduit without a fluid level(Figure 4)
DISCUSSION
In upper gastrointestinal tract, oesophageal strictures of benign etiology can occur commonly secondary to gastro-esophageal reflux disease, post-surgery such as oesophagectomy at the anastomosis, after radiotherapy or secondary to caustic ingestion[1]. However, benign stricture following caustic ingestion causing pyloric channel stricture at the outlet of gastric conduit are rare.
Management of benign upper GI and esophageal strictures remains challenging.Mainly in majority of endoscopy units, the dilation is carried out with either a bougie or a balloon. More than 80% of these patients usually respond and a proportion of them need more than one session. Around 10% develop a refractory or recurrent stricture. These usually require several dilatations raising risks of bleeding and perforation[2].
Oesophageal strictures can be simple or complex. Simple strictures are short (< 2 cm), focal, straight, and passable with an endoscope such oesophageal web or Schatzki's ring. A non-passable or significantly narrowed diameter (< 12 mm)stricture, that is longer than 2 cm and tortuous are deemed complex. These are mainly occur following surgery, radiotherapy or corrosive ingestion and are difficult treat[3].Management of POGO remains a challenge, endoscopic intervention is technically demanding given the angulation at the level of diaphragm and postsurgical anatomic configuration.
Recurrent and refractory strictures are usually distinguished by; fibrotic stenosis restricting the oesophageal lumen, absence of active inflammation or motility disorder, and failure to achieve a luminal diameter of 14 mm for 4 wk after 5, two weekly dilatations[3].
There are no defined characteristics for refractory POGO published in the literature.In this case, persistent symptoms and failed 3 dilations are taken in to account prior to the placement of a BD stent.
Since 2008, BD stents are accessible for endoscopic intervention; they usually degrade after 11-12 wk. Therefore, BD stents are an attractive substitute to treat dysphagia secondary to benign or malignant strictures[4]. Placement of a BD stent is seen as an alternative to repeated dilatations in a patient with benign refractory stricture, with the objective of reducing dilatations and allowing remodeling at stricture site[5].
The use of stents as a palliative measure in malignant strictures has been well established. A range of benign stenosing disorders of the esophagus and upper gastro-intestinal tract can also be treated safely with a self-expanding or BD plastic stent such as benign oesophageal strictures secondary to peptic disease or caustic injury[5]. In this case, ingested caustic caused initial inflammation with ulceration followed by pyloric channel fibrosis, resulting in POGO. This is a distinctive casereport we know of a BD stent being used in an obstructed gastric conduit in a postoesophagectomy patient to treat a caustic stricture of the pylorus. We advocate attending gastroenterologist to contemplate using BD stents in selected patients at similar clinical situations.
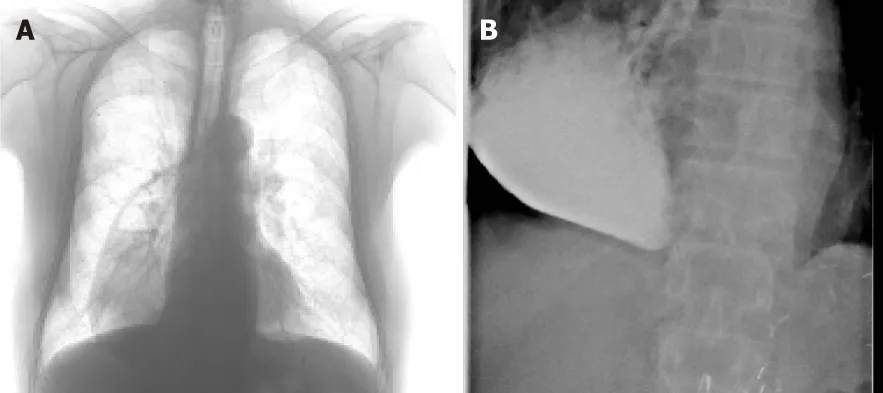
Figure 1 Chest x ray with a dilated gastric conduit with air fluid level and a contrast X ray showing meagre passage of contrast with dilated gastric conduit.
CONCLUSION
In this article, authors have illustrated the role of a BD stent in the management of caustic pyloric stricture. The treating endoscopic physician should contemplate the usage of a BD stent in these challenging situations even after oesophagectomy. The role of a BD stent in the management caustic Upper GI refractory stricture is not well understood needs further investigation.

Figure 2 Bougie dilatation with two clip markers at the site of pyloric stricture.
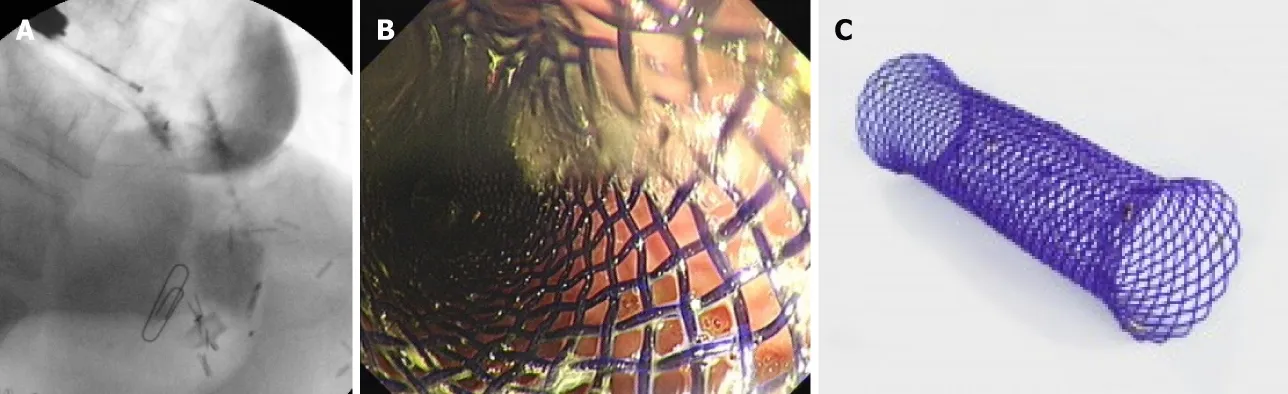
Figure 3 Contract X ray deployed biodegradable stent with endoscope in the gastric conduit together injection catheter, endoscopic and outside view of the biodegradable stent.

Figure 4 X ray showing well decompressed gastric conduit with proximal radio opaque markers of the biodegradable stent.
杂志排行
World Journal of Gastrointestinal Endoscopy的其它文章
- Role of endoscopic vacuum therapy in the management of gastrointestinal transmural defects
- Endoscopic ultrasound-guided biliary drainage: A change in paradigm?
- Should a fully covered self-expandable biliary metal stent be anchored with a double-pigtail plastic stent? A retrospective study
- Role of colonoscopy in diagnosis of capecitabine associated ileitis:Two case reports
- Comprehensive review on EUS-guided biliary drainage
- Endoscopic characteristics of small intestinal malignant tumors observed by balloon-assisted enteroscopy
