Long-term survival of a patient with advanced pancreatic cancer under adjunct treatment with Viscum album extracts: A case report
2019-04-15PaulWerthmannRobertKempenichGerlindeLangAvrousGunverKienle
Paul G Werthmann, Robert Kempenich, Gerlinde Lang-Avérous, Gunver S Kienle
Paul G Werthmann, Gunver S Kienle, Department of Methodology, Institute for Applied Epistemology and Medical Methodology (IFAEMM), Freiburg 79111, Germany
Paul G Werthmann, Gunver S Kienle, Center for Complementary Medicine, Institute for
Environmental Health Sciences and Hospital Infection Control, Medical Center - University of Freiburg, Freiburg 79106, Germany
Robert Kempenich, Private Praxis, General Practitioner with Specialization in Oncology,Strasbourg F-67000, France
Gerlinde Lang-Avérous, Department of Pathology, Hôpital de Hautepierre, University Hospital of Strasbourg, Strasbourg F-67000, France
Abstract BACKGROUND Advanced pancreatic cancer (aPC) has a poor prognosis with limited survival benefit from current standard treatment. Viscum album extracts (VAE) are used by many cancer patients, showing immune-stimulating effects, improved quality of life, and a survival benefit in patients with aPC.CASE SUMMARYA 59-year-old architect developed epigastric pain. A cystic lesion of the pancreas of 45-mm diameter was detected. In a follow-up magnetic resonance imaging,about one year later, multiple lesions were seen in the corpus and the tail of the pancreas; CA-19-9 was elevated to 58.5 U/mL. A distal pancreatectomy with splenectomy was performed, and a tumor of 7 cm × 5 cm × 3.5 cm was excised.Histologic investigation showed an intraductal papillary mucinous neoplasmassociated invasive adenocarcinoma with invasion of the lymph vessels,perineural invasion, and positive nodes (2/27); surgical margins showed tumor cells, and the tumor was classified as pT3 N1 M0 R1. The patient was treated with radiation of the tumor bed and capecitabine/oxaliplatin followed by gemcitabine and FOLFIRINOX. Seven months after surgery, a liver metastasis was detected and treatment with FOLFIRINOX was started. Four months after detection of the metastasis, the patient opted for additional treatment with VAE. Another month later, the metastasis was treated with radiofrequency ablation (RFA). Eight months later, the hepatic lesion recurred and was again treated with RFA. The continuous VAE treatment was increased in dose, and the patient stayed recurrence-free for the next 39 mo in good health and working full-time (as of the time this case report was written).CONCLUSION We present the case of a patient with aPC with R1-resection with development of liver metastasis during the course of treatment who showed an overall survival of 63 mo and a relapse-free survival of 39 mo under increasing VAE therapy. The possible synergistic effect on tumor control of RFA treatment and immunestimulatory effects of VAE should be further investigated.
Key words: Pancreatic cancer; Integrative medicine; Viscum album extract;Radiofrequency ablation; Case report
INTRODUCTION
Pancreatic cancer (PC) is a common malignancy (incidence 12.6/100.000 in the United States[1]), with a dismal prognosis (5-year survival of 2%[2]), especially in cases of locally advanced disease (median survival of 8-12 mo[3]). Intraductal papillary mucinous neoplasm (IPMN)-associated invasive adenocarcinoma of the pancreas is a histologic subtype of PC that has to be kept distinct from mucinous cystic neoplasms of the pancreas[4]; IPMN-associated invasive adenocarcinoma shows a better prognosis due to earlier onset of clinical symptoms compared to pancreatic ductal adenocarcinoma (PDA). However, prognosis of IPMN-associated and standard PDA are equally poor when compared by stage[5]. In all PC patients in which R0-resection seems feasible, surgery is recommended. R0-resected patients show a strong survival benefit compared to R1-resected patients[6]. Type of chemotherapy regimen - as primary or adjuvant treatment - is chosen according to tumor stage and performance status[7]. Radiofrequency ablation (RFA) is increasingly used in advanced PC (aPC);the procedure is safe, but comparative randomized trials on effectiveness are lacking[8-10].
Viscum album(European mistletoe,Viscum album L.) is a hemiparasitic shrub,growing on different host trees (oak, apple, pine and others). AqueousViscum albumextracts (VAE) show a variety of antineoplastic properties including cytotoxic effects,apoptosis induction, immune stimulation, down-regulation of cancer genes (e.g.,transforming growth factor β and matrix-metalloproteinases), reduction of cell migration, and reduction of tumor angiogenesis[11-14]. Active compounds of VAE are especially mistletoe lectins and viscotoxins, but also oligo- and polysaccharides,flavonoids, and triterpene acids[14]. Injectable forms of VAE preparations (typically for subcutaneous use, or - as off-label use - for intralesional or intravenous application)are commercially available, and are used as supportive cancer therapy[15]. VAE show a common range of local reactions such as erythema at the injection site and general reactions like fever and flu-like symptoms. Rarely, pseudo allergic reactions can occur. VAE are safe, even when used in higher dosages[16].
CASE PRESENTATION
Chief complaints
A 59-year-old architect developed epigastric pain. He had a body mass index (BMI) of 30 (body weight of 92 kg, height of 175 cm) and was a nonsmoker.
History of present illness
Nothing to declare.
History of past illness
The patient had a history of bronchial asthma and suffered from gastroesophageal reflux disease, which was treated with esomeprazole.
Personal and family history
His father had died from metastatic colon cancer.
Laboratory examinations
CA-19-9 was elevated to 58.5 U/mL.
Imaging examinations
A cystic lesion of the pancreas of 45-mm diameter was seen in ultrasound and confirmed by computed tomography (CT) scan. In a follow-up magnetic resonance imaging (MRI), about one year after initial symptoms, multiple lesions were seen in the corpus and the tail of the pancreas (Figure 1A and B). A splenopancreatectomy was performed, and a tumor of 7 cm × 5 cm × 3.5 cm of the pancreatic tail was excised. Histologic investigation showed a poorly demarcated IPMN-associated hypermuzinous invasive adenocarcinoma with invasion of the lymph vessels,perineural invasion, and positive nodes (2/27); the tumor was 1 mm in the ventral resection margin, and the dorsal margin showed tumor parts (Figure 2). The tumor was classified as pT3 N1 M0 R1.
FINAL DIAGNOSIS
A patient with aPC.
TREATMENT
The patient was treated with radiation of the tumor bed (59.4 Gy) and capecitabine and oxaliplatin followed by gemcitabine and 8 cycles of FOLFIRINOX (folinic acid 390 mg, fluorouracil 4700 mg, irinotecan 340 mg, oxaliplatin 150 mg).
OUTCOME AND FOLLOW-UP
About 7 mo after surgery, a liver metastasis 2 cm in diameter in segment VIII was detected, and therefore treatment with FOLFIRINOX was started. Four months after detection of the metastasis the patient opted for additional continuous treatment with VAE (Iscador Qu 10 mg, 3 injections per week). Another month later, the metastasis was still unchanged despite chemotherapy and therefore treated with RFA. Eight months later, the hepatic lesion recurred within the scar tissue of the first metastasis,showing a lesion about 2 cm in diameter (Figure 1C and D). It was again treated by RFA and by a dose increase of VAE (Figure 3). The lesion regressed again and the patient stayed recurrence-free for the next 39 mo (as of the writing of this case report;for details of the disease and treatment course, see Figure 3).
DISCUSSION
We present a case of a 59-year-old patient with an aPC who underwent resection but showed positive margins (R1), with two relapses (liver metastases) after radiochemotherapy and RFA of metastases. The patient continuously received an adjunct treatment with VAE in increasing doses beginning shortly after detection of the liver metastasis and continuing until present. He showed prolonged survival and good health 63 mo after initial diagnosis. The patient had an advanced primary tumor, perineural invasion, lymph vascular invasion, node involvement, and positive resection margins - all of which are independent negative prognostic factors[17]. In this patient, surgical excision was possible - a circumstance associated with an improved prognosis. However, median survival of PC patients who have undergone surgical excision, regardless of stage or other prognostic factors, is 19 mo (interquartile range,10-42 mo)[18].
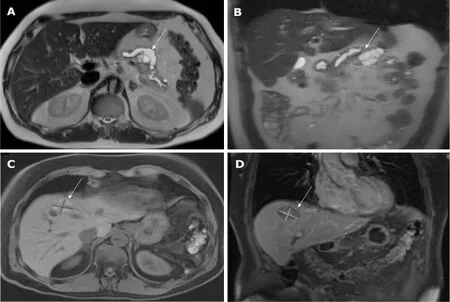
Figure 1 Magnetic resonance imaging images of the tumor lesions. A and B: primary tumor lesion 2 mo before the initial diagnosis: cystic lesion at the location between body and tail of the pancreas with a size of 43 mm × 38 mm × 30 mm; dilatation of the pancreatic duct of 13 mm (A: T2 axial, B: T2 coronal); C and D:Relapsed hepatic lesion in segment VIII in month 20 after initial diagnosis (C: T1 axial, D: T1 coronal).
VAE was repeatedly investigated in PC and showed cytotoxic effects in cell lines and animal studies (PA-TU-8902, PAXF 736, PAXF 546)[19-21]. Trögeret al[22]found a survival benefit for aPC patients solely treated with VAE in a randomized controlled trial on overall survival. Similar results were seen by Axtneret al[23]in an integrative oncology registry. In a phase 1 study of VAE and Gemcitabine in patients with advanced solid tumors (including PC) it could be shown, that VAE did not affect the pharmacokinetics of Gemcitabine[24]. VAE in PC is currently further investigated in clinical trials (NCT02948309).
RFA acts through direct thermal cell damage but shows additional immune stimulatory properties as tumor antigens and a variety of cytokines are released from the treated tumor tissue; increased numbers of tumor-specific T cells have been detected in RFA-treated patients[10]. Combination therapy of RFA with different immune-stimulatory agents showed promising results[25,26]. The combination of VAE with radiation - which, like RFA, leads to cell damage and to a release of antigens -proved to be more effective than radiation alone in animal studies[27,28]. VAE shows several immune-stimulating properties like proliferation induction and increase of antigen presentation of dendritic cells, proliferation of CD4+T cells, increase of natural killer cell-mediated cytotoxicity, and release of cytokines[14].
CONCLUSION
We presume that VAE acted synergistically with RFA, leading to tumor control.Reports of combined treatment with RFA and VAE should be collected to determine whether further investigations in this area are worthwhile.
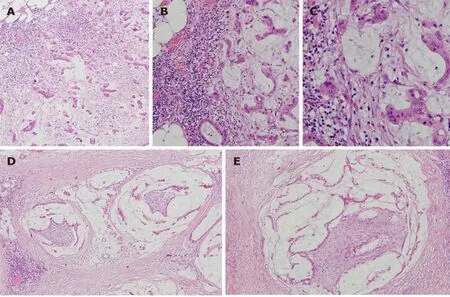
Figure 2 Patient's tumor, haematoxylin and eosin stain. A: × 100; B: × 200; C :( × 400) invasive mucinous adenocarcinoma; D and E: (× 100) perineural invasion.
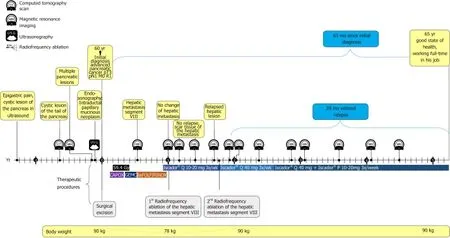
Figure 3 Timeline of the patient with advanced pancreatic cancer. Gy: Radiotherapy in Gray; CAPOX: Capecitabine + oxaliplatin; GEMC: Gemcitabine;FOLIFIRINOX: Leucovorin + fluorouracil + irinotecan + oxaliplatin.
ACKNOWLEDGEMENTS
We are thankful to Dr. Helmut Kiene (IFAEMM) for revision of the manuscript.
杂志排行
World Journal of Gastroenterology的其它文章
- International consensus statement on robotic hepatectomy surgery in 2018
- Growing burden of alcoholic liver disease in China: A review
- ?Esophageal diverticulum: New perspectives in the era of minimally invasive endoscopic treatment
- Gut microbiota profile in healthy Indonesians
- Ursodeoxycholic acid ameliorates hepatic lipid metabolism in LO2 cells by regulating the AKT/mTOR/SREBP-1 signaling pathway
- Risk factors for local recurrence and appropriate surveillance interval after endoscopic resection
