Changing trends in the mortality rate at 1-year post hip fracture - a systematic review
2019-03-21ColumDowneyMartinKellyJohnQuinlan
Colum Downey, Martin Kelly, John F Quinlan
Abstract BACKGROUND Traditionally, the mortality rate at 1-year post hip fracture was quoted as approximately 30% of all hip fractures. There have been recent improvements in hip fracture care in the main driven by national hip fracture registries with reductions in 30-d mortality rates reported.AIM To address recent 1-year post hip fracture mortality rates in the literature.METHODS Systematic literature review, national hip fracture registries/databases, local studies on hip fracture mortality, 5 years limitation (2013-2017), cohorts > 100,studies in English. Outcome measure: Mortality rate at 1-year post hip fracture.RESULTS Recent 1-year mortality rates were reviewed using the literature from 8 National Registries and 36 different countries. Recently published 1-year mortality rates appear lower than traditional figures and may represent a downward trend.CONCLUSION There appears to be a consistent worldwide reduction in mortality at 1-year post hip fracture compared to previously published research. Globally, those which suffer hip fractures may currently be benefiting from the results of approximately 30 years of national registries, rigorous audit processes and international collaboration. The previously quoted mortality rates of 10% at 1-mo and 30% at 1-year may be outdated.
Key words: Hip fracture; Mortality; Registries; Databases
INTRODUCTION
Hip fracture care continues to improve secondary to international audit and optimization of hip fracture management. Hip fractures are exceedingly common presentations to global emergency departments with approximately 3600 in Ireland per year[1], approximately 65000 in the United Kingdom[2], approximately 620000 in the European Union[3], approximately 300000 in the United States[4]and roughly 2 million worldwide[5]. This global figure is modest projected to increase threefold by 2050[6].
There is significant cost associated with hip fractures regarding: (A) financial cost to the health service providing care; and (B) morbidity and mortality cost to the patient.Recent research estimates the year 1 hospital cost secondary to an index hip fracture to be £14000 (€15900/$18750) per patient[7]. The annual cost of treatment in the European Union and the United States has been recently reported as €32 billion and$20 billion respectively[8].
The literature describes that after suffering a hip fracture, the patient will experience a reduction in overall functional status, social independence, mobility and increasing scores in depressive symptoms[9-10]. Due to the high prevalence of hip fractures and the disadvantage to both the patient and the local health service responsible for care, optimisation and the standardisation of hip fracture management has been targeted to reduce morbidity, mortality and financial expense. This optimisation and standardization, in the form of a national registry, has been shown previously to improve the quality of care and outcomes of hip fracture patients[11].
The earliest hip fracture registry established is “RIKSHÖFT”, the Swedish national hip fracture registry, set up in 1988, following on from the successful local implementation of national knee and hip arthroplasty registers in the 1970s[12]. In 1993,the Scottish Hip Fracture Audit (SHFA) implemented a registry that reported annually until 2008, after which, the audit was stepped down to capture “snapshot”data only. Following audit and the recognition of deterioration in outcomes post step down[13], the SHFA was re-implemented in May 2016 and year round data collection was re-instituted[14]. In 1995, the European Commission funded the initiation of the Standardised Audit of Hip Fracture in Europe due to the triumphs in outcomes secondary to the “RIKSHÖFT” audit in Sweden[15]. The Danish orthopaedic community established the Danish Hip Fracture Database in 2003[5]whilst the Norwegian community set up their database, the “NOREPOS”, in 2005[16].
In 2007, an important milestone was reached regarding the initiation of the largest and fastest growing national hip fracture registry by the United Kingdom. After publishing the “Blue Book”, which set quality standards established by the British Orthopaedic Association and the British Geriatrics Society, the National Hip Fracture Database (NFHD) began to collect and publish data annually regarding hip fractures[3]. In 2010, a European Union program, named euroHOPE (Healthcare Outcomes, Performance, Efficiency), was created to compare healthcare performance regarding hip fracture treatment across 7 European countries[17]. The fragility fracture network was then established in 2011, a global network, with a mission to optimize the multidisciplinary management of patients with fragility fracture globally and prevent secondary fracture[18]. This was followed by the foundation of the Irish Hip Fracture Database in 2012[1]and more recently the Australian and New Zealand Hip Fracture Registries in 2016[19]. Several countries are currently piloting their own national hip registries following the achievements published by the registries described above including Greece, Malta, Nederlands, Slovenia, Spain, Lebanon and Argentina.
Traditionally, orthopaedic trainees are taught that the mortality rates in this fragile population were approximately 10% at 30 d and approximately 30% at 1 year[20]. These figures are important at: (A) a patient level with regards to family discussions surrounding realistic expectations and prognosis following hip fracture; and (B) at a hospital and national level with regards to the optimisation of care and distribution of finite resources.
In 2015, following a review of 471590 patients which suffered a hip fracture in the United Kingdom between 2003-2011, it was concluded that “the launch of a national clinician-led audit initiative was associated with substantial improvements in care and survival of older people”[21]. This group reported significant reductions in 30-d mortality.
Following review of the recent literature emanating from the national registries, it was noted that whilst 87.5% of the national registries publish annual data on inpatient mortality and 62.5% publish annually on 30-d mortality, only 12.5% (1 registry) published mortality rate at 1-year post hip fracture. In order to explore whether there have been any recent global reductions in 1-year mortality post fracture, a systematic literature review was undertaken.
MATERIALS AND METHODS
A review of the available literature on (A) national hip fracture registries/databases and (B) local hip fracture studies which included 1-year mortality data was conducted using Pubmed and Google Scholar. The following keywords were used: “hip fracture”, “mortality”, “year”, “death”, “outcomes”, “registry”, “registries”,“database” and “databases”. The inclusion criteria were those studies published within the last 5 years (2013-2017), studies including a cohort > 100 and those in the English language. The most recent national registry reports were obtained and personal contact to authors of the Swedish and Danish reports via e-mail was required as these are reported in local language only.
RESULTS
National Registries
Table 1 lists the countries, registry names, foundation year, age inclusion criteria,recent annual reports with reference and the mortality data published by each of the 8 national databases. 87.5% of the registries have an age inclusion criteria of 50 years or more. The table shows a dearth in published data for 1-year mortality rates post hip fracture.
Europe
Recent (previous 5 years) 1-year mortality research data from the European continent was extracted from the literature and is summarised in Table 2. There were 22 articles reviewed with a mean 1-year mortality of 23.3% [standard deviation (SD) 6.3%,median 23.4%] reported. The lowest figure was 9.7% with the highest 34.8%. 19 of the 22 articles (86%) reported data regarding cohort numbers ranging from 124 to 31668 patients included (median 444, mean 6902, SD 11804). 91% reported age related inclusion criteria, with 55% including > 60 years only and the remaining 45%including patients < 60 years old. 82% of the articles were published within the period 2015-2017.
Asia
One year mortality data (2013-2017) from the Asian continent was extracted from the literature and is summarised in Table 3. There were 10 articles reviewed with a mean 1-year mortality of 17.89% (SD 8.7%, median 18.9%) reported in studies selected. The lowest figure was 2.4% with the highest 30.4%. All of the articles reported data regarding cohort numbers, which ranged from 110 to 43830 patients included (median 400, mean 5621, SD 13566). 90% reported age related inclusion criteria, with 67%including > 60 years only and the remaining 33% including patients < 60 years old.70% of the articles were published in the year 2017 with 90% published within 2015-2017.
Oceania
Table 4 lists the results from a large study undertaken in New South Wales, Australia which published a 1-year mortality rate post hip fracture of 24.9%. This study included 27888 patients which were aged > 60 years. To the best of the author’s knowledge, there were no recent local studies emanating from New Zealandregarding mortality post hip fracture.
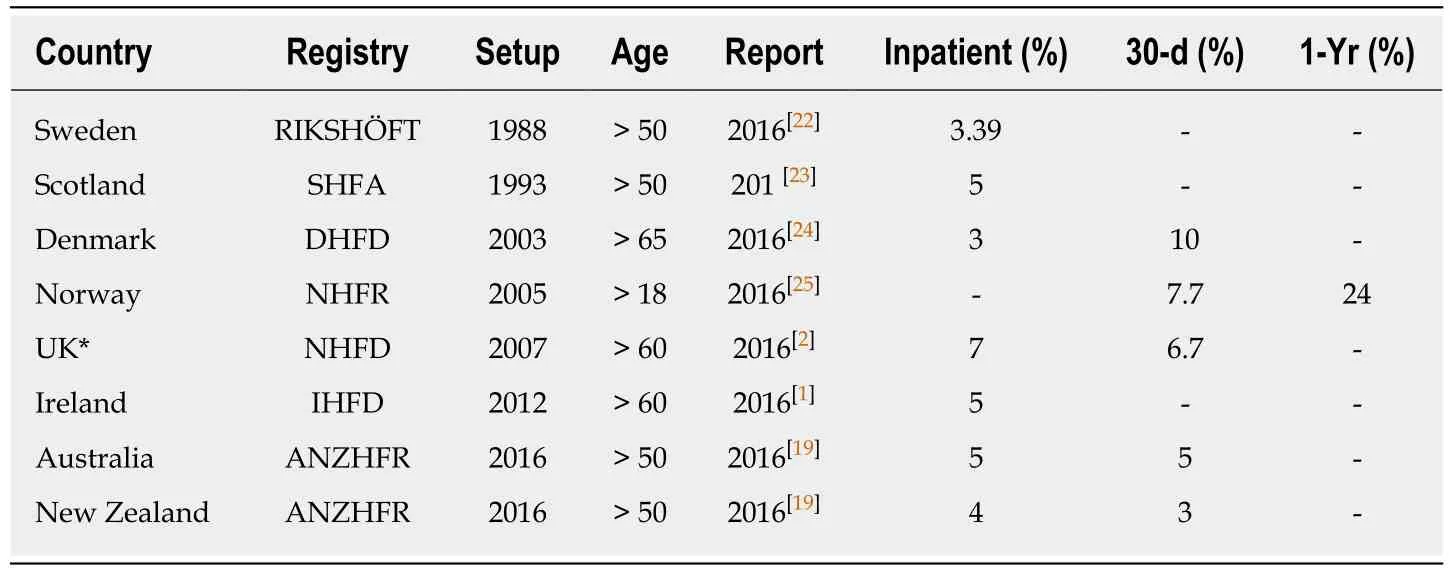
Table 1 Data from the National Registries
North America
Table 5 lists the results from a large study undertaken in the United States using the Kaiser Permanente database. This recent publication describes a 1-year mortality rate post hip fracture of 21%. This study included 14294 patients which were aged > 60 years. To the best of the author’s knowledge, there were no recent local studies published from Canada regarding 1-year mortality post hip fracture.
South America
One year mortality data from the South American continent was extracted from the literature and is summarised in Table 6. There were 2 articles reviewed with a mean 1-year mortality of 26.8% (SD 4.5%). The articles included small cohorts with 100 and 213 patients respectively. Both of the studies included patients > 65 only.
Africa
There has been no research regarding hip fracture mortality published throughout the African continent during the past 5 years to the best of the authors’ knowledge.
Global overview
Overall, local hip fracture related studies from 36 different countries were reviewed with regards to 1-year mortality rates post hip fracture. The mean overall 1-year mortality rate was 22.0% (SD 7.2%, median 22.8%) with a range from 2.4%-34.8%. A combined total of 229851 patients were included, with a range of 100-43830 patients from the smallest and largest cohort respectively. The median cohort was 402 patients.61% of the studies involved a cohort between 100-1000 patients, with 18% between 1001-10000 and the remaining 21% including more than 10001 patients. 58.3% of the studies included patients > 60 years only, with 33.3% including patients < 60 also with a small proportion not declaring age inclusion/exclusion criteria. Using studies which included patients > 60 years only (n = 21/36) may result in a more accurate representation of fragility hip fracture cohorts, however the results were quite similar with a mean rate of 21.8% (SD 7.6%, median 23.6%) mortality 1-year post hip fracture.83.3% of the local studies research included in this study was published in the years 2015-2017.
DISCUSSION
The mortality at 1 year post hip fracture has traditionally been reported as 30%[20]and more recently described as “around a third within a year”[60], whilst the 2017 NFHD annual report suggests “up to a third die within a year following a hip fracture”[2].There have been significant developments with regards to data collection in the areas of casemix, surgical/anaesthetic practice, process and outcomes of hip fracture care by the national registries. However, only 1 of the 8 national registries is publishing data regarding mortality at 1-year post hip fracture. There is therefore a void in the published literature on this topic.
After reviewing the recent hip fracture related mortality literature, it was found that the mean 1-year mortality rate in Europe was 23.3% (22 studies), whilst in Asiawas 17.9% (10 studies). The figures for the United States and Australia were 21% and 24.9% respectively. The figure in South America was 26.8%, however, this originated from small studies. On analysis of data from all 36 studies (n = 229851 patients), the mean 1-year global mortality rate was 22% (SD 7.2%, median 22.8%).
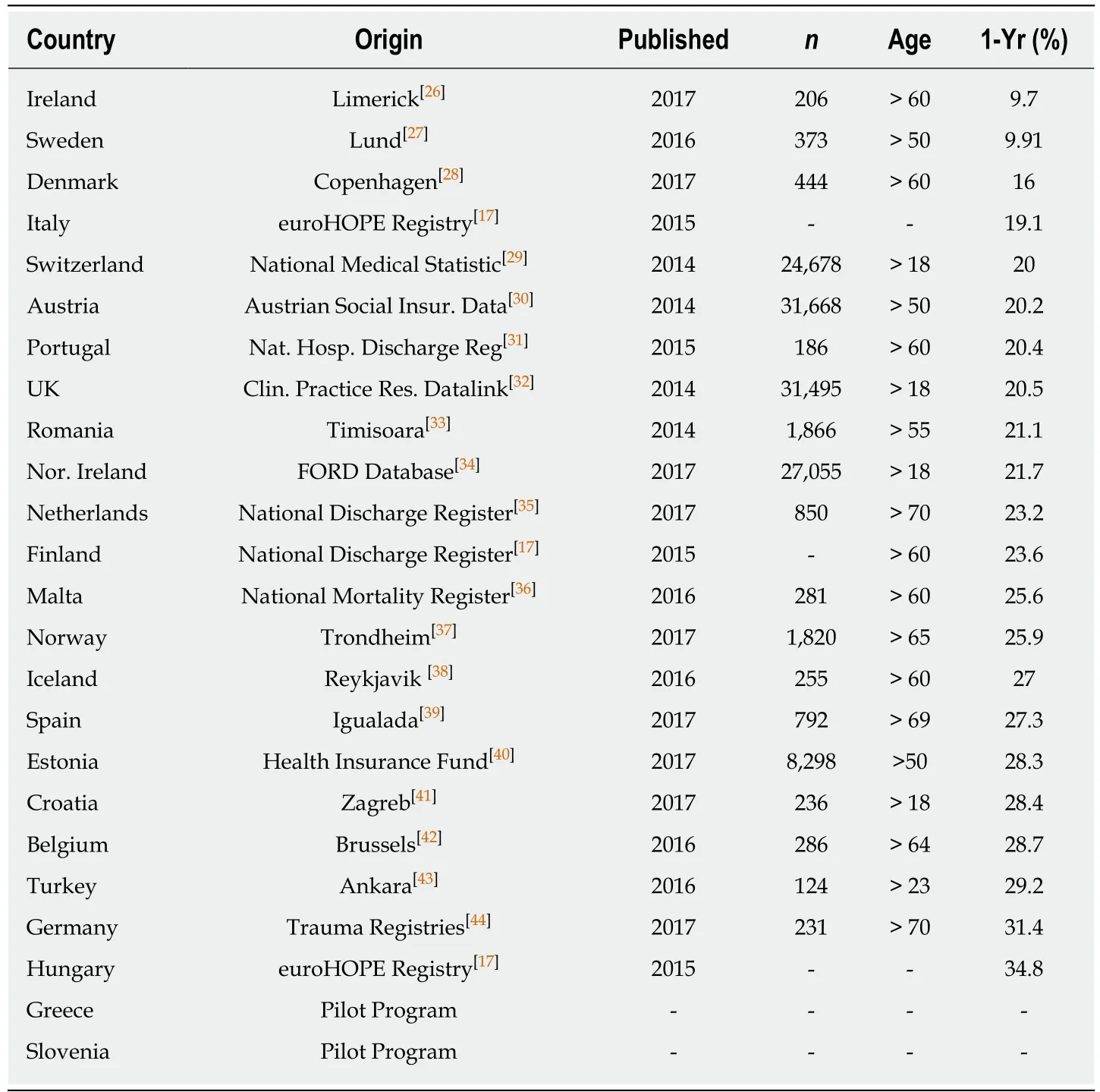
Table 2 Data from local hip fracture studies in Europe
These results are at odds with those reported previously and may suggest a consistent global improvement in longer-term survival following hip fracture. Best practice guidelines have been developed by way of continuous optimization through the auditing process of the national registries and continue to be developed, refined or discarded based on continuous audit cycle. The improvement in longer term survival post hip fracture may be secondary to worldwide adoption of current best practice in the care and secondary prevention of hip fracture.
This is the first study that has reviewed recent worldwide-published data on 1-year mortality rates including data collected from 229851 patients. Although the literature review included studies within the last 5 years, it is worth noting that the vast majority (83%) of the local studies (30/36) were published within the last 3 years(2015-2017). It is also worth noting that the most recent papers on this topic(published in 2018) confirm that the changing trend in 1-year mortality continues to be observed[61-63]. Cancio et al[64]this year published a 1-year mortality rate of 22% for a large hip fracture cohort (n = 30552), which is similar to our findings described above.
Whilst this article reports a decreasing trend in mortality at 1-year post hip fracture,it is important to recognize limitations of this study. A potential source of error is the use of data from all 36 studies to ascertain a mean mortality rate as some of the studies included patients < 60 years of age. However, limiting the inclusion criteria to those studies that include patients > 60 years only, the mortality rate is 21.8% (SD 7.6%, median 23.6%) which is a similar finding. Another limitation is equal weighting to mortality rates despite wide variation in cohort numbers. Limiting the inclusion criteria to those studies which include > 10001 patients only (n = 7), the mean mortality rate is 20.7% (SD 2.4%, median 20.5%) which also is a similar finding.
It is also worth noting that as an index hip fracture outcome measure, mortality is an imperfect quality indicator and is affected by both patient age and casemix(multiple comorbidities typically). Therefore, it is the trend in mortality rate data over time that is more useful as a quality indicator.
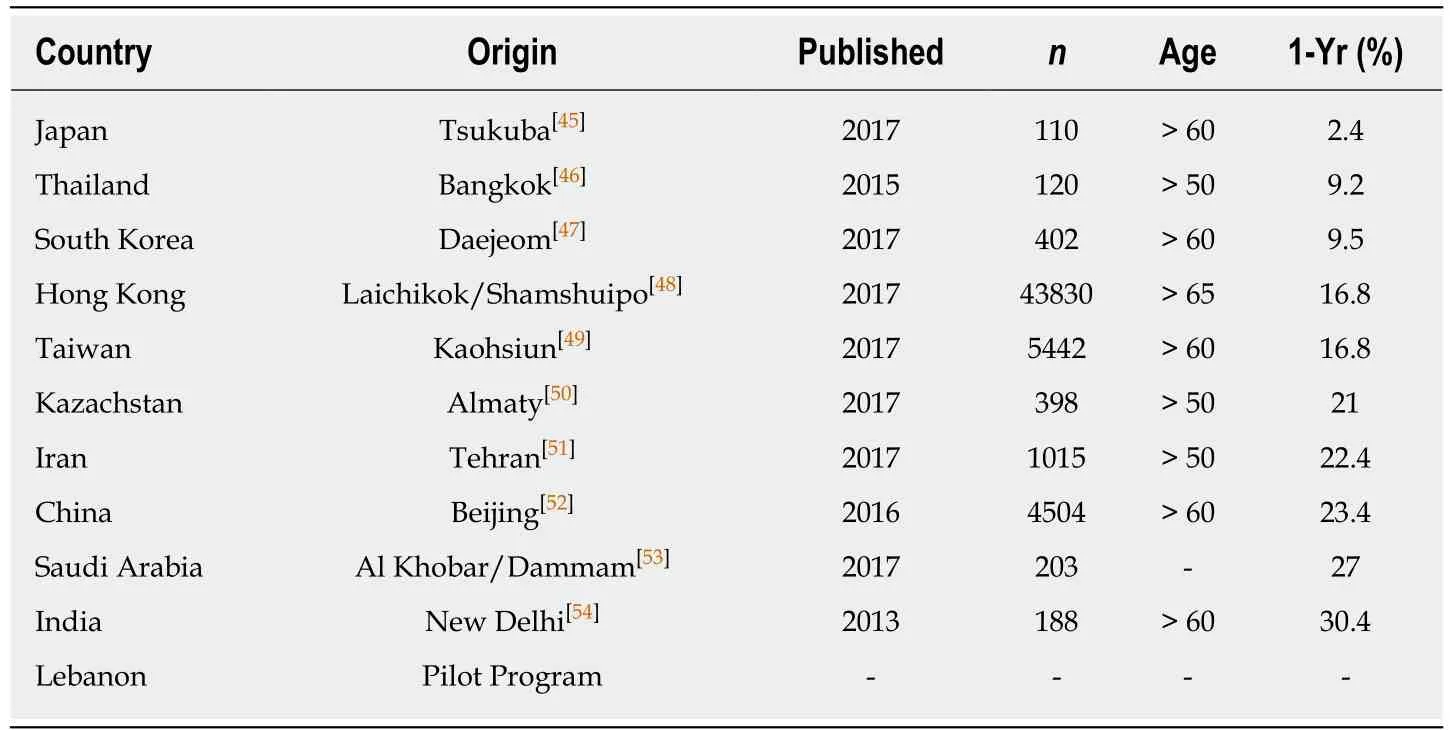
Table 3 Data from local hip fracture studies in Asia
Osteoporosis currently causes approximately 9 million fractures annually around the world[65]. As alluded to in the introduction, hip fractures are increasing with excess of 6 million per year predicted in 2050. The greatest increases are expected in Asia[66].The World Health Organisation predicts that between 2000 and 2050, the proportion of those aged > 60 will double in numbers from 11 to 22% or 605 million to 2 billion people[67]. It is important that this expected rise is planned for and this literature review suggests that as a global orthopaedic and orthogeriatric community, vast strides are being made in the optimisation of care with hip fracture patients to mitigate for the impending surge in hip fracture incidence. The reduction in 1-year mortality provides feedback that following adoption of hip fracture management standards of care, it is not simply improvements in early mortality with deferral of mortality outside of the acute window (30 d) but longer-term survival at 1-year post hip fracture. The United Kingdom National Hip Fracture Database website publishes monthly on overall performance measures including national average 30-d mortality.The most recent figure was 5.7% (July, 2018)[68]with almost month-to-month reductions since initially published in April 2012. These findings are very positive.Another recent positive development in hip fracture care is the increasing involvement of orthogeriatricians in the care of these fragile patients and their corresponding impact on mortality reduction[60].
The data collected by the national registries allow us as a community to tackle a complex international problem to minimise morbidity, mortality and costs associated with hip fractures. These registries continue to be optimised and it has been recently suggested that (1) simplicity; (2) continuous collection of all cases as routine practice;(3) definition of variables collected; and (4) a common set of variables collected will fulfil the criteria of a model registry which should allow direct national and international comparison and further improvements in care delivered[3].
In conclusion, globally, those which suffer hip fractures may currently be benefiting from 30 years of national registries, rigorous audit processes and international collaboration. This literature review suggests a decrease in trends in mortality at 1-year post hip fracture compared to previous research on this topic. Further improvements in hip fracture care quality indicators are expected by the authors in light of increased involvement of the orthogeriatric subspeciality and the continuous refinement process of the national registries. The results of 7 novel national pilot registries are anticipated.
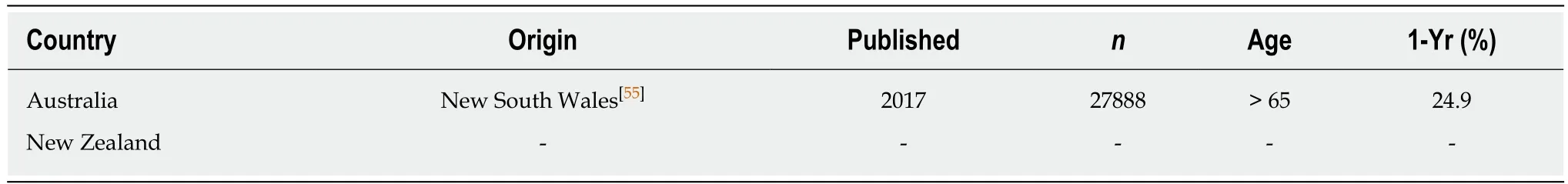
Table 4 Data from local hip fracture studies in Oceania
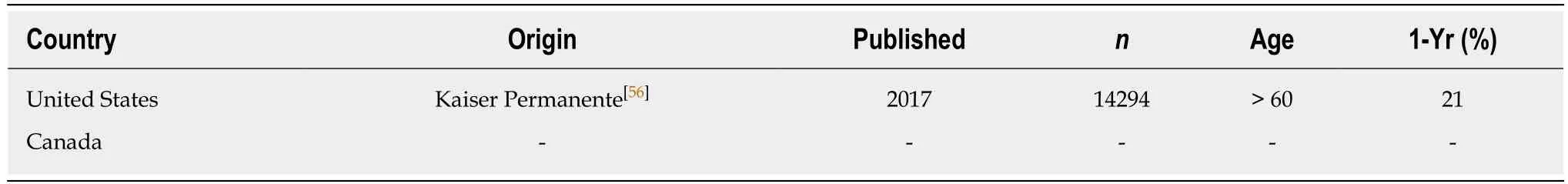
Table 5 Data from local hip fracture studies in North America
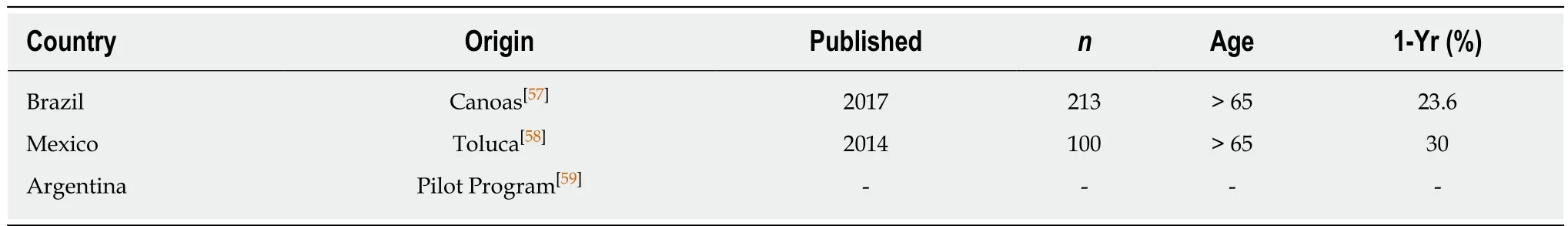
Table 6 Data from local hip fracture studies in South America
ARTICLE HIGHLIGHTS
Research background
Hip fracture audit is increasing globally with 8 countries producing national reports annually and several countries currently piloting hip fracture audit schemes. Hip fracture audit has been shown to result in improvements in care and survival of older people. Short-term mortality rates(in-patient and 30-d) are published by the majority of national registries and there is evidence that short term mortality rates are decreasing. The 1-year mortality rate post hip fracture is currently recognized as approximately 30%. Recent longer-term (1-year) mortality information is lacking in the literature.
Research motivation
Our research group believes there may also be a changing trend (decreasing) in 1-year mortality post hip fracture. Knowledge of a more current, up-to-date figure will lead to a more informed discussion with family of those affected and optimization of care of this fragile cohort at hospital and national levels.
Research objectives
To determine the current 1-year mortality rate post hip fracture.
Research methods
Systematic literature review. The following keywords were used: “hip fracture”, “mortality”,“year”, “death”, “outcomes”, “registry”, “registries”, “database” and “databases” (PubMed and Google Scholar). The inclusion criteria were those studies published within the last 5 years (2013-2017), studies including a cohort >100 and those in the English language.
Research results
Data from 8 national registries and 36 countries (6 continents) were reviewed. Recently published 1-year mortality rates appear lower than traditional figures and suggest a downward trend.
Research conclusions
The previously quoted 1-year mortality rate of approximately 30% appears to be outdated. A figure of 22% is a more accurate, up-to-date figure for 1-year mortality rate post hip fracture.
Research perspectives
This research provides a more current, up-to-date figure for 1-year mortality rate post hip fracture.
杂志排行
World Journal of Orthopedics的其它文章
- Aetiology of Legg-Calvé-Perthes disease: A systematic review
- Comparison of implant related complications amongst patients with opioid use disorder and non-users following total knee arthroplasty
- Short-term differences in anterior knee pain and clinical outcomes between rotating and fixed platform posterior stabilized total knee arthroplasty with a new femoral component design
- Linkage of microbiota and osteoporosis: A mini literature review