胎儿畸形相关环境因素调查分析
2019-02-10林秀郑莲钦石秀红
林秀 郑莲钦 石秀红

[摘要] 目的 分析研究引起胎儿畸形的相关环境因素,对孕期遗传咨询提供参考意见,以提高人口素质水平。方法 研究对象方便选取该院2017年10月—2018年12月间确诊为胎儿发育异常的120例孕妇和同期正常妊娠的120名孕妇,分别记为观察组和对照组。两组患者在院期间予相同孕期饮食、适当运动及营养素补充,以问卷调查形式对两组孕妇的生活习惯及环境因素进行统计分析,比较所观察危险因素与胎儿畸形的发生在两组孕妇之间有无差异。结果 观察组孕妇的文化程度为高中/中专及以上的占37.50%,明显低于对照组80.00%(χ2=14.160,P=0.000);观察组孕前半年即孕3个月内接触新房、车和家具等人数均多于对照组(χ2=31.510,P=0.000);观察组孕妇抽烟、酗酒者占8.33%,明显高于对照组0.83%(χ2=31.510,P=0.000);观察组孕妇丈夫抽烟、酗酒者占48.33%,明显高于对照组25.00%(χ2=32.110,P=0.000);观察组孕妇长期接触宠物者占22.50%,明显高于对照组11.67%(χ2=6.970,P=0.000);观察组长期接触电子产品者占53.33%,明显高于对照组17.50%(χ2=19.600,P=0.000);观察组常用重金属含量超标的化妆品者占25.83%,明显高于对照组4.17%(χ2=14.810,P=0.000);观察组有机会吸入空气中残余农药者占14.17%,高于对照组10.00%(χ2=14.620,P=0.000);观察组频繁烫发、染发者占80.00%,明显高于对照组27.50%(χ2=40.820,P=0.000);观察组常用空气清新剂、杀毒剂者占26.67%,高于对照组14.17%(χ2=24.420,P=0.000);观察组增补叶酸者占21.67%,明显低于对照组53.33%(χ2=24.340,P=0.000)。 结论 胎儿出现畸形的高危环境因素主要包括孕妇周围环境、不良生活习惯、接触化学因素三大方面。在备孕阶段的夫妇和处于孕期的孕妇应尽量规避上述高危因素、积极补充叶酸、孕前咨询、定期孕检,加强孕期保健,向孕妇普及产检的重要性,以避免或减少胎儿畸形的出现,降低畸形儿的出生率,从而提高生育质量及孕龄妇女的身心健康。
[关键词] 胎儿畸形;环境因素;叶酸
[中图分类号] R5 [文献标识码] A [文章編号] 1674-0742(2019)12(a)-0104-04
[Abstract] Objective Analyze and study the relevant environmental factors that cause fetal malformation, and provide reference for genetic counseling during pregnancy to improve the quality of the population. Methods A total of 120 pregnant women diagnosed with abnormal fetal development and 120 pregnant women with normal pregnancy during the period from October 2017 to December 2018 in the hospital were convenienty selected as observation group and control group. The two groups of patients were given the same pregnancy diet, appropriate exercise and nutrient supplement during the hospital. The living habits and environmental factors of the two groups of pregnant women were statistically analyzed by questionnaire. The observed risk factors and fetal malformations occurred in the two groups of pregnant women, to observe whether there is any difference between them. Results The education level of the pregnant women in the observation group was 37.50% of the high school/secondary school and above, which was significantly lower than that of the control group 80.00% (χ2=14.160, P=0.000); the observation group was exposed to new houses, cars and the first half of pregnancy during the first half of pregnancy. The number of furniture and other people was higher than that of the control group (χ2=31.510,P=0.000); the pregnant women in the observation group smoked and alcoholics accounted for 8.33%, which was significantly higher than the control group 0.83%(χ2=31.510, P=0.000); Smoking and alcohol abuse accounted for 48.33%, which was significantly higher than 25.00% of the control group(χ2=32.110, P=0.000). The pregnant women in the observation group accounted for 22.50% of the long-term exposure to pets, which was significantly higher than the control group of 11.67% (χ2=6.970, P=0.000); 53.33% of the observation group's long-term exposure to electronic products, significantly higher than the control group 17.50% (χ2=19.600, P=0.000); the observation group used the heavy metal content exceeding the standard of cosmetics accounted for 25.83%, significantly higher than the control group 4.17 %(χ2=14.810,P=0.000); the observation group had the opportunity to inhale the residual pesticide in the air accounted for 14.17%, which was higher than the control group 10.00%(χ2=14.620, P=0.000); the observation group frequent perm and dyed hair accounted for 80.00%, significantly higher than the control group 27.50%(χ2=40.820, P=0.000); the observation group used air fresheners, anti-virus agents accounted for 26.67%, higher than the pair According to the control group 14.17%(χ2=24.420, P=0.000); the folic acid supplementation in the observation group accounted for 21.67%, which was significantly lower than the control group 53.33%(χ2=24.340, P=0.000). Conclusion The high-risk environmental factors of fetal malformation mainly include three aspects: the surrounding environment of pregnant women, bad living habits and chemical factors of exposure. Couples in the pregnancy stage and pregnant women in pregnancy should try to avoid the above-mentioned high-risk factors, actively supplement folic acid, pre-pregnancy counseling, regular pregnancy check, strengthen pregnancy care, and popularize the importance of birth check-up to pregnant women to avoid or reduce the occurrence of fetal malformation and reduce The birth rate of deformed children, thereby improving the quality of birth and the physical and mental health of women of gestational age.
[Key words] Fetal malformation; Environmental factors; Folic acid
胎儿畸形是胎儿在子宫发育过程中出现遗传物质改变或身体结构异常的现象,已经成为导致围产儿和婴儿死亡的首要原因,胎儿畸形给孕产妇、其家属及整个社会均带来了消极影响[1]。每年全世界有超过550万畸形胎儿出生,畸形胎儿的数量占胎儿总出生数量的3.9%,我国畸形胎儿及儿童数量占总人口的5.8%,因此积极预防胎儿畸形对提高我国人口质量有重要意义。研究对象方便选取该院产科从2017年10月—2018年12月间收治的确诊为胎儿发育异常的孕妇120例,利用超声仪器对妊娠23~29周的孕妇进行实时脏器及体表结构全面检查。对确诊为胎儿发育异常的孕妇进行致畸因素统计分析,从根本上减少环境因素引起的胎儿畸形,从而促进优生优育及育龄妇女的身心健康,现报道如下。
1 资料与方法
1.1 一般资料
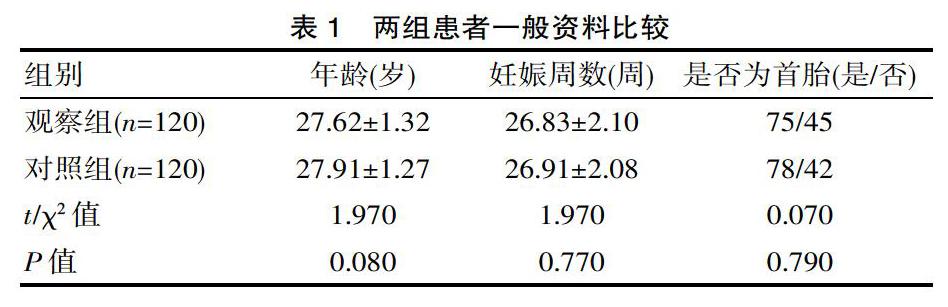
研究对象方便选取该院产科收治的确诊为胎儿发育异常的孕妇120例作为观察组,选择同期120名正常妊娠的孕妇作为对照组。纳入标准:①观察组患者符合第9版《产科学》对胎儿畸形的诊断标准[2];②患者未合并严重心脑血管、肝、肾等实质性脏器组织疾病;③患者无其他自身免疫性、血液和神经系统疾病;④患者及家屬知情,且已签署知情同意书。排除标准:①妊娠周数<23周或>29周者;②年龄<25岁或>29岁者;③无法完整配合研究进行者。两组患者在性别、年龄、妊娠周数及是否为首胎等一般资料方面比较,均差异无统计学意义(P>0.05),故具有可比性,见表1。
1.2 方法
对两组孕妇以调查问卷形式进行基本资料获取。主要调查内容包括:孕妇本人年龄、文化程度、妊娠周数、现患疾病、既往患病、居住、生活、工作环境、生活习惯、是否接触猫狗类宠物、是否经常染发、烫发以及接触重金属超标的化妆品等,以及是否增加叶酸或富含叶酸食物摄入量等。
1.3 统计方法
以SPSS 20.0统计学软件统计分析研究数据,计量资料用均数±标准差(x±s)表示,行t检验,计数资料用[n(%)]表示,行χ2检验,P<0.05为差异有统计学意义。
2 结果
在所有的研究因素中,与孕妇及其丈夫有关的行为习惯及环境因素共有14个,组间比较差异有统计学意义(P<0.05),两组孕妇胎儿畸形相关因素比较。见表2。
3 讨论
引起胎儿畸形的原因有很多,机制复杂,不仅包括家族遗传和母体因素,外界环境因素的影响也不容小觑。相关研究显示[3],近年来随着环境恶化加重,先天性畸形儿的发生率呈升高趋势。同时孕前半年及孕3个月内家庭装修或接触新家具,经常染发、烫发、长期使用含重金属的化妆品,接触宠物,孕妇或丈夫吸烟、酗酒,工作中接触有害物质均会导致胎儿畸形的发病率。适量补充叶酸可减少致畸因素对其生长发育的影响。孙越等[6]通过对胎儿先天畸形孕产妇高危因素分析,计算并比较各危险因素的相对危险度(OR)后认为,孕前后半年家庭装修或购置新家具(OR=4.883)、工作中接触有毒物质(OR=9.389)是孕期周围环境因素引起胎儿畸形的高危因素;增补叶酸(OR=0.125)为保护性因素。李喜莲[9]等通过研究证明,孕妇在孕期、备孕期间主动或被动吸烟(OR=3.162)、接触宠物(OR=3.840)、接触化学制剂(OR=3.053)、文化程度低(OR=2.355)等行为是导致胎儿先天畸形的主要危险因素;补充叶酸(OR=0.056)可对胎儿发育有一定的保护作用。对胎儿畸形出现的原因进行分析、早期预防、定期孕检,可对孕前或孕早期的问题提供参考建议,而且可以在发现胎儿畸形严重时及时引产,有效提高人口质量。
研究表明[4],备孕及怀孕初期,住房装修和接触新家具对胎儿畸形的形成均有显著影响。且居住环境周围有化工厂、垃圾焚烧厂及电力厂等均是出现胎儿畸形的高危因素,因为化学反应、燃料燃烧产生的毒害气体挥发到空气中,长期吸入会使精子与卵子变质、发育畸形,还可使处于生长发育期的胚胎发育畸形,发生结构改变,导致胎儿畸形[5-6]。因此孕妇在孕前半年及孕3个月内,应注意周围环境是否安全,避免长时间暴露于不良环境中[7-8]。其次,孕妇的生活习惯对胎儿畸形的发生也有重要影响。该研究显示,观察组孕妇丈夫吸烟、酗酒及孕妇本人吸烟、酗酒构成比分别占48.33%和8.33%,明显高于对照组(25.00%和0.83%),组间比较差异有统计学意义(P=0.000);孕妇长期接触电子设备、饲养宠物构成比分别占53.33%和22.50%,明显高于对照组(17.50%和11.67%),组间比较差异有统计学意义(P=0.000)。吸烟、酗酒、电子辐射和宠物携带的细菌病毒和寄生虫等因素均会降低孕妇的抵抗力[9-10],间接影响胎儿的生长发育,增加胎儿畸形的发生率。因此,有备孕准备或已经怀孕的孕妇应禁烟戒酒,改善不良生活习惯,以减少有害因素对胎儿生长的影响。长期接触化学物品也易引起胎儿畸形,该研究显示,观察组孕妇孕前半年及孕3个月内,频繁染发、烫发与常使用重金属含量超标的化妆品者构成比分别占80.00%和25.83%,经常使用空气清新剂、杀虫剂及接触空气中残余的农药构成比分别占26.67%和14.17%。当孕妇接触此类化学危害因素时,胎儿也会受到间接伤害,易出现发育异常[11-13]。此外孕妇的文化程度对胎儿畸形的形成也有一定影响:文化水平较低的孕妇常不具备孕前检查和定期孕检意识,无法及时监测胎儿生长状况,无视防护措施等。因此,加强普及孕前及孕期的宣教工作对胎儿的正常发育和提高人口质量有重要作用。
综上所述,有效规避引起胎儿畸形的危险因素,教育孕妇养成健康、良好的生活习惯,早期补充叶酸,加强孕妇定期产检意识,普及产前诊断与畸形儿筛查,可有效降低畸形儿的出生率,促进优生优育,是提高人口质量的有力举措。
[参考文献]
[1] 李霞,曾维佳,何薇,等. 不同孕周期胎儿畸形特征及超声诊断结果分析[J].中国优生与遗传杂志,2018,17(2):81-84.
[2] 林丽,高丽素,许玫,等. 胎儿畸形的影响因素分析[J]. 中国卫生标准管理, 2017, 8(18):1-3.
[3] Wei L, Qiao P, Shi Y, et al. Triclosan/triclocarban levels in maternal and umbilical blood samples and their association with fetal malformation[J]. Clinica Chimica Acta, 2017, 466:133-137.
[4] 张晓敏, 郭小春. 彩色多普勒超聲在产前胎儿畸形筛查中的应用价值[J]. 中国现代医学杂志, 2017, 27(3):112-115.
[5] Wataganara T, Grunebaum A, Chervenak F, et al. Delivery modes in case of fetal malformations[J]. Journal of Perinatal Medicine, 2017, 45(3):273-279.
[6] 孙越, 肖岩岩, 张战红. 胎儿畸形相关环境因素统计分析[J]. 中国优生与遗传杂志, 2011, 19(6):93-94.
[7] 兰清馥, 盛建国. 系统超声检查在不同孕期诊断胎儿畸形的临床观察[J]. 海军医学杂志, 2017, 38(1):66-69.
[8] 曾巍, 钱小芳, 刘桂华,等. 胎儿畸形选择引产孕妇心理准备的质性研究[J]. 中华现代护理杂志,2017,23(3):345-349.
[9] 李喜莲, 张斌. 胎儿先天畸形孕产妇高危因素分析[J]. 中国临床医学, 2017, 24(3):377-381.
[10] Yu M, Chen L, Peng Z, et al. Mechanism of deoxynivalenol effects on the reproductive system and fetus malformation: Current status and future challenges[J]. Toxicology in Vitro An International Journal Published in Association with Bibra, 2017, 41:150.
[11] Schwartz K L, Chan T, Rai N, et al. Zika virus infection in a pregnant Canadian traveler with congenital fetal malformations noted by ultrasonography at 14-weeks gestation:[J]. Trop Dis Travel Med Vaccines, 2018, 4(1):2.
[12] 普小芸,李力,郑英如,等.第三军医大学第三附属医院近几年新生儿先天畸形相关因素的临床研究[J].中国优生与遗传杂志,2017,25(2):99-101.
[13] Lubinsky M. An epigenetic association of malformations, adverse reproductive outcomes, and fetal origins[J]. Journal of Assisted Reproduction & Genetics, 2018, 35(1):1-12.
(收稿日期:2019-09-03)