Hypertension, abnormal blood pressure circadian pattern, and frailty:data from the literature
2019-01-16FabioFabbianAlfredoDeGiorgiRosariaCappadonaDarioGozziMauroPasinRobertoDeGiorgioRobertoManfredini
Fabio Fabbian, Alfredo De Giorgi, Rosaria Cappadona, Dario Gozzi, Mauro Pasin,Roberto De Giorgio, Roberto Manfredini
1Faculty of Medicine, Pharmacy and Prevention, University of Ferrara, Ferrara, Italy
2Department of Internal Medicine, General Hospital of Ferrara, Ferrara, Italy
Keywords: Blood pressure; Frailty; The elderly
According to the National Health and Nutrition Examination Survey (NHANES) data, more than 65% of people aged ≥ 60 years are hypertensive.[1]Diabetes mellitus,dyslipidemia, obesity and renal failure are frequently associated with hypertension, increasing the risk of negative outcomes, such as stroke and myocardial infarction.[2]The Hypertension in the Very Elderly Trial (HYVET)[3]and the Systolic Blood Pressure Intervention Trial (SPRINT)[4]studies established that effective treatment of hypertension even in the oldest old reduced major cardiovascular events.Frailty is a major clinical condition in older adults,[5]and it has been recognized as an independent cause of death as far several years ago.[6]Definition of frailty is still a matter of debate, and its estimated prevalence could vary depending on the definition used in population-based studies. Frailty could define different conditions based on clinical phenotype (suggesting a biological approach), cumulative burden of diseases and symptoms and a combination of physical and mental decline, associated with social isolation (suggesting a multidomain approaches).[7]In their systematic review of the literature on cross-sectional data from community-based cohorts (n = 61,500 patients), Collard, et al.[8]found a prevalence of frailty of 10.7% , higher in women than in men, and increasing with age. The American College of Cardiology Foundation and the American Heart Association expert consensus document on hypertension in the elderly[9]suggested that indications for ambulatory blood pressure monitoring (ABPM) were: (1) not clear hypertension diagnosis and/or response to anti-hypertensive therapy,(2) suspected syncope or hypotensive disorders, (3) suspected white coat hypertension in order to avoid overtreatment, and (4) suspected masked hypertension. The authors reported that cardiovascular death increased from 10% and 18% for each 10 mmHg increase in daytime and night-time systolic blood pressure (SBP), respectively. However, such consensus document made no mention about frail elderly subjects. Recently, Aprahamian, et al.[10]evaluated the prevalence of hypertension, and factors associated with frailty in a cohort of 619 older adults. Hypertension was diagnosed in 83% of cases, and subjects with hypertension were older, had history of stroke and myocardial infarction.Moreover, hypertension was independently associated with frailty.[10]The aim of this study is to detect if literature has been evaluating the relationship between ABPM and frailty.
We performed a MEDLINE literature search to identify relevant papers focused on ABPM and frailty. The following search terms were used: “ambulatory blood pressure monitoring”, “elderly”, “older adults”, “comorbidity”, “multimorbidity” and “frailty”. All cross-sectional studies, metaanalyses, controlled trials, cohort studies, case-control studies were considered for inclusion. Case reports, comments,discussion letters, articles in languages other than in English,and conference abstracts or proceedings were excluded.
The PubMed search on ABPM, updated to August 2018,collected over 13,300 articles. By adding the term “elderly”to the search string, reduced the number of articles to more than 8200. By further adding the terms “older adults”, the number of items reduced to 533. Finally, adding to “ambulatory blood pressure monitoring” the term “comorbidity”restricted results to 168 articles. PubMed search by using the terms “ambulatory blood pressure monitoring” and“multimorbidity” found only one article, and “multimorbidity” plus “frailty” yielded seven articles. We further analyzed the references of these seven papers. Authors, years of publication, country, main patients’ characteristics, and outcomes were recorded. Due to the heterogeneity ofthe studies, it was not possible to proceed to a meta-analysis,so we decided to limit to a narrative review. Only three studies really evaluated frail patients. Overall, the total number of patients enrolled in the three studies were 1224(645 women), and mean age was 76 years (range 72-83).The three studies, one observational and two cross-sectional,were conducted in Italy, Brazil, and Spain, respectively. The main characteristics of these studies are reported in Table 1.
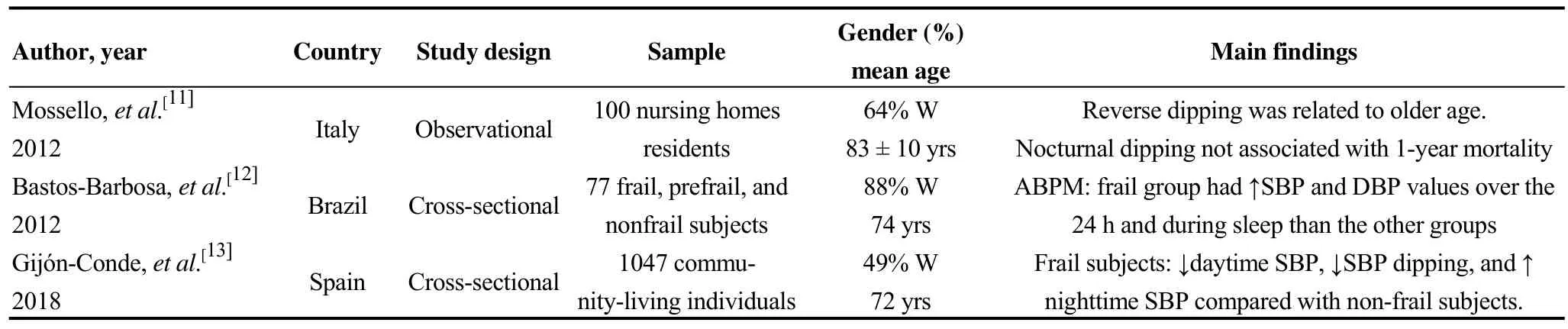
Table 1. Available studies on the relationship between ambulatory blood pressure (ABPM) and frailty.
Study 1. Mossello, et al.[11]evaluated 100 nursing homes residents (51% hypertensives) with mean Charlson comorbidity score of 5 ± 2. A maintained circadian rhythm was observed in 28% of patients, 39% were non-dippers, 33%had nocturnal hypertension (reversed circadian pattern).Moreover, 33% had white coat effect, 11% had masked hypertension and 17% were hypertensive measuring BP both in the clinic and with ABPM. Reverse dipping was related to older age, however nocturnal dipping was not associated with 1-year mortality as well as preserved or altered circadian pattern.
Study 2. Bastos-Barbosa, et al.[12]evaluated 77 frail, prefrail, and nonfrail subjects, with a mean number of comorbidities of 2.8 ± 1.6. They underwent ABPM, and frail group had higher systolic and diastolic BP values over the 24 h and during sleep than the other groups.
Study 3. Gijón-Conde, et al.[13]study investigated 1047 community-living individuals (6% frail, and 8.1% with disability). Frail subjects had 3.5 mmHg lower daytime SBP,3.3% less SBP dipping, and 3.6 mmHg higher nighttime SBP, compared with nonfrail subjects. Subjects with disability had 2.5 mmHg lower daytime SBP, 2.5% less SBP dipping, and 2.7 mmHg higher nighttime SBP compared with subjects without disability.
To the best of our knowledge, this this the first attempt of reviewing the available data on the relationship between hypertension, ABPM and frailty. Hypertension and its consequences are often present in the clinical history of older adults. Whether treatment of hypertension is beneficial in multimorbid older adults with frailty is still matter of debate,due to possible secondary adverse effects, such as hypotension, orthostatic hypotension, and falls.[14]The benefits related to preventive pharmacological treatment of hypertension are not certain,[15]and it has also been reported that in frail patients the chance of mortality decreases with increasing SBP and diastolic blood pressure (DBP).[16]Although the growing proportion of the population aged ≥ 80 years is accompanied by increasing number of patients with multimorbidity, there are no conclusive data regarding the causal association between the two conditions. In fact, although frailty and multimorbidity were associated conditions in older adults, it has estimated that prevalence of multimorbidity in frail individual was 72% while prevalence of frailty among multimorbid individuals was significantly lower (16%).[17]
BP exhibits a well-known circadian pattern, as the result of a complex series of neuroendocrine mechanisms, including hypothalamic-pituitary-adrenal system, hypothalamicpituitary-thyroid system, opioid, renin-angiotensin-aldosterone, plus endothelial systems and specific vasoactive peptides.[18]Moreover, a relationship between circadian BP organization and unfavorable cardiovascular events is well known,[19]and most unfavorable events, e.g., myocardial infarction, stroke, rupture or dissection of aortic aneurysms,exhibit an evident biphasic pattern characterized by a main peak in the morning.[20-22]Asleep SBP is considered the most significant BP-derived risk factors for CVD events.[23]
The association between hypertension and elderly and frailty may show various aspects. In older subjects, nocturnal dipping of lesser magnitude was associated with greater brain atrophy, and they both were also associated with slower gait speed and worse functional outcome after stroke.[24]Poor physical function and/or cognitive dysfunction have been shown to be possible valid markers likely to be associated with high nocturnal SBP.[25]However, particular attention should be given to older patients with dementia and mild cognitive impairment. In fact, excessive SBP lowering could be harmful in these patients, since low daytime SBP was independently associated with a greater progression of cognitive decline.[26]A calculation of the frailty index (FI) for participants of the HYVET showed that both the frailer and the fitter older adults with hypertension appeared protected against major CV events from treatment without evidence of an interaction between effect of treatment for hypertension and frailty.[27]It has been recently shown that 24 h, day and night SBP levels and SBP variability were positively related to cerebral small-vessel disease (cSVD) burden, moreover higher SBP levels and SBP variability were independent risk factors for cSVD.[28]An altered circadian BP pattern in frail subjects is not surprising, and nocturnal hypertension seems to represent frequent diagnosis. However management of hypertension in this population appears to be very complex. Older adults show high BP variability, hypotension is interspersed with hypertension on ABPM, BP variability is recognized as a common cause of falls and syncope. In frail hypertensive patients, extreme dipper pattern, orthostatic hypotension,post-prandial hypotension, target organ hypoperfusion, target organ damage and major clinical events could represent a vicious and harmful circle. Finally, growing attention is deserved to social and socioeconomic factors. Marital status(MS) impacts on cardiovascular health. In general, married persons show better outcomes, and men who were single generally had the poorest results.[29]Moreover, being married is associated with lower risk factors, including hypertension. In fact, Causland et al.[30]showed that married subjects showed greater odds of dipping (OR = 2.26) compared with unmarried ones, and married subjects had a lower nighttime SBP (-2.4 mmHg), more pronounced in men than in women (-3.1 mmHg and 1.7 mmHg, respectively).
Blood pressure target in older adults could vary depending on the patient’s clinical features. Presence of frailty could greatly impact BP target values to be reached by treatment, on the contrary fit elderly patients could tolerate lower BP values and could benefit from aggressive treatment. Moreover, frailty has been shown to be a significant independent factor contributing to worse adherence to pharmacological and non-paharmacological treatment of hypertension.[31]
In conclusion, there is an extreme paucity of literature dealing with the association between hypertension and frailty. Older people are often excluded by clinical trials,and this may explain the uncertainty of conclusions on benefits of harms of different pharmacological interventions.The world reality, especially in Europe but now also in China, is rapidly growing in age, and studies focused on elderly people are strongly needed. Moreover, particular attention has to be given even to marital status, since usually women live longer and men have poor outcomes.
Acknowledgements
The authors thank Dr. Claudia Righini and Dr. Donato Bragatto, Biblioteca Interaziendale di Scienze della Salute,General Hospital of Ferrara, for precious assistance. All authors had no conflict of interest related to this paper. Authors declare that there are not any potential conflicts of interests that are directly or indirectly related to the data presented in the paper.
杂志排行
Journal of Geriatric Cardiology的其它文章
- Applicability of the PRECISE-DAPT score in elderly patients with myocardial infarction
- Heart failure mortality compared between elderly and non-elderly Thai patients
- Value of cystatin C in predicting atrial fibrillation recurrence after radiofrequency catheter ablation
- Perspective of delay in door-to-balloon time among Asian population
- Characterization of coronary atherosclerotic plaques in a homozygous familial hypercholesterolemia visualized by optical coherence tomography
- Contralateral pneumothorax in the subacute phase after pacemaker implantation: lead retention and follow-up
