Should a fully covered self-expandable biliary metal stent be anchored with a double-pigtail plastic stent? A retrospective study
2019-06-11SaadEmhmedAliWesamFrandahLeonSuCoryFieldingHoussamMardini
Saad Emhmed Ali, Wesam M Frandah, Leon Su, Cory Fielding, Houssam Mardini
Saad Emhmed Ali, Department of Internal Medicine, Division of Hospital Medicine,Department of Internal Medicine, University of Kentucky, Lexington, KY 40536, United States
Wesam M Frandah, Cory Fielding, Houssam Mardini, Department of Internal Medicine, Division of Gastroenterology, Department of Internal Medicine, University of Kentucky, Lexington,KY 40536, United States
Leon Su, Department of Statistics, College of Arts and Sciences, College of Public Health,University of Kentucky, Lexington, KY 40536, United States
Abstract
Key words:Metal stents; Double-pigtail plastic stent; Endoscopic retrograde cholangiopancreatography; Biliary drainage; Biliary obstruction
INTRODUCTION
Fully covered self-expandable metal stents (FCSEMSs) have been widely used as an effective biliary endoprosthesis in the setting of pancreaticobiliary conditions such as benign and malignant strictures, post-sphincterotomy bleeding, and occasionally bile leaks[1]. The primary advantages of covered stents are a lower rate of tumor ingrowth,longer patency, and their potential removability compared to uncovered stents.However, one concern about FCSEMSs is a higher migration rate than uncovered stents[2]. The migration rate of FCSEMSs in prospective studies for benign biliary strictures is 5%-37%[1]. In this study, we conducted a retrospective analysis to evaluate the efficacy of 7-French (Fr) and 10-Fr double-pigtail plastic stent (DPS) within the FCSEMS as an anti-migration technique. We compared the rate of stent migration between patients who received FCSEMS alone and those who received both an FCSEMS and anchoring DPS in a large patient population with both benign and malignant strictures as well as non-stricture etiologies.
MATERIALS AND METHODS
Between July 2015 and April 2017, 1366 patients had undergone endoscopic retrograde cholangiopancreatography (ERCP) at our institution. Among these, 203 patients with FCSEMS placement with or without DPS were identified. The review and analysis were conducted through our endoscopy reporting system (ProVation®MD) and medical records. Patients included in the study had FCSEMS insertion for the treatment of malignant biliary stricture, benign biliary stricture, and non-stricture etiology such as post-sphincterotomy bleeding and bile leak.
After the Institutional Review Board and the Ethics Committee of our hospital approved the study protocol, data was extracted by reviewing patient charts, ERCP reports, and fluoroscopic images. Patients who only had uncovered stents or plastic stents placed were excluded. All endoscopic procedures were performed by three advanced endoscopists. Comprehensive data were collected through Microsoft Excel spreadsheet and included the following: stent type [WallflexTM (Boston Scientific)vsViabil® (Gore Medical)], the diameter of double-pigtail PS (7-Frvs10-Fr), indications for FCSEMS placement including stricture type (malignantvsbenign), and nonstricture etiologies such as post-sphincterotomy bleeding and bile leak.
Baseline patient characteristics were identified, such as previous cholecystectomy,biliary sphincterotomy, history of stent migration, choledocholithiasis, and diameter of the common bile duct (CBD). After stent placement and during the follow-up period, patients' records were reviewed to verify the stent position. We defined FCSEMS migration endoscopically if the stent was no longer visible through the major papilla. It either migrates proximally (into the bile duct) or distally (out of the bile of duct). The anti-migration properties of FCSEMSs include higher radial force,anchoring flap, anchoring fins and flared ends have been designed to prevent the migration. Categorical data were analyzed using the Chi-Square test and Fisher Exact test and continuous data using non-parametric tests. A regression analysis was performed to identify factors independently associated with increased risk of stent migration. All analyses were completed in SAS 9.4 (SAS Institute Inc., Cary, NC,United States).
The primary endpoint of the study was to compare stent migration rates between patients who received FCSEMSs alone and those who received both an FCSEMS with an anchoring DPS. A secondary endpoint was the presence of complications related to stent migration.
RESULTS
1366 patients had undergone ERCP by three advanced endoscopists over 21-mo period; among these, 203 patients had FCSEMS placed with or without DPS (88 females and 115 males). 65 patients had FCSEMSs with DPS, and 138 had FCSEMSs alone (Table 1 and Table 2). 95 patients had a malignant stricture, 82 patients had a benign stricture, 12 patients had bile leak, 12 patients had cholangitis, and nine patients had post-sphincterotomy bleeding (Figure 1). For the patients with stent migration, 12 (66.7%) had a benign biliary stricture, and 6 (33.3%) did not have, while for the patients without stent migration, 70 (37.8%) had a benign biliary stricture and 115 (62.2%) did not have (P= 0.01). Also. For patients with stent migration, 12 (66.7%)had the previous sphincterotomy, and 6 (33.3%) did not have, while for the patients without stent migration, 71 (38.4%) had the previous sphincterotomy and 114 (61.6%)did not have (P= 0.01). The migration rate in patients with benign biliary stricture was 14.6% and for those with non-benign biliary stricture was 5%. Migration rate in patients with the previous sphincterotomy was 14.5%, and those without previous sphincterotomy was 5%. Therefore, the distribution of patients that had a benign biliary stricture and previous sphincterotomy were significantly different between patients with stent migration and patients with no stent migration. There was no significant association between any of the other tested variables including anchoring the FCSEMSs with DPS and the risk of stent migration. The migration rate in patients with anchored FCSEMSs with DPS was 6%, and those without anchoring DPS was 10% (P= 0.35). Overall, migration was reported in 18 patients with FCSEMS placement out of 203 patients with an overall migration rate of 9.7%.
DISCUSSION
FCSEMS has been associated with longer patency than uncovered stents in some studies even though they may have higher rates of migration[3-5]. To minimize the riskof migration, FCSEMSs have been designed with anti-migration mechanical properties, such as higher radial force, an anchoring flap, and specific stent flare structures[6-8]. Nevertheless, other modifications such as anchoring fins and flared ends have been designed to prevent the migration of FCSEMSs, even though; there are no randomized studies to evaluate their effectiveness[7,9].
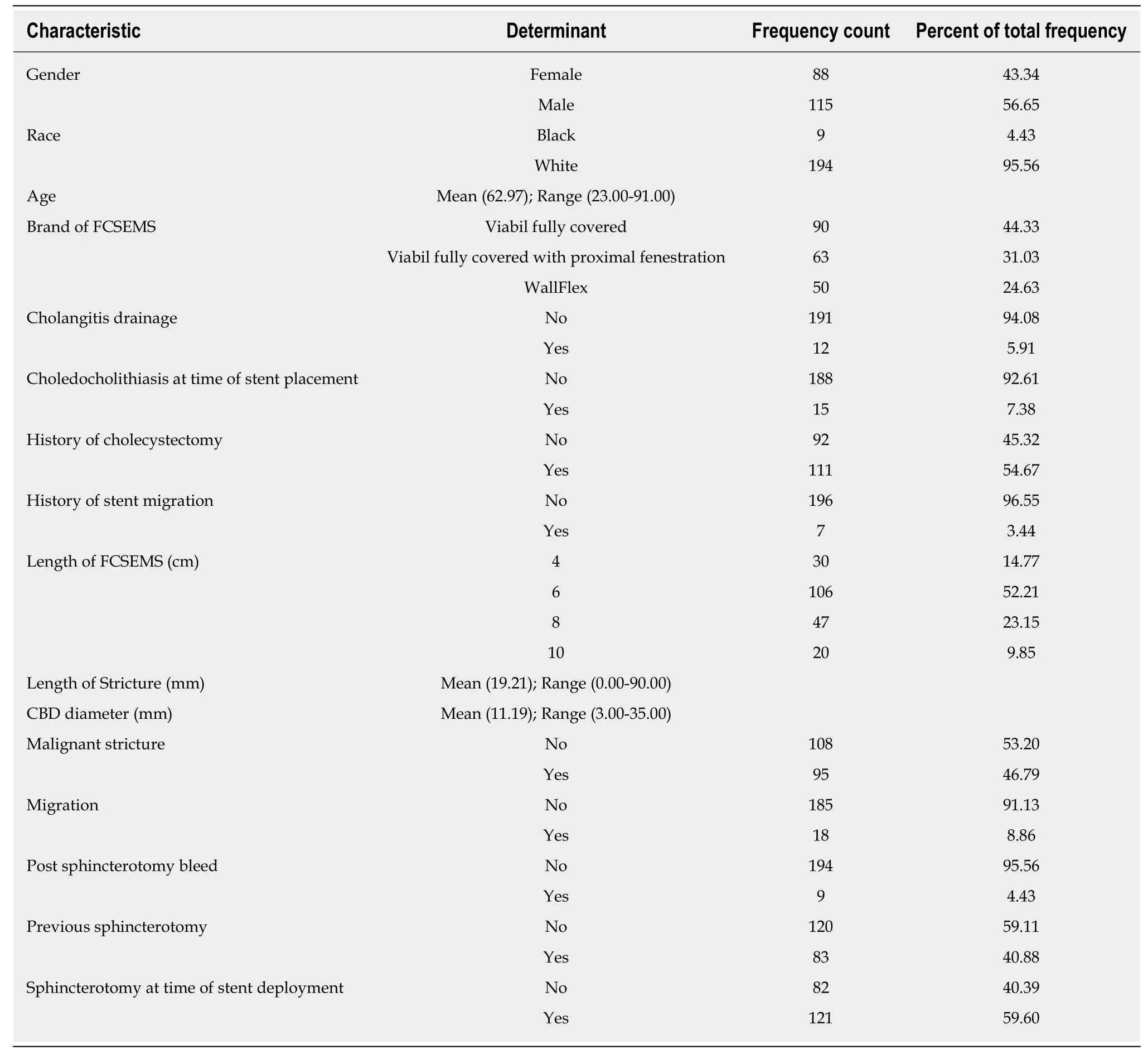
Table 1 Clinical characteristics of patients who underwent fully covered self-expanding metal stent placement with or without doublepigtail plastic stent
In our study, the risk of migration of biliary FCSEMS seemed to be lower than previous studies at 9.7%. In contrast, migration rates have been reported to be up to 37.5% in the previous study[1]. To our knowledge, there are only two studies that have evaluated the efficacy of anchoring DPS to prevent migration of FCSEMS.
In a randomized controlled study, Parket al[10]described their experience of placing a 5-Fr DPS into FCSEMS in 17 patients out of 33 patients who received FCSEMS for benign biliary strictures. During the follow-up, the migration rate was significantly lower in the anchored group (FCSEMS + anchoring DPS) compared with a nonanchored group (FCSEMS alone): 1/16 (6.3%)vs7/17 (41.2%) respectively,P= 0.024.However, in the study by Parket al[10], their sample size was underpowered to identify any significant clinical difference between the two groups and the study was terminated before the planned sample size was reached.
Recently, Katsineloset al[11]investigated the efficacy of using a 10-Fr DPS to prevent migration in 10 patients with malignant biliary strictures and one patient with a suprapapillary benign biliary stenosis. These patients were prospectively enrolled.
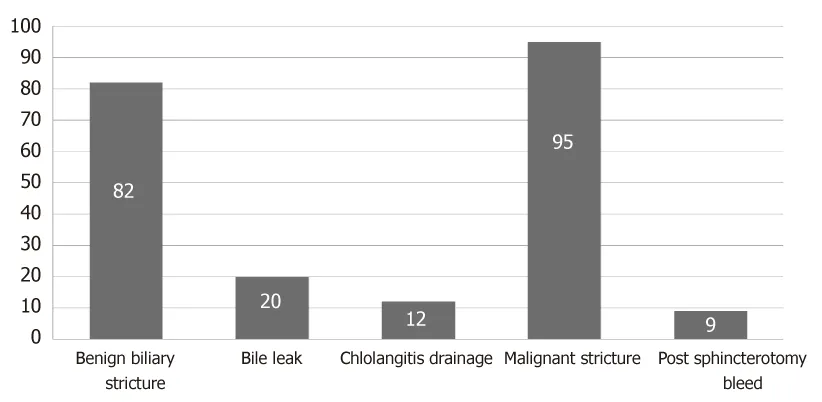
Figure 1 Indication for fully covered self-expandable metal stent with or without double-pigtail plastic stent placement.
The median follow-up period was eight months, and no migration of FCSEMS was reported. Even though it was the first study to assess the use of anchoring a 10-Fr DPS inside an FCSEMS as anti-migration technique, it was limited by small sample size and lack of randomization.
Our study contains a much larger sample size than the studies described above.Also, we included patients with a variety of indications for FCSEMS placement, such as benign and malignant biliary stricture, post sphincterotomy bleed, cholangitis drainage, and bile leak. Our study was different from the above studies because 90%of DPS were 7-Fr and 10% were 10-Fr.
The complication rate from stent migration was very low in our study. Five patients developed obstructive jaundice due to stent migration, and only one patient developed stent-induced cholecystitis secondary to the occlusion of the cystic orifice by a proximally migrated stent in a patient with pancreatic cancer. Acute cholecystitis after placement of a biliary metallic stent has been reported in up to 13% and is likely associated with tumor involvement at the orifice of the cystic duct[12-14].
This study was limited by being retrospective and not being randomized. However,this is the first study to investigate the efficacy of a 7-Fr DPS inside an FCSEMS as an anti-migration technique and the first study to assess the migration rate of FCSEMS with or without anchoring DPS among those with non-stricture etiologies such postsphincterotomy bleeding and bile leak.
In conclusion, our findings suggest that anchoring of FCSEMS with a 7-Fr or 10-Fr DPS does not decrease the risk of stent migration. Only benign biliary stricture and previous Sphincterotomy were to have a significant association with stent migrations(P= 0.01). We did not find evidence to support the routine placement of anchoring DPS. However, prospective randomized controlled studies are needed to evaluate the efficacy of an anchoring DPS within an FCSEMS as an anti-migration technique.
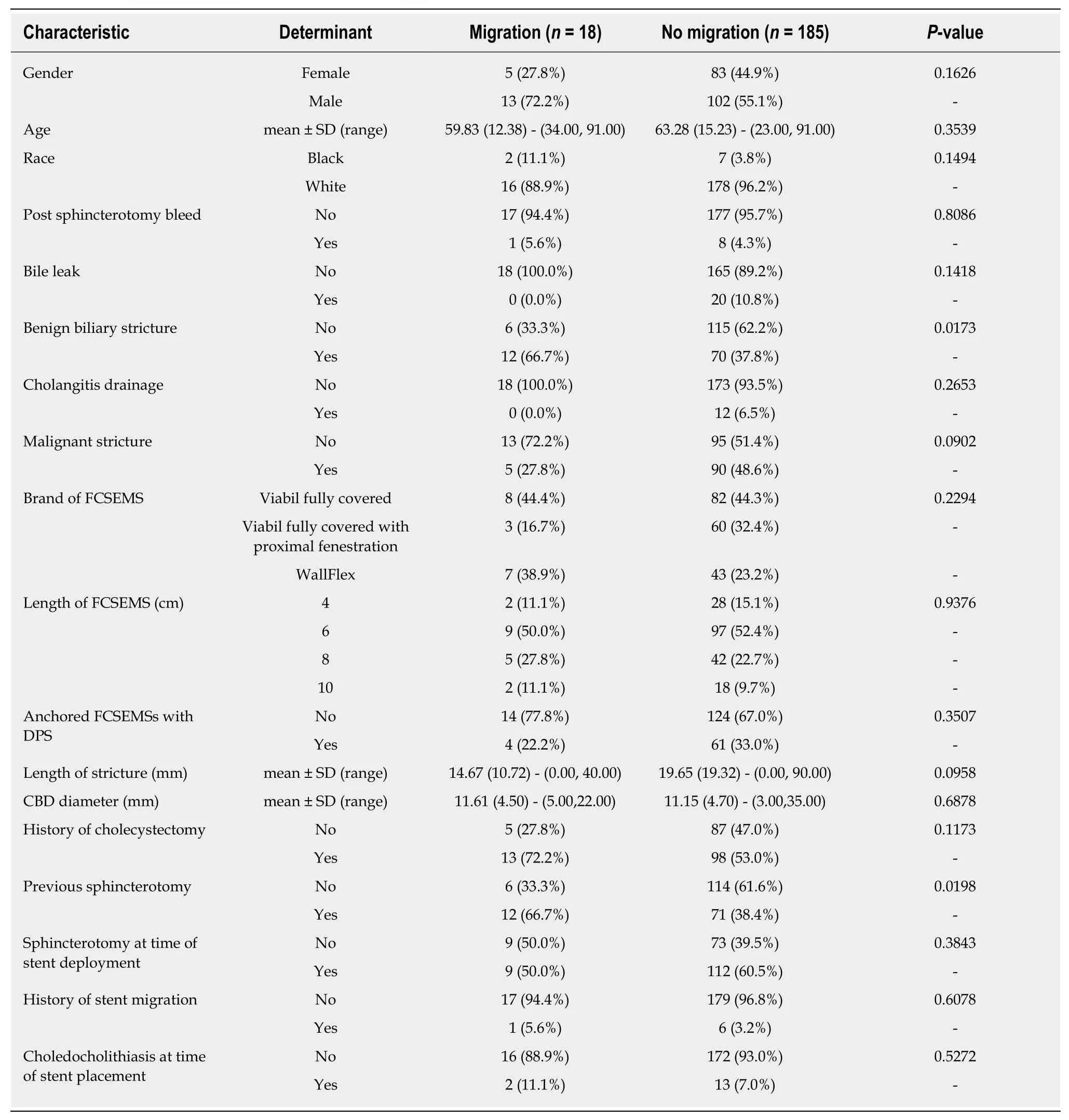
Table 2 Comparison between patients who had migration of fully covered self-expanding metal stent placement (FCSEMS) and patient who had no migration of FCSEMS
ARTICLE HIGHLIGHTS
Research background
Fully covered self-expandable metal stents (FCSEMSs) have been widely used as an effective biliary endoprosthesis in the setting of pancreaticobiliary conditions such as benign and malignant strictures, post-sphincterotomy bleeding, and occasionally bile leaks. The primary advantages of covered stents are a lower rate of tumor ingrowth, longer patency, and their potential removability compared to uncovered stents. However, one concern about FCSEMSs is a higher migration rate than uncovered stents. In this study, we conducted a retrospective analysis to evaluate the efficacy of 7-French (Fr) and 10-Fr double-pigtail plastic stent (DPS) within the FCSEMS as an anti-migration technique. We compared the rate of stent migration between patients who received FCSEMS alone and those who received both an FCSEMS and anchoring DPS in a large patient population with both benign and malignant strictures as well as nonstricture etiologies. We did not find evidence to support the routine placement of anchoring DPS.We found that anchoring of FCSEMS with a 7-Fr or 10-Fr DPS does not decrease the risk of stent migration.
Research motivation
FCSEMSs have been commonly used as an effective biliary endoprosthesis in the setting of pancreaticobiliary conditions such as benign and malignant strictures. To minimize the risk of migration, FCSEMSs have been designed with different anti-migration mechanical properties.The use of DPS is still unclear as an anti-migration method. Prospective randomized controlled studies are needed to evaluate the efficacy of an anchoring DPS within an FCSEMS as an antimigration technique.
Research objectives
The main objective of the study was to assess to the rate of stent migration between patients who received FCSEMS alone and those who received both an FCSEMS and anchoring DPS in both benign and malignant strictures as well as non-stricture etiologies. To our knowledge, there are only two small retrospective studies that have evaluated the efficacy of anchoring DPS to prevent migration of FCSEMS. So, more randomized controlled trials with a larger number of patients are needed.
Research methods
A retrospective analysis of endoscopy reporting system and medical records of patients who underwent ERCP with FCSEMS placement was conducted. The review and analysis were conducted through our endoscopy reporting system (ProVation® MD) and medical records.Patients included in the study had FCSEMS insertion for the treatment of malignant biliary stricture, benign biliary stricture, and non-stricture etiology such as post-sphincterotomy bleeding and bile leak. Data included stent type [WallflexTM (Boston Scientific)vsViabil® (Gore Medical)], the diameter of double-pigtail PS (7-Frvs10-Fr), and indications for FCSEMS placement. We defined FCSEMS migration endoscopically if the stent was no longer visible through the major papilla. It either migrates proximally (into the bile duct) or distally (out of the bile of duct).
Research results
There was no significant association between any of the other tested variables including anchoring the FCSEMSs with DPS and the risk of stent migration. The migration rate in patients with anchored FCSEMSs with DPS was 6%, and those without anchoring DPS was 10% (P=0.35). Overall, migration was reported in 18 patients with FCSEMS placement out of 203 patients with an overall migration rate of 9.7%. The distribution of patients that had a benign biliary stricture and previous sphincterotomy were significantly different between patients with stent migration and patients with no stent migration.
Research conclusions
In our study, the risk of migration of biliary FCSEMS was 9.7 %. Anchoring an FCSEMS with a 7-Fr or 10-Fr DPS does not decrease the risk of stent migration. Routine placement of anchoring stents is unnecessary. We believe that further randomized controlled trials with a larger number of patients might be helpful to ascertain if anchoring an FCSEMS with DPS is useful as an antimigration technique.
Research perspectives
Anchoring of FCSEMS with a 7-Fr or 10-Fr DPS does not decrease the risk of stent migration.Only benign biliary stricture and previous Sphincterotomy were to have a significant association with stent migrations. Needs more prospective large studies. More randomized controlled trials with a larger number of patients are needed.
杂志排行
World Journal of Gastrointestinal Endoscopy的其它文章
- Role of endoscopic vacuum therapy in the management of gastrointestinal transmural defects
- Endoscopic ultrasound-guided biliary drainage: A change in paradigm?
- Role of colonoscopy in diagnosis of capecitabine associated ileitis:Two case reports
- Post-oesophagectomy gastric conduit outlet obstruction following caustic ingestion, endoscopic management using a SX-ELLA biodegradable stent: A case report
- Comprehensive review on EUS-guided biliary drainage
- Endoscopic characteristics of small intestinal malignant tumors observed by balloon-assisted enteroscopy
