抗生素降阶梯治疗慢性阻塞性肺疾病合并重症肺炎效果分析
2019-02-10翟溶凡蒋先训
翟溶凡 蒋先训

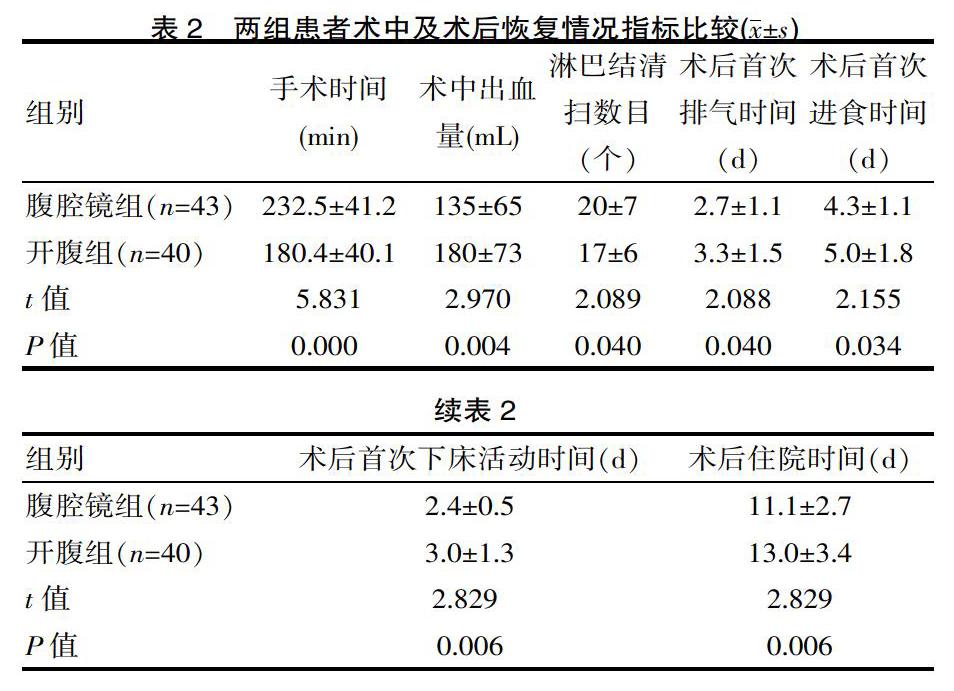
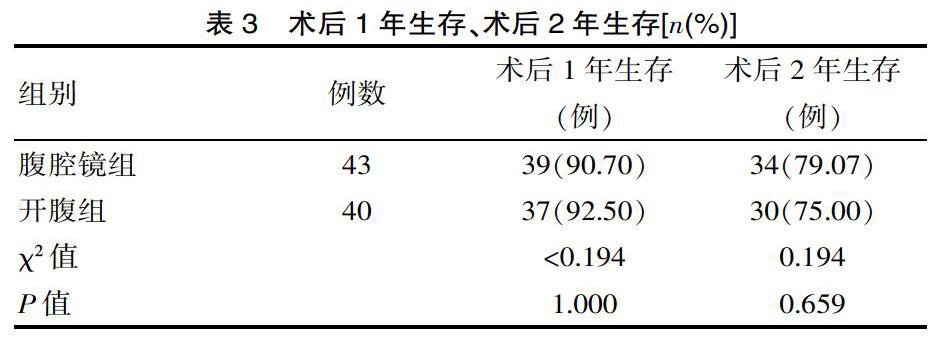
[摘要] 目的 探討比较胃癌在腹腔镜手术与开腹手术中的疗效。 方法 采用回顾性队列研究方法。整理了2011年1月—2017年4月该院收治的83例胃癌患者,其中腹腔镜组43例,开腹组40例。腹腔镜组平均年龄:﹙62.5±11.3﹚岁,开腹组平均年龄:(60.3±9.2)岁,观察指标:①临床资料;②术中术后情况:手术时间,术中出血量,淋巴结清扫数目,术后首次排气时间,术后首次进食时间,术后首次下床活动时间,术后住院时间,术后1年生存,术后2年生存;③术后并发症:切口感染,肺部感染,腹腔感染,腹腔出血,吻合口瘘,十二指肠残端瘘,胃瘫。 结果 ①临床资料比较:二者在性别、年龄、BMI、肿瘤部位、肿瘤分期方面,均差异无统计学意义(P>0.05)。②术中术后情况:术中出血量(135±65)mL、术后首次排气时间(2.7±1.1)d、术后首次进食时间(4.3±1.1)d、术后首次下床活动时间(2.4±0.5)d、术后住院时间(11.1±2.7)d腹腔镜组指标均优于开腹组,差异有统计学意义(t=2.970,2.088,2.155,2.829,0.194,P=0.004,0.040,0.034,0.006,0.659)。手术时间腹腔镜组(232.5±41.2)min长于开腹组(180.4±40.1)min,差异有统计学意义(t=5.831,P=0.000),术后1年、2年生存时间差异无统计学意义(P>0.05)。③术后并发症:二者术后并发症(切口感染,肺部感染,腹腔感染,腹腔出血,吻合口瘘,十二指肠残端瘘,胃瘫)总数比较差异无统计学意义(P>0.05)。 结论 通过临床对比研究,腹腔镜手术治疗胃癌相对于开腹手术治疗胃癌,虽然手术时间长于开腹组,但具有术中出血少、淋巴结清扫数目多、术后胃肠功能恢复快、早期进食、下床活动、住院时间短等优点,同时在术后1年、2年生存期及术后并发症方面无统计学差别,是损伤小,恢复快,安全可靠的术式,可以在临床推广发展。
[关键词] 胃癌;腹腔镜;开腹;疗效
[中图分类号] R735 [文献标识码] A [文章编号] 1674-0742(2019)12(a)-0015-04
[Abstract] Objective To investigate the efficacy of gastric cancer in laparoscopic surgery and open surgery. Methods A retrospective cohort study approach was used. 83 patients with gastric cancer admitted to our department from January 2011 to April 2017 were enrolled, including 43 in the laparoscopic group and 40 in the open group. The average age of the laparoscopic group was (62.5±11.3)years, and the average age of the open group was (60.3±9.2)years. Observed indicators: 1.clinical data;2.intraoperative and postoperative conditions: operation time, intraoperative blood loss, lymph node dissection number, first postoperative exhaust time, first postoperative feeding time, first time to get out of bed after surgery, postoperative hospital stay, 1 year postoperative survival, 2 years postoperative survival;3.postoperative complications: incision infection , pulmonary infection, abdominal infection, abdominal bleeding, anastomotic leakage, duodenal stump fistula, stomach cramps. Results 1.Comparison of clinical data: There was no significant difference in gender, age, BMI, tumor location and tumor stage (P>0.05). 2.Intraoperative and postoperative conditions: intraoperative blood loss (135±65)mL, first exhaust time after surgery (2.7±1.1)d, first time after surgery (4.3±1.1)d, first time after going to bed time (2.4±0.5)d and postoperative hospital stay (11.1±2.7)d were better than the open group in the laparoscopic group , the difference was statistically significant(t=2.970, 2.088, 2.155, 2.812, P=0.004, 0.040, 0.034, 0.006). The laparoscopic group (232.5±41.2)min was longer than the open group (180.4±40.1)min, and there was a statistical difference (t=5.831, P=0.000). There was no significant difference in 1-year and 2-year survival time after surgery(P>0.05). 3.Postoperative complications: there was no statistically significant difference in the total number of postoperative complications (incision infection, pulmonary infection, abdominal infection, abdominal hemorrhage, anastomotic leakage, duodenal stump fistula, stomach cramps(P>0.05). Conclusion Through clinical comparative study, laparoscopic surgery for gastric cancer compared with open surgery for gastric cancer, although the operation time is longer than the open group, but with less intraoperative bleeding, more lymph node dissection, postoperative gastrointestinal function recovery, early eating, getting out of bed, short hospital stay, etc., and no statistical difference in 1-year, 2-year survival and postoperative complications are small, quick recovery, safe and reliable, and can be promoted in clinical practice and development.
综上所述,与传统开腹治疗胃癌手术相比效,腹腔镜胃癌根治术是术中损伤更小,术后恢复更快,安全有效的手术方式,值得推广应用。虽然目前在进展期胃癌中腹腔镜手术仍然存在着一定争议,但随着腹腔镜器械、设备的完善成熟、腹腔镜在多学科的广泛开展、长期的多中心大样本随机对照试验的进一步验证,我相信腹腔镜在胃癌手术方面的优势将更加显著,它将与传统开腹手术长期并存。
[参考文献]
[1] Siegel RL,Miller KD,Jemal A.Cancer statistics,2018 [J].CA Cancer J Clin,2018,68(1):7-30.
[2] 国家消化系疾病医学研究中心,中华医学会消化内镜学分会,中华医学会健康管理学分会,等.中国早期胃癌筛查流程专家共识意见(草案,2017年,上海)[J].中华消化杂志,2018,38(2):87-92.
[3] 蔡慧,徐光寰,王珏.上海市原卢湾区2004-2011年消化系统常见肿瘤的发病和死亡趋势分析[J].中国临床医学,2018, 25(4): 542-548.
[4] 中国医师协会内镜医师分会腹腔镜外科专业委员会,中国研究型医院学会机器人与腹腔镜外科专业委员会,中国腹腔镜胃肠外科研究组.中国腹腔镜胃癌根治手术质量控制专家共识(2017版) [J]. 中华消化外科杂志,2017,16(6):539-547.
[5] 邢亚峰.阿帕替尼联合希罗达治疗晚期胃部的临床疗效观察[J].临床医学进展,2018,8(9):855-860.
[6] 董朋朋,张红军 .晚期胃癌免疫治疗研究进展[J].养生保健指南,2019(21):203.
[7] 梁良.调强放疗和同步化疗用于进展期胃癌治疗中的临床效果[J].中国社区医师,2019(3):53-56.
[8] 胡建昆,张维汉,陈心足.从中国CLASS-03a研究的开展看腹腔镜手术联合新辅助化疗的胃癌治疗[J].中华胃肠外科杂志,2018(2):138-142.
[9] Kitano S, Iso Y, Moriyama M, et al. Laparoscopy-assistedBillrothI gastrectomy[J].Surg Laparosc Endosc,1994,4(2):146-148.
[10] 日本胃癌学会 胃癌处理规约[M]. 东京:金原出版株式会社,2017.
[11] Lin JX, Huang CM, Zheng CH, et al. Is All Advanced Gastric Cancer Suitable for Laparoscopy-Assisted Gastrectomy With Extended Lymphadenectomy A Case-Control Study Using a Propensity Score Method[J]. Ann Surg Oncol,2016,23(4):1252-1260.
[12] Chen QY, Zheng CH, Li P, et al. Which method is more suitable for advanced gastric cancer with enlarged lymph nodes, laparoscopic radical gastrectomy or open gastrectomy[J].Gastric Cancer,2018,21(5):853-863.
[13] 张军永,邢攸轩.腹腔镜远端胃癌根治与开腹对早期胃癌的影响[J].中国继续医学教育,2018, 10(36): 62-64.
[14] 李国新,胡彦锋,刘浩.中国腹腔镜胃肠外科研究组CLASS-01研究进展[J].中华消化外科杂志,2017,16(1):38-42.
[15] Lee HJ, Hyung WJ, Yang HK, et al. Morbidity of laparoscopic distal gastrectomy with D2 lymphadenectomy compared with open distal gastrectomy for locally advanced gastric cancer: Short term outcomes from multicenter randomized controlled trial(KLASS-02)[J].J Clin Oncol,2016,34:abstr 4062.
[16] Park YS, Son SY, et al. Eleven-year experience with 3000 cases of laparoscopic gastric cancer surgery in a single institution: analysis of postoperative morbidities and long-term oncologic outcomes[J]. Surg Endosc,2016,30(9):3965-3975.
[17] Xu Y, Hua J, Li J, et al. Laparoscopic versus open gastrectomy for gastric cancer with serous invasion: long-term outcomes[J].J Surg Res,2017,215:190-195.
[18] 顏宏锐,朱焕明.胃肠外科腹腔镜技术在基层医院“复制”的学习曲线 [J].系统医学,2018(5):98-100.
[19] 黄昌明,林建贤.腹腔镜胃癌根治术淋巴结清扫中团队配合的策略与技巧[J].中华消化外科杂志,2019,18(3):209-212.
[20] 钱俊甫,李书旺,牛国浩. 腹腔镜下不同淋巴结清扫方案对1-3期胃癌手术临床指标及术后并发症的影响[J]. 2019,34(1):57-60.
[21] 高增战,李树营 .胃癌D2 根治术采用腹腔镜与传统开腹术治疗进展期胃癌的疗效对比 [J].中华普外科手术学杂志:电子版,2018,12(6):520-522.
(收稿日期:2019-08-10)