Comparison of implant related complications amongst patients with opioid use disorder and non-users following total knee arthroplasty
2019-03-21RushabhVakhariaKarimSabehAjitVakhariaDhanurDamodarTsunYeeLawMartinRoche
Rushabh M Vakharia, Karim G Sabeh, Ajit M Vakharia, Dhanur M Damodar, Tsun Yee Law, Martin W Roche
Abstract BACKGROUND The influence of opioid use disorder on implant related complications, infection and readmission rates, and total global episode-of-care costs following primary total knee arthroplasty (TKA) is limited.AIM To examine whether opioid abuse in patients undergoing primary TKA.METHODS A retrospective analysis of the Medicare dataset, using the PearlDiver database,from 2005-2014 comparing outcomes in patients with opioid abusers (OUD) to non-opioid abusers (NOU) undergoing primary TKA was performed. Patient outcomes were analyzed including implant complications, readmission rates, and day-of-surgery and 90-d cost. Statistical analysis was performed with R(University of Auckland, New Zealand) calculating odds-ratio (OR) along with their respective 95% confidence interval (95%CI) and P-values.RESULTS The OUD group was at greater odds of having implant related complications overall (20.84% vs 11.25%; OR: 2.07; 95%CI: 1.93-2.23; P < 0.001). Revision (OR:2.07; 95%CI: 1.11-3.84; P < 0.001), infection (OR: 1.92; 95%CI: 1.72-2.18; P < 0.001),periprosthetic fractures (OR: 1.83; 95%CI: 1.16-4.79; P < 0.001), and 90-d readmission rates (OR: 1.47, 95%CI: 1.35-1.61, P < 0.001) were also significantly increased. OUD patients also incurred in higher day-of-surgery and total global 90-d episode-of-care costs compared to NOU.CONCLUSION Patients with OUD show an increased risk of complications compared to the nonopioid users group. Appropriate recognition, pre-surgical optimization, and patient education are essential to mitigate these complications and improve patient outcome.
Key words: Opioid use; Total knee arthroplasty; Medicare; Database; Cost; Readmission rates
INTRODUCTION
Patients with osteoarthritis of the knee can manifest with symptoms such as pain and reduced range of motion, negatively impacting the patient’s quality of life[1]. Total knee arthroplasty (TKA) is the treatments of choice when conservative therapy has failed for patients suffering from osteoarthritis of the knee[2,3]. Recent studies have shown that there has been an increase in the number of TKA procedures performed in the United States and is expected to grow exponentially[4]. Minimizing postoperative complications and improving patient-reported outcome measurements (PROMs) is important for patients undergoing these procedures[5]. Preoperative optimization, by identifying risk factors associated with adverse events and worse clinical outcomes,has been shown to directly impact postoperative complications and PROMs[6-9].
Currently, Orthopedic Surgeons are the third highest prescriber of opioids following Internists and Dentists[10,11]. Morris et al[11]and Dufour et al[12]have illustrated an increasing trend in the number of opioids prescribed by providers and the incidence of opioid abuse or dependency diagnosis in the community. Blazer and Wu[13]reported that 1.4% of adults above the age of 50 consume opioids for recreational use. This finding was greater than the use of sedatives, tranquilizers, and stimulants, all of which were less than 1%[13]. In addition to providing an analgesic affect, opioids are known to directly impact endocrine, immune, gastrointestinal and musculoskeletal systems[14]. The influence of opioid use disorder on implant related complications, infection and readmission rates, and total global episode-of-care costs following primary TKA is limited.
The aim of the study was to analyze and compare rates of implant complications,90-d infection rates, 90-d readmission rates, and hospitalization cost among opioid abusers (OUD) and non-opioid abusers (NOU) undergoing primary TKA. We hypothesize that following primary TKA, opioid abuse and dependency is associated with higher implant complications, infections, 90-d readmissions rates and higher episode-of-care costs compared to NOU.
MATERIALS AND METHODS
A retrospective review of the Medicare patient population from 2005-2014 within the PearlDiver (Pearl Diver Technologies, Fort Wayne, IN) claims based database was performed. PearlDiver is a commercially available database which has been used extensively for orthopedic-related research. The database is compliant with the Health Insurance Portability and Affordability Act and holds the records of over 100 million patients. The database provides information on diagnosis, procedures, complications,and additional information such as demographics, region, discharge library, and length of stay (LOS).
Patients who underwent TKA were identified using International Classification of Disease, ninth revision (ICD-9) procedure code 81.54. Patients with a history of opioid use disorder and dependency were identified with ICD-9 diagnosis code 304.00-304.02 and 305.50-305.52. The inclusion criteria for the study group consisted of all patients in the database undergoing TKA and having a 90-d history and diagnosis of OUD on the same day of their index procedures. The control group consisted of all patients who underwent TKA and had no history of opioid abuse or dependency. Patients in the study group were randomly matched 1:1 to patients in the control group with respect to age, gender, and Elixhauser-Comorbidity Index (ECI). ECI was used as a marker to ensure that patients in the study group and control group were matched appropriately, as used in previous studies[15,16]. The authors decided to use ECI compared to the traditional Charlson-Comorbidity Index (CCI) as ECI as it includes 31 conditions, and demonstrates better predictions of mortality in patients with cardiac, pulmonary gastrointestinal, nephrology, hepatobiliary, and oncologic conditions[17]. Additionally, ECI also contains comorbidities such as hypertension,obesity, psychiatric disorders that are not found in CCI[18]. After the matching process two mutually exclusive cohorts were formed.
Implant related complications 2-years following the index procedure were analyzed and compared. ICD-9 coding was also used to determine implant and infection related complications (Table 1). Reimbursements were used as a marker for cost, as used in previous studies[16,19-21]. Ninety-days was chosen for infection related complications and readmission rates to be in accordance with the Comprehensive Care for Joint Replacement model design, stating that episode of care begins day of admission and ends 90-d following discharge[19,20].
Statistical analysis
Descriptive and statistical analysis was performed with the programming language R(University of Auckland, New Zealand) analyzing odds-ratios (OR) with their respective 95% confidence interval (95%CI), and P-value. Welch’s t-test was utilized to determine significance in reimbursement rates between the two cohorts. An alpha value less than 0.05 was considered statistically significant.
RESULTS
After appropriately matching the study group with the control group, there were 23072 (female = 15616; males = 7230; unknown = 226) OUD (n = 11536) and NOU (n =11536) to have undergone TKA (Table 2). Patients in the study group and control group undergoing primary TKA had an average ECI of 11.93 ± 4.31 (P = 1.00)indicated the two groups were matched appropriately and no statistical difference exists between the two groups.
Implant complications and LOS
OUD patients were found to have greater odds of implant related complications(20.84% vs 11.25%; OR: 2.07; 95%CI: 1.93-2.23; P < 0.001) compared to NOU within 2-years following the index procedure. Complications such as requiring a revision procedure (OR: 2.07, 95%CI: 1.11-3.84, P < 0.001), periprosthetic fracture (OR: 1.83,95%CI: 1.16-4.479, P < 0.001), dislocation of prosthetic joint (OR: 1.68, 95%CI: 1.37-2.05,P < 0.001), and mechanical loosening (OR: 1.33, 95%CI: 1.08-1.62, P < 0.001) were greater in the OUD group compared to NOU (Table 3). Odds of developing infections within 90-d were also higher in the OUD group (OR: 1.92; 95%CI: 1.70-2.18; P < 0.001)compared to controls (Table 3). In-hospital LOS was greater in OUD (3.44 d vs 3.32 d;P < 0.001) compared to NOU following primary TKA.
Readmission rates and reimbursements
Readmission rates within 90 d of primary TKA were higher in OUD compared to NOU (OR: 1.47, 95%CI: 1.35-1.61, P < 0.001). Cost analysis revealed that day-ofsurgery reimbursements ($14499.39 vs $14247.74; P < 0.001) were higher for OUD undergoing TKA compared to controls. Similarly, total global 90-d episode of care reimbursements were also higher ($18619.98 vs $16885.21; P < 0.001) in OUD compared to the NOU group (Table 4).
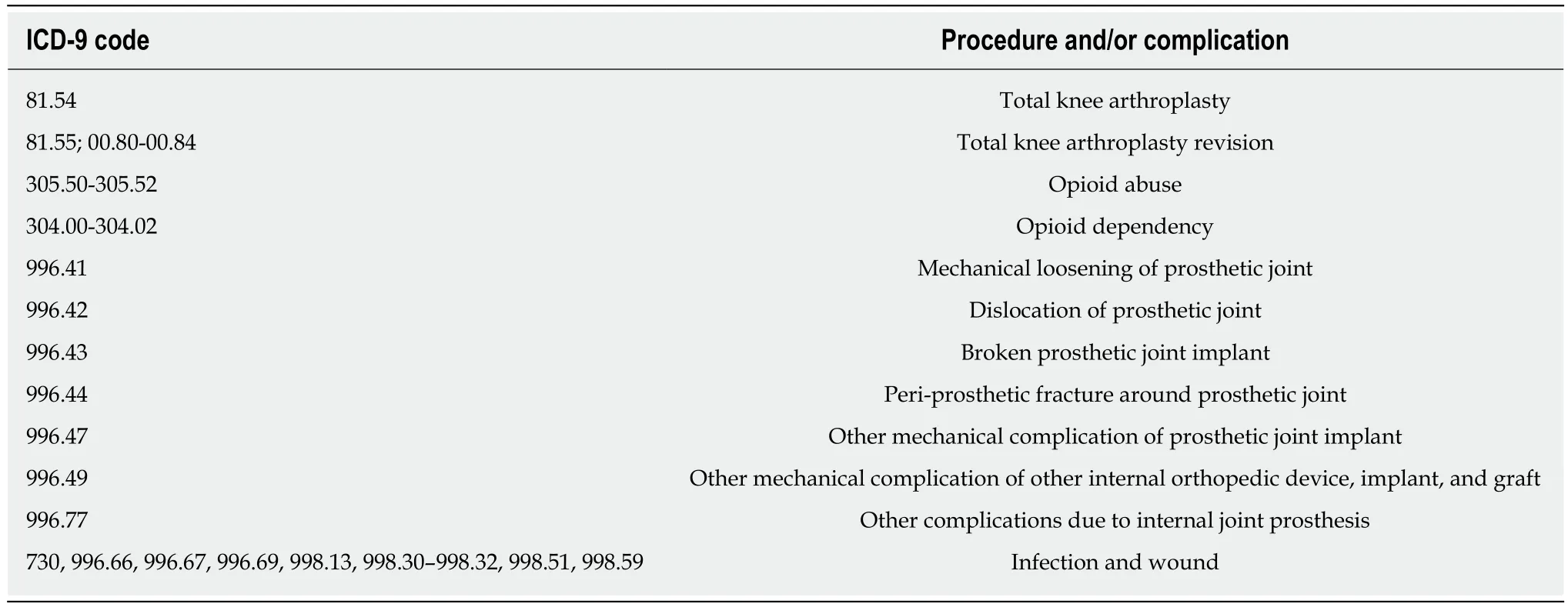
Table 1 List of ICD-9 procedure and complication codes used
DISCUSSION
Recent studies show an alarming increase in the overall rates of opioid abuse, misuse,and dependence in the United Sates-collectively termed: Opioid Use Disorder.Meanwhile, orthopaedic surgeons were found to be the third highest prescribers of opioid prescriptions amongst all providers[20-23]. These statistics place a significant number of our orthopaedic patients at risk of the detrimental effects of narcotics and potential for abuse. In the arthroplasty patient population, there remains limited evidence in the literature linking opioid abuse to post-operative complications and implant survivorship following primary THA and TKA. Our study demonstrates that patients with opioid use disorder are at a significantly higher risk for having shortterm implant related complications and failure such as periprosthetic fractures, along with increased risk of infections within 90 d of their primary procedure, longer lengths of stay, and greater odds for readmission within the first 90 d, all resulting in higher episode of care costs.
Similar to our results, Sing et al[24]found that 5.1% of their patients taking shortacting opioids and long-acting opioids prior to surgery subsequently went on to develop periprosthetic fractures following total hip and TKA, compared to 1.7% who were not taking opioids. Out of this population, 14.2% of patients required revision surgery. In their study, they found short and long-acting opioids to have a 4.42 and 6.15 times greater odds of developing postoperative complications following TKA,respectively[24]. Saunders et al[25]found similar results in elderly patients consuming opioids, where higher doses of opioids (> 50 mg/d) were associated with 2.00 increase risk of fractures.
Long term opiate use has shown to have negative effects on cognition and motor function as demonstrated by Kerr et al[26]who demonstrated that infusion of morphine to normal concentrations led to significant cognitive and motor impairments. The study found that the processing time of verbal instructions and ability to maintain force were increased and decreased, respectively[26]. Opioid use has shown to lead to development of dizziness and sedation affecting balance and proprioception, all leading to an increased risk for falls and therefore fractures[14]. Studies have shown that opioids impact the immune system negatively[27]. Animal studies demonstrate that opioids impair both adaptive and innate immunity, and increases susceptibility to many pathogens[27,28]. Furthermore, opioids increase production of corticosteroid production, amplifying the inflammatory state with proinflammatory cytokines[28,29].The effects of diminished bone mineralization, increased susceptibility to falls,alterations within the immune system may explain the increased rate of periprosthetic fractures, dislocation, mechanical loosening, prosthetic joint infections, and ultimately TKA revisions in the OUD group[14,26].
This study also showed that readmission rates 90-d following surgery was also significantly higher in the OUD group. The findings were consistent with an investigation by Mosher et al[30], where readmission rates where compared in occasional users, OUD, and non-abusers. OUD had greater 30-d readmission rates compared to non-abusers[30]. Our data is consistent with the findings in current literature. In addition, a large database study performed by Menendez et al[31]found patients with a history of opioid abuse and dependency undergoing elective orthopedic surgery had greater odds of prolonged hospitalization stays (OR: 2.5,95%CI: 2.4-2.5). Oderda et al[32]quantitatively found the average LOS in OUD and dependency increased by 10.3% (95%CI: 6.5-14.2, P < 0.001) compared to patients without a history of opioid abuse or dependency. Azar et al[33]found the average increase in LOS and amongst OUD undergoing primary orthopedic procedures was 0.52 d. In our study, patients in the study group had an average LOS of 12 d longer when undergoing primary TKA.
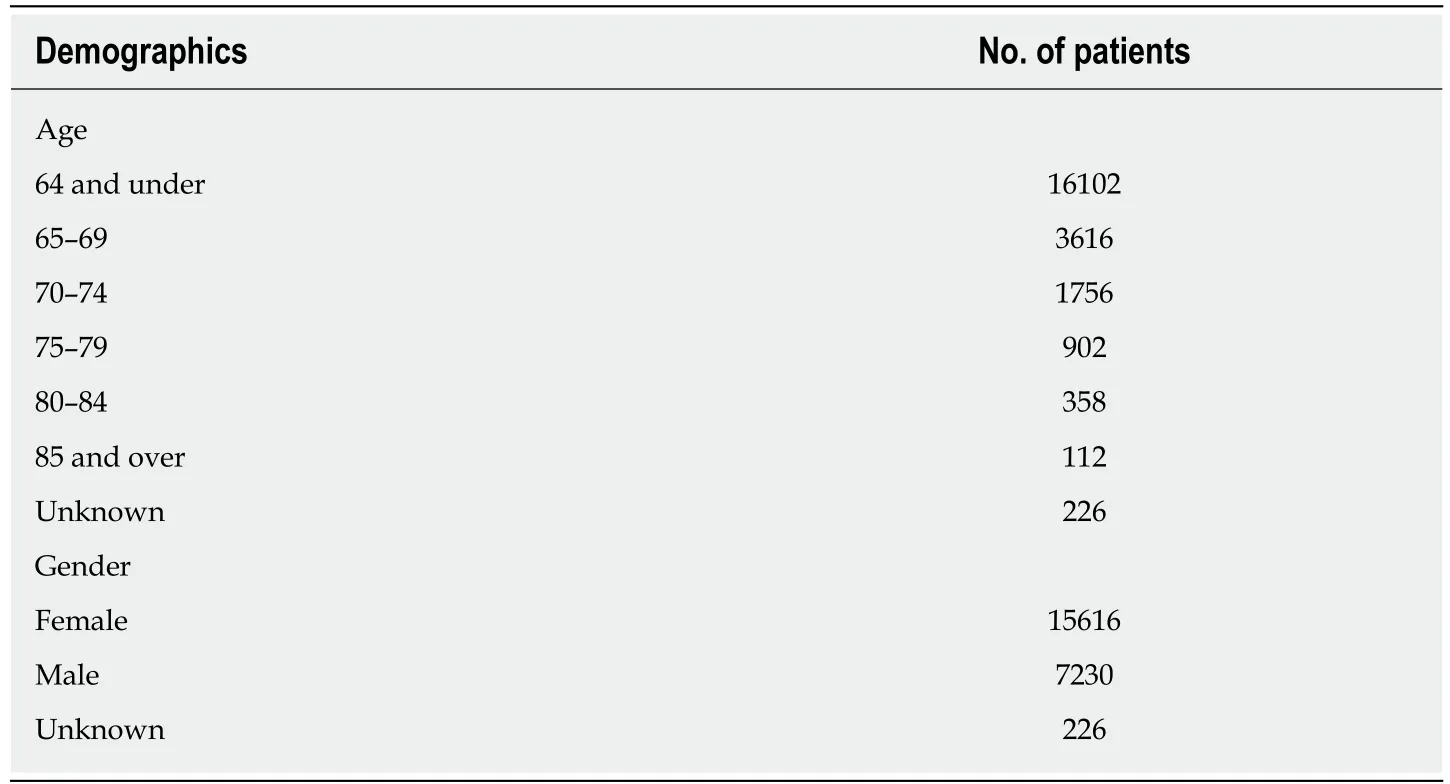
Table 2 Demographics of patient age and gender undergoing total knee arthroplasty after matching process
Improving patient outcome while reducing cost has been the main focus of the value-based care initiatives put forth by Center for Medicare and Medicaid Services.Our study, however, showed that the increased complication rate associated with opioid abuse translates into poorer patient outcome and increased cost of care. For example, the OUD group was found to have significantly higher day-of-surgery costs following primary TKA when compared to the control group. One study found that the approximate increase in costs for patients with a diagnosis of OUD was approximately 6% higher and another study calculated an increase of $861.50[34,35].Meyer et al[35]reported that OUD with private insurance had an average cost of care of$24193 in direct healthcare costs, in contrast to NOU who incurred only $3647 in healthcare costs. When comparing healthcare costs of OUD within the Medicaid provider, OUD incurred approximately $26724 in costs, compared to $11541 for patients in the matched control group.
While the study has its advantages of including a large sample size, database studies are not without limitations. Being a database analysis study, the validity of our analysis and results are reliant on accuracy of procedural coding within the database[36]. This translates to the fact that miscoding and noncoding by providers is a potential source of error. Currently, it is expected that 1.3% of coding errors are present within the Medicare population[37]. Secondly, only a single insurer’s data was included in our analysis, and may not represent a true cross section of the OUD group in the United States[37]. Additionally, the prevalence of comorbid conditions and adverse events may be underreported[36]. A selection bias may also be present as patients in the study may enter or exit the database as a natural manifestation[36].
In conclusion, the study demonstrates that patients with opioid use disorder undergoing primary TKA are at a greater risk for implant complications such as revision, infections, and periprosthetic fractures. They were also found to have a higher 90-d readmission rates, and incur in higher episode of care costs. The results of this study may improve a providers’ ability to preoperatively counsel patients regarding specific adverse events associated with opiate abuse and TKA and highlights the need to reduce narcotic prescriptions to our patients.
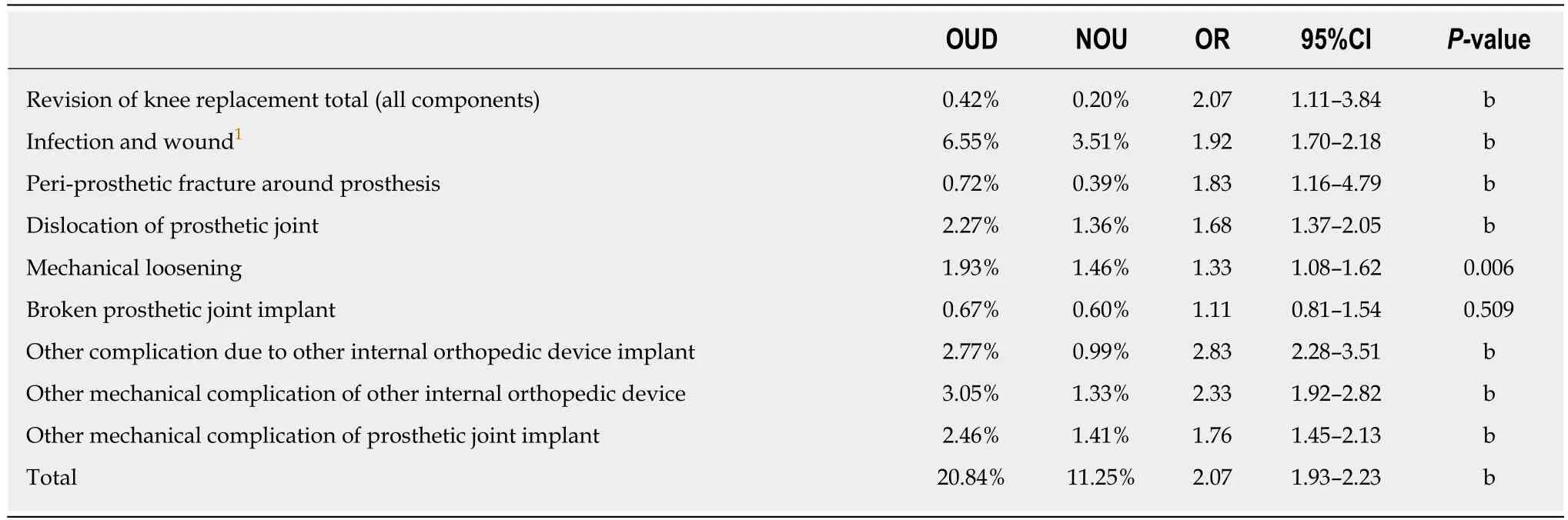
Table 3 Comparison of implant related complications 2-years following primary total knee arthroplasty in opioid abusers and non-opioid abusers
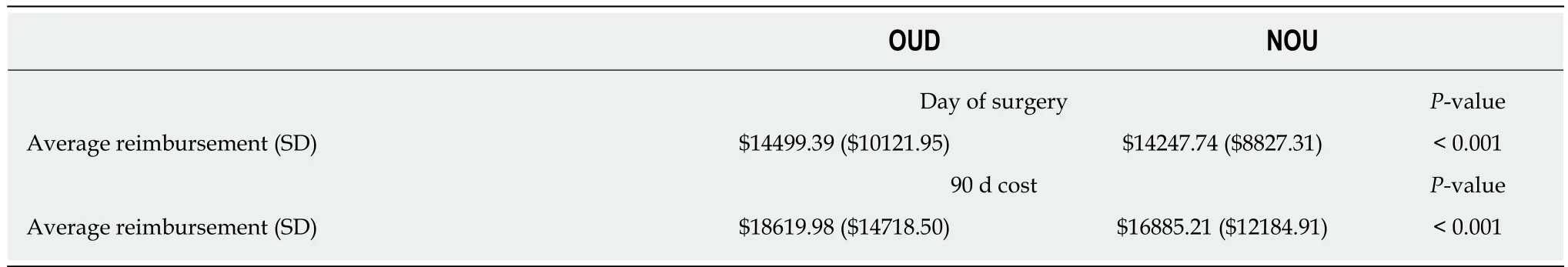
Table 4 Comparison of day of surgery and total global 90-d episode of care reimbursement amongst opioid abusers and non-opioid abusers undergoing primary total knee arthroplasty within the medicare population
ARTICLE HIGHLIGHTS
Research background
Opioid use has been shown to be effective method of analgesia following orthopedic surgery,and as a result, the prescribing rates of opioids have increased. Currently, orthopedic surgeons are the third highest prescribers of opioids following internists and dentists. The literature demonstrates that opioids are known to interfere with endogenous synthesis of testosterone and estrogen, which are vital for proper bone mineralization; in addition to other complications.There is no study to our knowledge which has analyzed the effects of opioid abuse and dependency on implant related complications in patients undergoing primary total knee arthroplasty (TKA).
Research motivation
As the number of prescriptions and abuse potential is increasing within the United States, its impact in orthopedics should be well understood. The study addresses the question on the implant related complications orthopedic surgeons may encounter in patients who have a history of opioid abuse and dependency following primary TKA. The study will allow for further studies on how to properly optimize opioid abusers prior to undergoing surgery.
Research objectives
The authors of this study wanted to determine the impact opioid abuse and dependency on implant related complications in patients undergoing primary TKA in patients greater than the age of 65.
Research methods
Patients who underwent primary TKA with a history of opioid abuse and dependency were identified from the Medicare claims database and were randomly matched 1:1 to a control group. Two-year implant related complications were analyzed and compared, along with 90-d reimbursement rates, along with day of surgery and total global 90-d episode of care costs.
Research results
The study found that patients who with a history of opioid abuse and dependency were at greater odds of developing implant related complications compared to controls. Implant related complications which were higher in the study group consisted of: requiring a revision procedure, periprosthetic fractures, prosthetic joint infection, mechanical loosening, in addition to others. Similarly, 90-d readmission rates along with day of surgery and total global 90-d episode of care costs were higher in patients with a history of opioid abuse and dependency compared to controls.
Research conclusions
The findings of the study demonstrate that opioid abuse and dependency increase the odds of developing implant related complications, 90-d readmission rates, and cost within patients who are undergoing primary TKA. These findings further confirm the hypothesis that patients with a history of opioid abuse or dependency would have greater complications following surgery compared to controls. The results of the study should warrant further studies on how to offset the detrimental effects of opioid abuse on bone mineralization.
Research perspectives
Patients with a history of opioid abuse or dependency are at a significantly greater risk of implant related complications, 90-d readmission rates, and cost following primary TKA. Further research should be warranted at identifying these patients prior to surgery and adequately optimizing them prior to surgery.
杂志排行
World Journal of Orthopedics的其它文章
- Changing trends in the mortality rate at 1-year post hip fracture - a systematic review
- Aetiology of Legg-Calvé-Perthes disease: A systematic review
- Short-term differences in anterior knee pain and clinical outcomes between rotating and fixed platform posterior stabilized total knee arthroplasty with a new femoral component design
- Linkage of microbiota and osteoporosis: A mini literature review