Perspective of delay in door-to-balloon time among Asian population
2019-01-16LongLIManYanWUFengZHANGSuFangLIYuXiaCUIDanHUHongCHEN
Long LI, Man-Yan WU, Feng ZHANG, Su-Fang LI, Yu-Xia CUI, Dan HU, Hong CHEN
Department of Cardiology, Beijing Key Laboratory of Early Prediction and Intervention of Acute Myocardial Infarction, Center for Cardiovascular Translational Research, Peking University People’s Hospital, Beijing, China
Keywords: Door-to-balloon time; Primary percutaneous coronary intervention; ST-segment elevation myocardial infarction; Written consent
1 Introduction
Effective and timely reperfusion of infarcted coronary artery is crucial to the treatment of patients with ST-segment elevation myocardial infarction (STEMI).[1,2]Current guidelines highly recommend that the door-to-balloon (D2B)time, as a quality metric of primary percutaneous coronary intervention (PCI) in patients with STEMI, should be ≤ 90 min and preferably less than 60 min.[3,4]However, significant variations from guidelines exist in the real world practices at hospitals. Nevertheless, the D2B alliance, an American College of Cardiology (ACC)’s Quality Improvement(QI) Campaign launched in November 2006, has successfully reached the above goal and set us an example.[5]By 2010, the median value of D2B time has decreased from 94 min to 64 min,[6]thus significantly reducing the mortality of STEMI.[7]Although China has also introduced its own guidelines on the management of STEMI and great effort has been put into practice, the trend of D2B time in China has not changed over the past decade. The median D2B time was 135 min about Beijing in 2006,[8]134 min about Xinjiang in 2010,[9]and 172 min about Henan in 2012,[10]respectively. Apparently, the median D2B time in China is significantly longer than that in the U.S. Moreover, the first national study on the median D2B time in China showed that only 27.8% of STEMI patients in China received primary PCI in 2011.[11]Unfortunately, since the record of hospital admission time and balloon dilation time is only available for less than 3.0% of all STEMI patients, the exact D2B time of the general patient population cannot be determined. Therefore, the findings shown in this study may partly explain that, unlike Western countries, why China is associated with a gradually rising mortality of acute myocardial infarction during the past decade.[12]
2 Comparison with the D2B alliance in the USA
Launched by the ACC’s QI Campaign in 2006, the D2B initiative in the USA has set us an excellent example of transformation in health care. Updated on the official website of ACC, the flow chart and time process of the D2B initiative were originally modified from the approach of Bradley, et al.[13]and included sections of introduction,news, toolkit and related research. The strength of the D2B program in the USA has focused on three prominent strategies. Firstly, pre-hospital electrocardiograph (ECG) was acquired by emergency medical services (EMS) for rapid identification of STEMI and subsequent diagnosis by a catheterization laboratory cardiologist for time saving. Secondly, the collaboration of interdisciplinary teams was established. Thirdly, an emergency department (ED) physician could communicate with the catheterization laboratory cardiologist to decide the option for operation (Figure 1B).Unfortunately, the hospitals in China seldom adopt these strategies. Especially, ED transport patients to catheterization laboratory usually after providing consent and finishing financial process in our country, causing delay for non-system reasons (Figure 1A). Moreover, the process and timeline of STEMI treatment in our center were compared with those used by the D2B alliance, and the results showed that all components of D2B time were prolonged except the time for the diagnosis and activation the catheterization laboratory. Approximately 20% to 40% of the patients in the step 2, step 3 and step 5 satisfied the standard, and the mean prolonged time of these three steps was less than 10 min.Moreover, the time to obtain patient consent was most remarkably increased, for average increased time was 20.3 min (Table 1). In fact, Bradley, et al.[13]described the features in top-performing hospitals by identifying six strategies, which were most adopted by the D2B initiative, in order to shorten the D2B time. Among these strategies, the establishment of an interdisciplinary collaborative team and the measurement of pre-hospital ECG by EMS were the approaches showing the most significant improvement.

Figure 1. Comparison of D2B process flow chart between the center of the authors (A) and D2B alliance (B). Path #1, patients arrived at the emergency department without pre-hospital electrocardiograms; Path #2 patients arrived at the emergency department with pre-hospital electrocardiograms. Cath lab: catheterization laboratory; D2B: door-to-balloon; ECG: electrocardiogram; ED: emergency department; EMS: emergency medical service; PCI: percutaneous coronary intervention; Pt: patient; STEMI: ST-segment elevation myocardial infarction.
3 Reasons of delay in D2B time
3.1 Clinical factors related to delay in D2B time
Many reasons can cause D2B delay.[14,15]In addition, it was shown that a shorter patient-specific D2B time[7]rather than the annual D2B time[16]is associated with a lower mortality. The 194 STEMI patients undergoing primary PCI in our study showed a median D2B time of 123 min and a mean D2B time of 132 ± 41 min. In addition, 147 (75.7%)patients had a D2B time of ≥ 90 min and they were allocated into a D2B delay group. Furthermore, the patients in the D2B non-delay group were more frequently observed with a history of diabetes mellitus or prior PCI operation, or symptoms of ST-segment elevation or left bundle branch block ECG on admission. There was no difference between the two groups in demographic features and culprit vessel of acute myocardial infarction (AMI). In a multivariable analysis, first abnormal ECG at arrival was the strongest predictor of non-delay in D2B time (OR = 8.806, 95% CI:1.15-67.21, P = 0.036). The presence of diabetes mellitus was also an independent predictor of non-delay in D2B time(OR = 2.174, 95% CI: 1.05-4.48, P = 0.035). Our studies identified several independent predictors of D2B non-delay as previous described, such as co-morbid conditions ofdiabetes and a diagnostic ECG at arrival.[17]However, although other studies showed that the patients with a history of prior PCI or admitted via EMS were likely to have a shorter D2B time, our study showed no such difference in the multivariate analysis.[18]Furthermore, there was no significant difference in mortality between D2B non-delay and D2B delay groups. The reason of such discrepancy may be due to the small sample size.

Table 1. Timeline compared with the D2B alliance in the USA.
3.2 Informed consent factors about delay in D2B time
A national study in the USA has showed that the delay in providing consent could result in the longest D2B time, and Asians are more unlikely to provide timely consent.[19]Interestingly, many studies reported that the failure to provide timely consent would cause prominent D2B delay for nonsystem reasons both in China and India.[8-10,20]However, more evidence is required to draw a definite conclusion. Brddock,et al.[21]have described seven classic elements as follows: (1)discussion of the patient’s role in decision making; (2) discussion of clinical issues or the nature of the decision; (3)discussion of alternatives; (4) discussion of the pros and cons of alternatives; (5) discussion of uncertainties associated with the decision; (6) assessment of the patient’s understanding; and (7) exploration of the patient’s preference. It is known that the USA Food and Drug Administration do not allow delayed informed consent in this critical situation.[22]Hence, our study focused on the comprehensive reasons behind the usual delay in obtaining consent from Asians.
In our study, the mean increased time was 20.3 min. In addition, the majority of consent signers were not patients themselves but their relatives (Table 2). Among these consent signers, 45.5% were the spouse of the patients, 40.9%were the children of the patients and only 2.7% were the patients. Therefore, consent signers were divided into two groups by the median consent time (28 min), and no difference was seen in the proportion of consent signers between the two groups (P = 0.275). Also, it was found that most patients were old and they were not willing to make their own decisions. Hence, the percentage of relatives as consent signers was higher in the group with a shorter consent time(72.7% vs. 54.4%, P = 0.027), potentially by saving the time waiting for their family members. Among the classic 7 elements of informed decision making, cardiologists in the longer consent time group were more likely to assess signer understanding and explore signer preferences (P = 0.012 and P = 0.033). Of all discussions carried out by cardiologists, 96 (54.5%) included the basic elements (elements 2, 3 and 4) and 36 (20.5%) contained all 7 elements. The more elements were discussed, the longer the consent time (4.9 ±1.3 vs. 5.2 ± 1.4, P = 0.035). Since signer understanding may account for consent delay, the signers were surveyed in more detail in this respect. More signers in the short consent time group realized the importance of timely reperfusion and hence were less worried about the risk of primary PCI(P = 0.027 and P = 0.034).
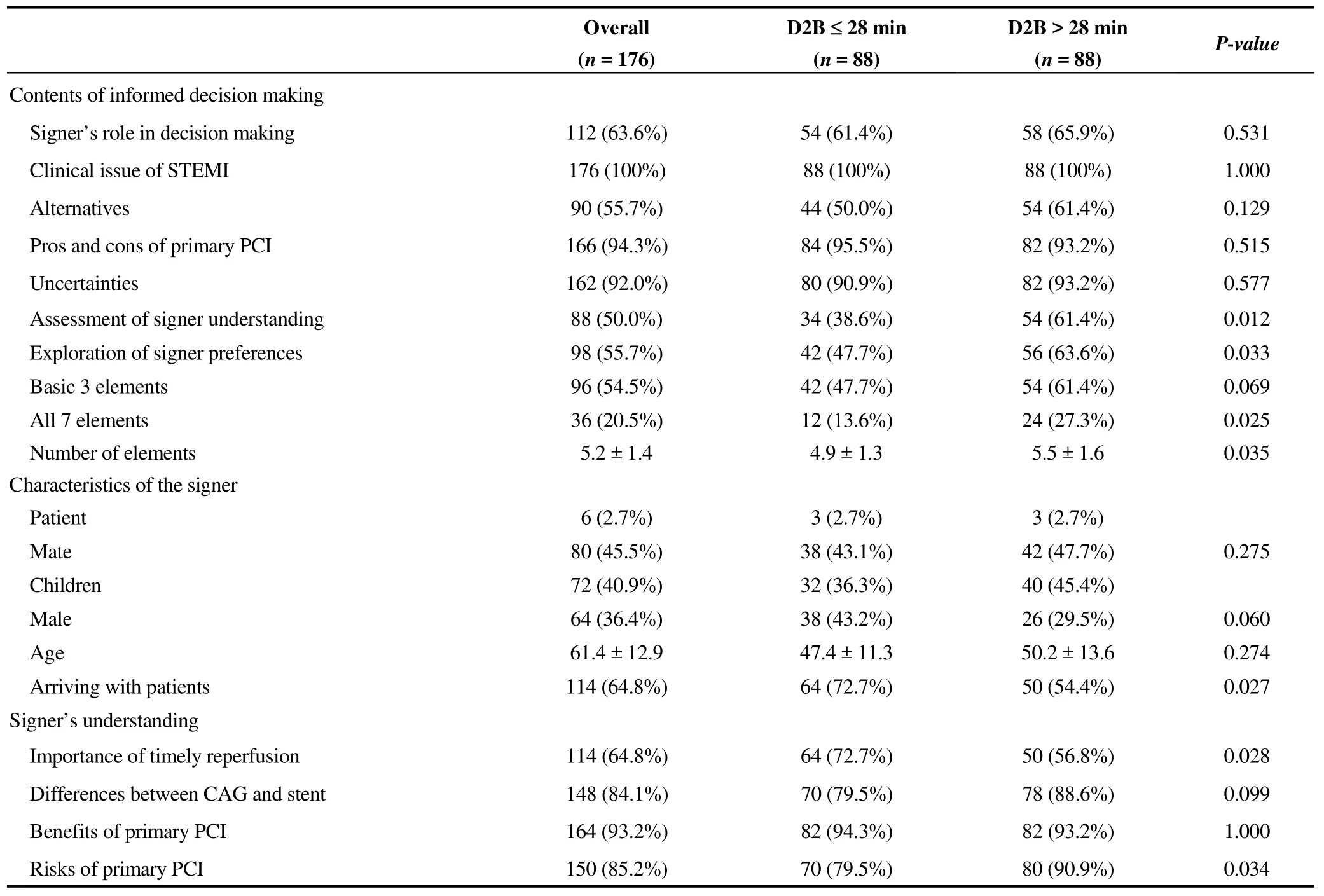
Table 2. Informed consent factors related to delay in D2B time.
It was found that, for some kind of culture reasons, Chinese and Indians value the opinions of the whole family.Almost all decisions made by their family members instead of patients themselves, the signer’s awareness of the PCI and the time of hospital admission appeared to be the main factors. Indeed, in many cases, staff often waited for patients’ relatives to arrive at the hospital. Michael, et al. reported that, in patients with stable coronary disease who chose not to undergo PCI, more complete elements were involved.[23]In addition, if the signers further realized the importance of timely reperfusion and hence were less worried about the risks, the time of decision making would be shorter. Therefore, policy makers should put more efforts on educating the public about the primary PCI.
4 Overview of the delay in D2B time in Asia.
The ratio between D2B time and guideline-recommended time of ≤ 90 min was summarized for Asia (Table 3). Most studies were based on national registries, which helped to comprehend the epidemiology and treatment of STEMI across the Asia. However, unlike the USA, most countries in Asia do not have national QI institutions to reach the goals of the guidelines in their practice and to shorten the discrepancy among different hospitals. Only Taiwan, Singapore and Israeli had a median D2B time of <90 min, indicating that more than half of the primary PCI procedures would meet the metrics recommended by the guideline. Many studies in China and India showed that the providence of informed consent causes significant D2B delay, while researchers in other counties have not mentioned this reason. The D2B time of primary PCI in the entire Asia is not optimistic. Among Asian countries, the median D2B time in Singapore and Israeli is shorter,[24-26]but no country reached the USA that 90% of D2B time should be < 90 min.[6]Therefore, countries in Asia, especially China and India, should develop their own framework in the practice.[27-31]After all, China and India have the highest populations in the world.

Table 3. Overview of the D2B time in Asia.
5 Conclusion
The D2B time of primary PCI for some countries in Asia is unsatisfactory and calls for the launch of national quality improvement initiatives like those in Western countries. The establishment of an interdisciplinary collaborative team and the obtaining of pre-hospital ECG by EMS were the most successful approaches for improvement. Besides, policymakers in China and India should pay more attention to the delay caused by obtaining the written consent.
Acknowledgment
There was no conflict of interests to be declared. This study was supported by the National Natural Science Foundation of China (No.81770356 & No.81470473), and the Capital Health Research and Development of Special (No.2016-2-4083).
杂志排行
Journal of Geriatric Cardiology的其它文章
- Applicability of the PRECISE-DAPT score in elderly patients with myocardial infarction
- Heart failure mortality compared between elderly and non-elderly Thai patients
- Value of cystatin C in predicting atrial fibrillation recurrence after radiofrequency catheter ablation
- Characterization of coronary atherosclerotic plaques in a homozygous familial hypercholesterolemia visualized by optical coherence tomography
- Contralateral pneumothorax in the subacute phase after pacemaker implantation: lead retention and follow-up
- Hypertension, abnormal blood pressure circadian pattern, and frailty:data from the literature
