?Esophageal diverticulum: New perspectives in the era of minimally invasive endoscopic treatment
2019-04-15HirokiSatoManabuTakeuchiSatoruHashimotoKenichiMizunoKoichiFurukawaAkitoSatoJunjiYokoyamaShujiTerai
Hiroki Sato, Manabu Takeuchi, Satoru Hashimoto, Ken-ichi Mizuno, Koichi Furukawa, Akito Sato,Junji Yokoyama, Shuji Terai
Hiroki Sato, Satoru Hashimoto, Ken-ichi Mizuno, Junji Yokoyama, Shuji Terai, Division of Gastroenterology, Niigata University Medical and Dental Hospital, Niigata 951-8510, Japan
Manabu Takeuchi, Division of Gastroenterology, Nagaoka Red Cross Hospital, Nagaoka 940-2085, Japan
Koichi Furukawa, Division of Gastroenterology, Niigata City General Hospital, Niigata 950-1197, Japan
Akito Sato, Division of Gastroenterology, Nagaoka Chuo General Hospital, Nagaoka 940-8653,Japan
Abstract Esophageal diverticula are rare conditions that cause esophageal symptoms, such as dysphagia, regurgitation, and chest pain. They are classified according to their location and characteristic pathophysiology into three types: epiphrenic diverticulum, Zenker's diverticulum, and Rokitansky diverticulum. The former two disorders take the form of protrusions, and symptomatic cases require interventional treatment. However, the esophageal anatomy presents distinct challenges to surgical resection of the diverticulum, particularly when it is located closer to the oral orifice. Since the condition itself is not malignant,minimally invasive endoscopic approaches have been developed with a focus on alleviation of symptoms. Several types of endoscopic devices and techniques are currently employed, including peroral endoscopic myotomy (POEM). However,the use of minimally invasive endoscopic approaches, like POEM, has allowed the development of new disorder called iatrogenic esophageal diverticula. In this paper, we review the pathophysiology of each type of diverticulum and the current state-of-the-art treatment based on our experience.
Key words: Diverticulum; Esophagus; Epiphrenic diverticulum; Zenker's diverticulum;Rokitansky diverticulum; Iatrogenic disease; Esophageal achalasia; Peroral endoscopic myotomy; Diverticulectomy
INTRODUCTION
Esophageal diverticula comprise a rare condition that causes dysphagia, regurgitation, and chest pain as they progress. The pathophysiology of the diverticula varies according to their location in the esophagus (i.e., epiphrenic, Zenker's, and Rokitansky).
Interventional treatment should be considered for symptomatic cases. Although surgical resection of the diverticulum has traditionally been considered to be the only curative option, esophageal anatomy presents several challenges to surgery,particularly when the diverticulum is near the oral orifice. Some of the issues associated with surgery include the extensive invasiveness and risk of adverse events.Esophageal diverticula themselves are not malignant; hence, minimally invasive endoscopic treatment that avoids surgery is preferred. The primary purpose of interventions for esophageal diverticulum is to alleviate the patients' symptoms and improve their quality of life; therefore, we do not have to singularly focus on achieving complete excision of the diverticulum. However, the development of minimally invasive endoscopic approaches for the esophagus has led to a new kind of disorder called iatrogenic diverticula. Caution must be exercised to avoid the incidence of such diverticula.
In this paper, we review the pathophysiology and up-to-date treatment options for esophageal diverticulum based on our experience.
EPIPHRENIC DIVERTICULUM
Pathophysiology of epiphrenic diverticulum
Epiphrenic diverticula are pulsion-type diverticula that are usually located in the distal esophagus (Figure 1A and D). Histologically, they appear as pseudodiverticula lacking a muscle layer. Their pathogenesis is considered to be secondary to esophageal motility disorders and is associated with congenital weakness of the esophageal wall[1].
Recent studies have reported that more than 75% of epiphrenic diverticula occur concomitantly with esophageal motility disorders[2-8]. Therefore, evaluation of esophageal motility using high resolution manometry (HRM) is recommended before deciding on the intervention (Figure 1B)[9,10]. The right esophageal wall is more susceptible to epiphrenic diverticula[2,11], although the reason for this is still unclear. In contrast, spontaneous esophageal rupture tends to occur through the left wall (Table 1)[12].
Treatment of epiphrenic diverticulum
The classical indications for surgery are continued growth of the diverticulum, the presence of symptoms, and concomitant malignancy in the diverticulum.
The laparoscopic approach is the less invasive surgical choice. As described above,associated motility disorders of the esophagus are found in most cases; therefore, a myotomy through the lower esophageal sphincter (LES) and an anti-reflux procedure should be added to treat the primary problem and avoid gastroesophageal reflux[13].The long-term outcomes of surgical management are satisfactory[7,14,15]. However,Michaelet al's[16]study using a United States nationally representative database showed that the mortality rate associated with surgery for non-Zenker's diverticulum(ZD) was 1.6% and that the most common complication was air leakage (3.1%).Furthermore, the risk of postoperative morbidity was greater after thoracotomy than after laparoscopy (odds ratio: 7.45).
In 2010, Inoueet al[17]first reported a case series of achalasia successfully treated with peroral endoscopic myotomy (POEM). It is an innovative approach for endoscopic myotomy of the esophageal muscle layer through the mouth. POEM has been gaining attention due to its minimally invasive nature and equivalent efficacy for achalasia compared to that of conventional surgical approaches, such as Heller's myotomy[18,19]. We previously reported the first case of epiphrenic diverticulum successfully treated by salvage POEM (s-POEM)[20]. In s-POEM, endoscopic myotomy of the side opposite to the diverticulum was performed longitudinally, from the oral to the gastric terminus, and a thick muscle layer, including the LES, was completely dissected (Figure 1C). The patient's severe dysphagia and regurgitation subsequentlyresolved. Follow-up endoscopy showed no food remnants in the diverticulum or esophageal lumen, and a post-barium swallow test indicated smooth passage through the esophago-gastric junction (Figure 1D). One interesting aspect in this case was that the HRM showed no specific esophageal abnormalities, although the patient was suspected to have an esophageal motility disorder-related diverticulum based on the findings of the endoscopic and barium swallow examinations. Similarly, patients with disparate manometry (normal), and barium swallow (corkscrew esophagus) findings have been previously reported[2]. Based on this successful experience, we proceeded to perform s-POEM for cases, such as epiphrenic diverticulum with achalasia and esophagogastric junction outflow obstruction[21], which were, without exception,effective in ameliorating symptoms and clearing remnant food from the diverticulum(Figure 1). Therefore, s-POEM could be a promising treatment alternative for epiphrenic diverticulum[22,23]. Diverticular peroral endoscopic myotomy (D-POEM),which is a septotomy of the diverticulum using the POEM technique, has also been reported to be effective[24]. The procedure involves exposing the septal wall after creation of a submucosal tunnel.
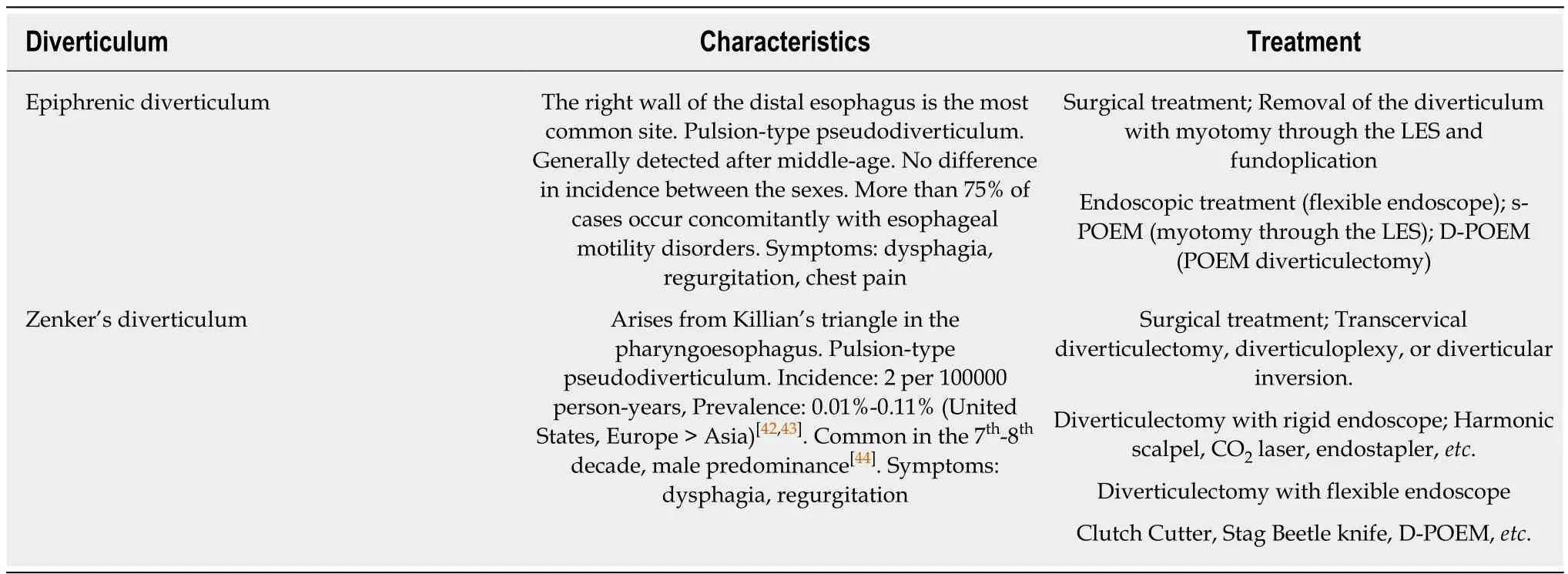
Table 1 Summary of the characteristics of epiphrenic and Zenker's diverticula and their treatment options
Iatrogenic diverticulum
The development and adoption of minimally invasive endoscopic treatments, such as POEM have led to reports of iatrogenic diverticulum (Figure 2A)[25,26], although it has not been recognized as a major problem in POEM[27,28]. Based on our experience with epiphrenic diverticula, the right wall of the distal esophagus is anatomically vulnerable and predisposed to diverticulum formation. Furthermore, remnant abnormal contractions of the esophageal body post-POEM (Figure 2B) exert significant pressure on the weak wall of the distal esophagus. Thus, clinicians need to take extra care when using POEM in esophageal motility disorders, such as jackhammer esophagus(hypercontractile esophagus) or type II (with pan-esophageal pressurization) and III(with spastic pressurization in the distal esophagus) achalasia. A pre-procedural HRM examination is essential to the decision-making process. A long myotomy that targets the esophageal body contraction as well, or a posterior myotomy that avoids the weak segments of the esophagus may prevent post-POEM diverticulum formation (Figure 2C).
ZD
Pathophysiology of ZD
ZD is also called pharyngoesophageal diverticulum or pharyngeal pouch (Figure 3A and B). As the synonyms suggest, ZD is an acquired pulsion-type pseudodiverticulum in the pharyngoesophagus. Increased intraluminal pressure leads to posterior outpouching between two strong pharyngoesophageal muscles: the cricopharyngeus and inferior pharyngeal constrictor. This area has a decreased hypopharyngeal wall tone and increased intraluminal pressure can present with posterior pouch formation. The location with the anatomical weakness is known as the Killian's triangle[29].
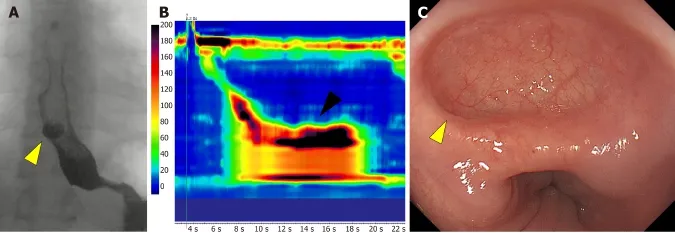
Figure 2 A case of iatrogenic diverticulum after peroral endoscopic myotomy. A: An iatrogenic diverticulum (yellow triangle) is visible on the anterior right wall in the lower esophagus on barium swallow; B: Hypercontractions on high resolution manometry persisted after peroral endoscopic myotomy, causing pulsion of the esophageal wall; C: Endoscopic view of the iatrogenic diverticulum of the esophagus that developed on the side where peroral endoscopic myotomy was performed,which lacks a muscle layer.
ZD is a rare condition with a yearly incidence rate of 2 per 100000 adults. Geographical variation in the incidence has been observed with a significantly lower incidence in Asian than in Western countries[30]. It occurs predominantly in men, and is most common in the seventh and eight decades of life (Table 1)[31].
Treatment of ZD
Several surgical options are available for the management of ZD. Diverticulectomy,diverticulopexy, diverticular inversion with or without myotomy, and myotomy alone have been reported[32]. Conventionally, an open left cervical incision under general anesthesia has been employed. However, as mentioned above, symptoms of ZD generally appear in the seventh and- eight decades of life, debilitating the patients and leading to increased surgical morbidity and mortality rates. Thus, minimally invasive endoscopic approaches have gained popularity in the recent years[33].
Endoscopic treatment generally involves diverticulectomy, using several devices originally developed for endoscopic submucosal dissection, and the POEM technique.The septal wall is dissected using a rigid endoscope with a CO2laser or endostapler,while a flexible endoscope uses devices such as a stag beetle knife and clutch cutter knife. Two approaches to the dissection have been reported: direct incision of the septal wall along with the mucosa using the rigid or flexible endoscope[34](Figure 3C),or myotomy of the exposed septal wall using the POEM technique with a flexible endoscope (D-POEM)[33]. Yuanet al[32]reviewed their entire experience from 1990 to 2011 and reported that the overall morbidity and mortality rates for the endoscopic approach were 8.7% and 0.2%, respectively, while they were 10.5% and 0.6%, respectively for open surgery. Studies on endoscopic treatment and open surgery for ZD performed from 1990 to 2002 also found that the endoscopic stapling technique was associated with lower major complications and mortality rates than open surgery(2.6%vs11.8% and 0.3%vs1.6%, respectively). It is understandable that the endoscopic technique carries a lesser risk of nerve injury and wound infection due to the minimally invasive nature of the endoluminal approach[35]. In addition, the hospital costs for endoscopic treatment are slightly lower than those for open surgery[36]. The recurrence rate varies from 0% to 35%[37-39].
ROKITANSKY DIVERTICULUM
Classically, diverticula of the middle esophagus were classified as Rokitansky diverticula, which generally occur in the thoracic esophagus. They are formed by cicatricial contraction due to a chronic inflammatory and fibrotic state that draws the wall of the esophagus outward; therefore, they involve the entire wall of the esophagus (true diverticulum). The apex of the pouch is generally located at a higher point than its entry point; therefore, it rarely attains an appreciable size or produces any symptoms. Their association with pulmonary tuberculosis is well characterized[40,41]. Cases of uncontrolled pulmonary tuberculosis are rare in the current era;therefore, Rokitansky diverticula presenting with clinical problems are even rarer.
Pulsion-type diverticula in the middle esophagus should be treated similarly to epiphrenic diverticula.
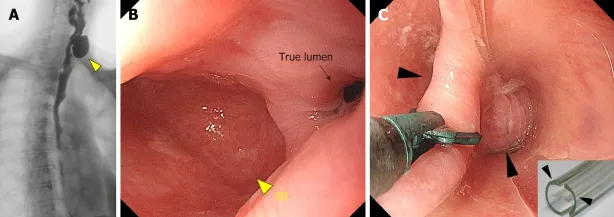
Figure 3 Zenker's diverticulum treated using endoscopic diverticulectomy. A: Zenker's diverticulum (ZD, yellow triangle) visible on a barium swallow; B: On endoscopy, the ZD (yellow triangle) is easily visible and is bigger than the true esophageal lumen (black arrow); C: Endoscopic diverticulectomy is performed with a diverticuloscope (insert) straddled across the septum, with one flap inserted into the bottom of the ZD and the other in the esophageal lumen (black arrow) for a clear visualization of the septum and safe diverticulectomy[34]. ZD: Zenker's diverticulum.
CONCLUSION
At present, the relative proportion of pulsion-type esophageal diverticula (epiphrenic and ZD) is increasing, while that of the traction-type (Rokitansky) is decreasing.Minimally invasive endoscopic treatment is indicated for pulsion-type diverticula and is being increasingly adopted owing to lower complication rates and equivalent efficacy to surgery. However, no randomized controlled trials comparing the difference between endoscopic treatment and surgery, or among the different endoscopic techniques have been performed. Furthermore, such studies of long-term follow-up results, including esophageal motility outcomes, are required to decide the best intervention modality for esophageal diverticulum. Another issue is the risk of esophageal carcinoma in the remnant diverticulum. Although the absolute risk of esophageal carcinoma is rather low, surveillance endoscopy is necessary after treatment. Minimally invasive endoscopic treatment should be performed after careful consideration of its advantages and drawbacks.
杂志排行
World Journal of Gastroenterology的其它文章
- International consensus statement on robotic hepatectomy surgery in 2018
- Growing burden of alcoholic liver disease in China: A review
- Gut microbiota profile in healthy Indonesians
- Ursodeoxycholic acid ameliorates hepatic lipid metabolism in LO2 cells by regulating the AKT/mTOR/SREBP-1 signaling pathway
- Risk factors for local recurrence and appropriate surveillance interval after endoscopic resection
- Accuracy of multi-echo Dixon sequence in quantification of hepatic steatosis in Chinese children and adolescents
