Heart failure mortality compared between elderly and non-elderly Thai patients
2019-01-16RungrojKrittayaphongKhemajiraKaraketklangAhthitYindeengamSatitJanwanishstaporn
Rungroj Krittayaphong, Khemajira Karaketklang, Ahthit Yindeengam, Satit Janwanishstaporn
1Division of Cardiology, Department of Medicine, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand
2Department of Medicine, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand
Abstract Objective To investigate heart failure mortality compared between elderly and non-elderly Thai patients. Methods This study included patients at least 18 years of age who were admitted to the hospital with a primary diagnosis of heart failure (ICD-10-TM code: 150.9)during 2008-2012 according to three major Thailand reimbursement systems (civil servant, social security, and universal coverage systems).Patients were categorized into either the elderly group (age > 65 years) or the non-elderly group (age ≤ 65 years). Mortality rate and survival analysis were compared between groups. Demographic, underlying disease and comorbid condition data were collected. Cardiovascular and non-cardiovascular death was also analyzed. Results A total of 201,709 patients were included. The average age of patients was 64.9 ±14.8 years, and the gender proportion breakdown was 84,155 (41.7%) males and 117,554 (58.3%) females. Just over half of patients(107,325 patients; 53.2%) were elderly. Overall mortality rate was 50.8%. The mortality rate at one month, six months, one year, and three years was 11.0%, 24.5%, 32.5%, and 46.3%, respectively. Elderly patients had a higher rate of mortality compared to non-elderly patients with an adjusted odds ratio (OR) of 1.47 (95% CI: 1.46-1.49) for all-cause mortality, an OR of 1.25 (95% CI: 1.23-1.27) for cardiovascular death, and an OR of 1.72 (95% CI: 1.68-1.75) for non-cardiovascular death (all P < 0.001). After adjusting for potential confounders, elderly status remained the second strongest factor associated with increased risk of mortality after heart failure hospitalization following chronic kidney disease. Conclusions The overall mortality rate after heart failure hospitalization was a very high 50.8%. Multivariate analysis revealed elderly status to be an independent predictor of mortality after hospitalization. This finding suggests that improvements are needed related to the quality of care and follow-up given to elderly Thai heart failure patients.
J Geriatr Cardiol 2018; 15: 718-724. doi:10.11909/j.issn.1671-5411.2018.12.006
Keywords: Heart failure; Mortality; Outcomes; Thai population; The elderly
1 Introduction
Heart failure (HF) is a major burden on healthcare systems worldwide. Approximately 1% of population are living with heart failure, and heart failure accounts for 1% of all primary diagnoses that result in hospital admission.[1]The prevalence of heart failure showed an increasing trend even though the prevalence of many cardiovascular diseases showed a decreasing trend due to the increased in aging population.[2-4]The rate of patient death among patients with HF is still very high. In-hospital mortality is estimated to be approximately 7%-10%, with one-year and five-year mortality rates of approximately 10% and 30%, respectively,in both Western and Asian populations.[5-7]Previous studies reported the differences in clinical presentation and outcomes of patients with heart failure when compared between Asian and Western populations.[8,9]As such, the nature and clinical course of heart failure may differ between Asian and Western populations. Data from the Acute Decompensated Heart Failure National Registry (ADHERE)revealed that Asian patients hospitalized due to heart failure were approximately ten years younger earlier than Western patients, and that the disease is more severe in Asians than in Westerners.[10,11]Moreover, the outcome of heart failure was reported to be poorer in elderly patients than in non-elderly patients.[8,9,12]This may, in part, be related to more advanced disease and/or suboptimal treatment relative to the treatment guidelines recommended for this group.[9,13]However, the data of characteristics and outcomes of elderly population is scarce in developing countries.
The aim of this study was to investigate heart failure mortality after heart failure hospitalization compared between elderly and non-elderly Thai patients.
2 Methods
2.1 Study population
This study included patients at least 18 years of age who were hospitalized to the hospital with a primary diagnosis of heart failure during 2008-2012 according to data from three major Thailand reimbursement systems [Civil Servant Medical Benefit scheme (CS), Social Security scheme (SS),and Universal Coverage scheme (UC) systems]. The diagnosis of heart failure was identified by using International Classifications of Disease, Tenth Edition, Thai Modification(ICD-10-TM code: 150.9). Among patients with more than one heart failure hospitalization, only the first hospitalization was included as the index admission. Patients were categorized into either the elderly group (age > 65 years) or the non-elderly group (age ≤ 65 years). The protocol for this study was approved by the Siriraj Institutional Review Board (SIRB), Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand.
2.2 Data collection
Demographic, underlying disease and comorbid condition data were collected from inpatient medical expense claim data. Cardiovascular and non-cardiovascular death were also analyzed. Medical condition diagnosis data were searched and categorized by ICD-10-TM code. The ICD-10-TM codes were then grouped in the same manner as the Center of Medicare and Medicaid services (CMS)ICD-10-TM mapping.
Mortality data, including date and cause of death, was acquired from the Bureau of Registration Administration of Thailand.
2.3 Statistical analysis
All data analyses were performed using SPSS Statistics version 20.0 (SPSS, Inc., Chicago, IL, USA). Descriptive statistics were used to summarize demographic and clinical data. Continuous data are described using mean ± SD, and categorical data are shown using number and percentage.Continuous data were compared using Student’s t-test for unpaired data, and categorical data were compared using chi-square test or Fisher’s exact test. Univariate and multivariate Cox proportional hazards regression analysis was used to determine independent factors that predict death.Mortality rate and survival analysis was compared between elderly and non-elderly population. Kaplan-Meier analysis was used to demonstrate the mortality rate over time. Effect of elderly status on the main outcomes was tested using the interaction test of Cox regression analysis. The results of univariate and multivariate analysis are shown as unadjusted and adjusted hazard ratio (HR) and 95% confidence interval(CI). A P-value of less than 0.05 was considered statistically significant.
3 Results
There were a total of 201,709 patients admitted with a primary diagnosis of heart failure during 2008-2012 in Thailand. The average age was 64.9 ± 14.8 years, and 41.7% of patients were male. Just over half of patients(107,325 patients; 53.2%) were elderly (aged > 65 years).Baseline characteristics of elderly and non-elderly patients are shown in Table 1. Elderly patients were found to be significantly more likely to have many cardiovascular risk factors and comorbid conditions than non-elderly patients except for diabetes and rheumatic heart disease. Mortality data was available for an average of 24.8 ± 20.6 months after the index admission. Among the 201,709 included patients,102,407 (50.8%) died. Comparisons of baseline data between patients who died and patients who survived are shown in Table 2. Deceased patients are more likely to have comorbid conditions and/or risk factors compared to those who survived. Univariate and multivariate analysis for factors associated with increased risk of death are shown in Table 3. Multivariate analysis revealed elderly status to be the second strongest independent predictor of mortality following chronic kidney disease (CKD). Kaplan-Meier analysis of all-cause death for the whole group is shown in Figure 1A. Figure 1B shows that the elderly were significantly more likely to die early after heart failure hospitalization than non-elderly patients. Moreover, the curves diverge over time demonstrating the adverse effect of aging on mortality.
Cause of death data was available only in the 186,062(92.2%) patients covered by the UC reimbursement system.Among those patients, 97,147 (52.2%) patients died. Analysis of cause of death was based on the available data.Table 4 shows cause of death compared between cardiovascular and non-cardiovascular causes in both the elderly and non-elderly groups. Cardiovascular death was observed in 52,534 patients accounting 54.1% of all death. Table 5 shows the rate of all-cause death, cardiovascular death, and non-cardiovascular death at one-month, six-months, oneyear, and three-years. Elderly patients had an increased risk of death compared to non-elderly patients. Elderly status had an impact on non-cardiovascular death more than cardiovascular death. Table 6 shows univariate and multivariate analysis of elderly status as a predicting factor forincreased all-cause, cardiovascular, and non-cardiovascular mortality. After adjusting for potential confounders, elderly status was found to be an independent predictor of both cardiovascular and non-cardiovascular death. The hazard ratio for elderly status resulting in non-cardiovascular death is greater than the hazard ratio for elderly status resulting in cardiovascular death. Figure 2 shows Kaplan-Meier analysis of cardiovascular death and non-cardiovascular death in the whole group (Figure 2A), and compared between the elderly and non-elderly groups (Figure 2B). Similar to Figure 1,the curves in Figure 2B show an increased disparity in the death rate over time between elderly and non-elderly patients, which reflects the persistent effect of elderly status on mortality.

Table 1. Baseline characteristics of elderly and non-elderly heart failure patients.
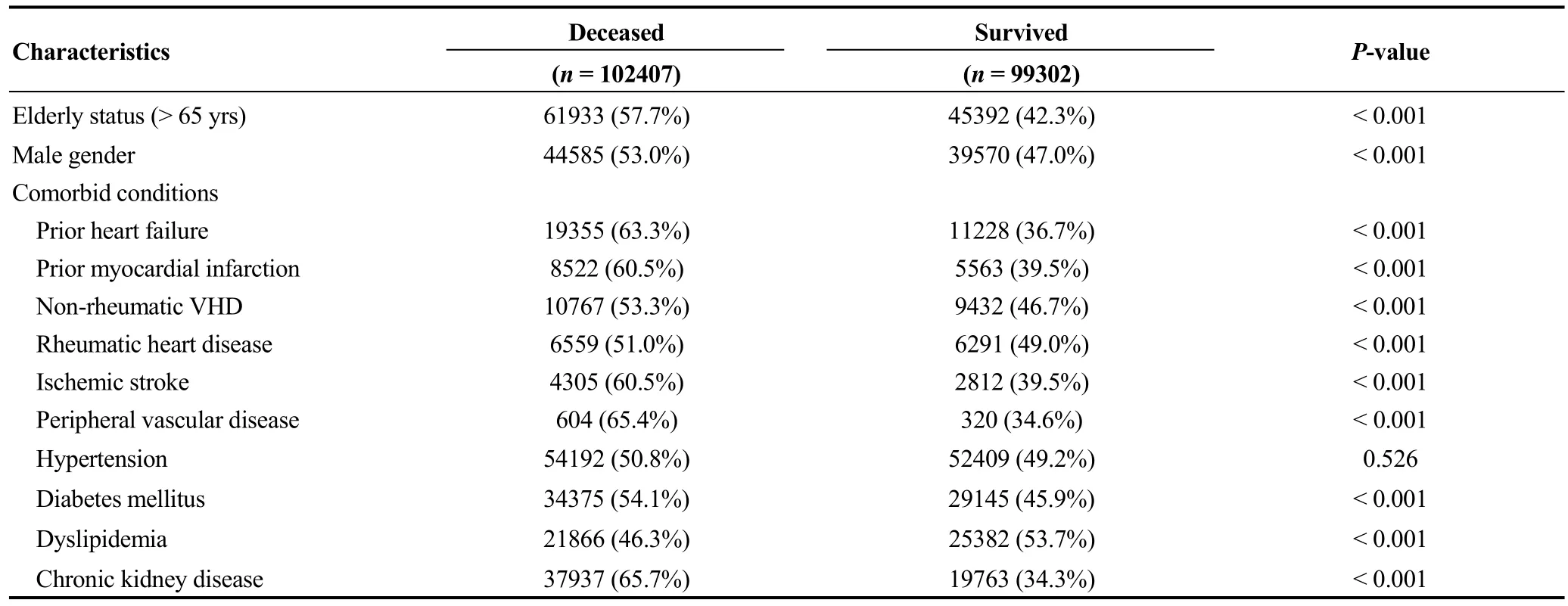
Table 2. Baseline characteristics compared between patients who died and patients who survived during the follow-up.
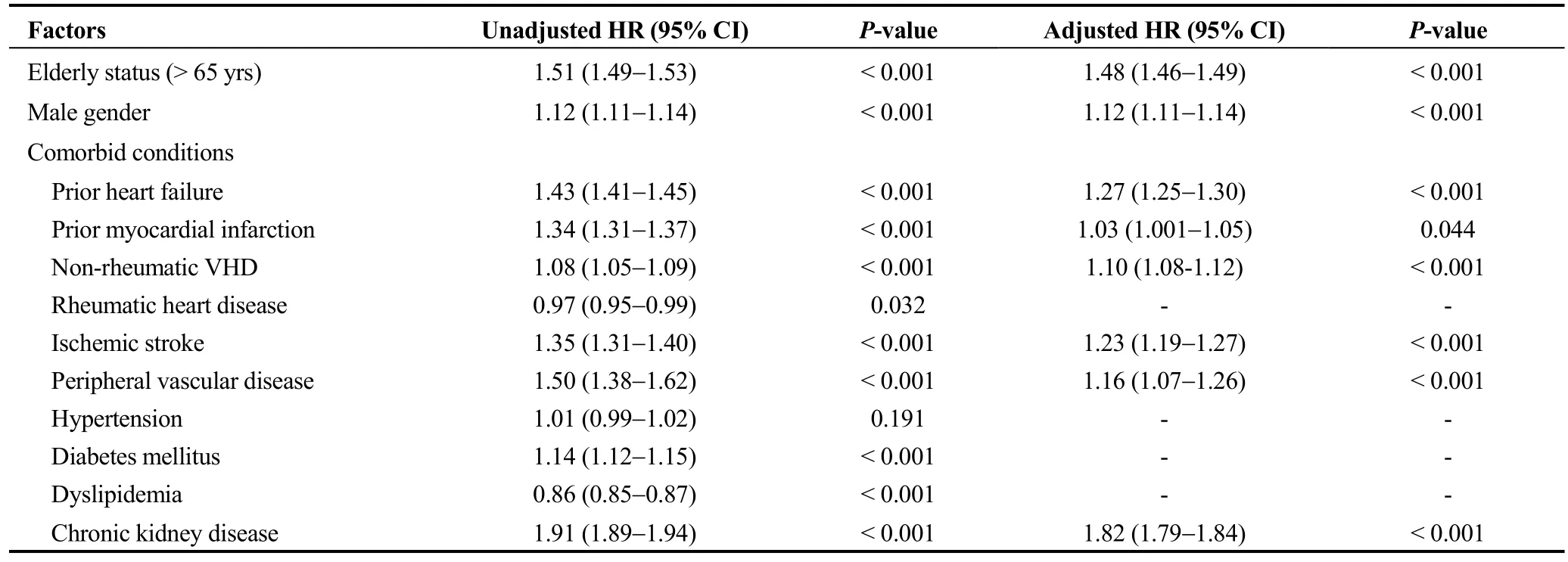
Table 3. Univariate and multivariate analysis for factors associated with increased mortality in Thai heart failure patients.

Figure 1. Kaplan-Meier analysis of all-cause death in the whole group (A), and compared between the elderly and nonelderly (B).
4 Discussion
In this study of 2008-2012 Thailand national claim data in patients admitted with heart failure as the primary diagnosis, we found a mortality rate of 11.0% at one month,24.5% at six months, 32.5% at one year, and 46.3% at three years. After CKD, old age (age > 65 years) was identified as the most important factor determining mortality after hospitalization for heart failure.

Table 4. Causes of death among 186,062 Thai heart failure patients.
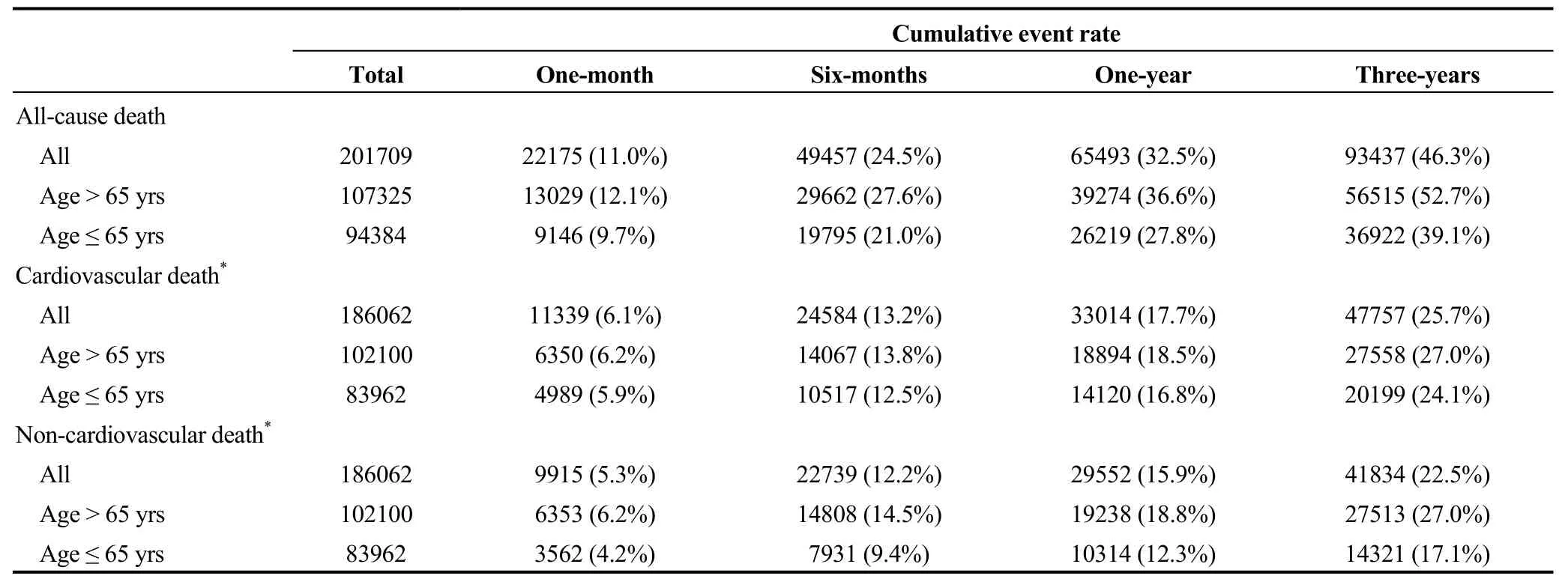
Table 5. All-cause, cardiovascular, and non-cardiovascular death at one month, six months, one year, and three years.
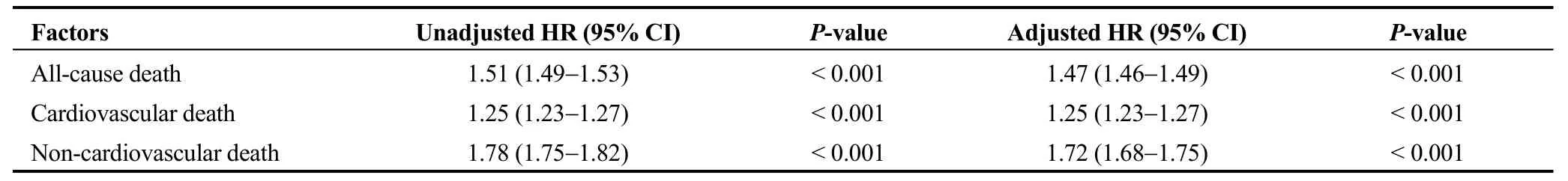
Table 6. Univariate and multivariate analysis of elderly status as a predicting factor for increased all-cause, cardiovascular, and non-cardiovascular mortality.

Figure 2. Kaplan-Meier analysis of cardiovascular death and non-cardiovascular death in the whole group (A), and compared between the elderly and non-elderly groups (B).
Despite the advances in medications and device therapy for heart failure, the mortality rate in patients with heart failure remains high. Overall mortality during heart failure hospitalization and at one year was 7%-10% and 30%,[1,14,15]respectively, among several reports from the United States,[11]Europe,[16,17]and Asia-Pacific countries.[10]In addition, heart failure outcomes may vary among geographic regions, which may reflect a disparity in access to healthcare, healthcare infrastructure, and other factors.[9,18]The International Congestive Heart Failure (INTER-CHF) study revealed different mortality rates among Asian countries,which may be attributable to differences in healthcare systems, access to medication, and environmental factors.[8]The mortality rate in the present study is similar to the rates reported from previous studies.
Heart failure in the Asia-Pacific region presents at approximately ten years younger than the presentation age data reported from Western countries.[10,11,17]Moreover,patients with heart failure from Asia-Pacific countries tend to have more severe condition,[10]and they tend to receive suboptimal standard treatment including inadequate doses of medications and underutilization of implantable cardioverter defibrillator.[13]The prevalence of heart failure increases with age. It is estimated that 70% of the heart failure population that will increase in prevalence in the future will consist of those aged older than 65 years.[2]Previous data showed that the heart failure mortality rate is significantly higher in elderly population than in non-elderly population.[8,19]In addition to our data demonstrating that the mortality rate higher in the elderly compared to the non-elderly group, we also found elderly status to be a factor that significantly predicts patient prognosis after heart failure hospitalization, with an HR and 95% CI of 1.48 and 1.46-1.49,respectively. The most significant factor that determines outcome of heart failure in the present study was chronic kidney disease. Other important factors identified in this study were male gender, prior heart failure hospitalization,prior myocardial infarction, valvular heart disease, ischemic stroke, and peripheral vascular disease.
Elderly status is associated with many risk factors and comorbid conditions that may increase the risk of death,including hypertension, diabetes, prior myocardial infarction, ischemic stroke, peripheral vascular disease, and CKD.[19]However, in our study and after adjusting for these factors in multivariate model, elderly status remained the second strongest independent factor affecting heart failure outcomes after CKD. In our study, the cause of death in patients with heart failure was cardiovascular-related in 54.1% of cases, and non-cardiovascular-related in 45.9% of cases. These proportions are similar to those described in previous reports,[8]although death from unknown causes accounted for a significant proportion of heart failure population in the INTER-CHF study.[8]Elderly status increases the risk of death from both cardiovascular and non-cardiovascular causes. The survival analysis curves representing the cumulative mortality rate between the elderly and non-elderly groups separates early after heart failure hospitalization, and then continues to progressively separate until the end of the follow-up, which reflects the importance and impact of elderly status on heart failure outcome.
4.1 Limitations
There are some mentionable limitations in this study. (1)we had no access to left ventricular ejection fraction (LVEF).Therefore, we were not able to compare elderly patients with heart failure with reduced ejection fraction (HFrEF)with patients with heart failure with preserved ejection fraction (HFpEF). However, a previous study reported no difference in patient prognosis compared between patients with HFrEF and patients with HFpEF.[20](2) The presence of either HFrEF or HFpEF would not have impacted mortality in either of our two study groups. Second, we did not have access to medication or treatment data, so neither of those factors were included in our analysis. (3) Due to the nature of retrospective study using the routine collected database,there may be a limited accuracy in identifying heart failure and other comorbid conditions; and (4) the cause of death given in the death certificate may have a limited accuracy.
4.2 Conclusion
The overall mortality rate after heart failure hospitalization was a very high 50.8%. Multivariate analysis revealed elderly status to be an independent predictor of mortality after hospitalization. This finding suggests that improvements are needed relative to the quality of care and follow-up given to elderly heart failure patients.
Acknowledgments
All authors declare that there is no personal or professional conflict of interest about relating to any aspect of this study. The authors gratefully acknowledge the Central Office for Health Care Information, the National Health Security Office, and the Social Security Office for providing patient data, and Dr. Prapat Suriyaphol for preparing the data for analysis.
杂志排行
Journal of Geriatric Cardiology的其它文章
- Applicability of the PRECISE-DAPT score in elderly patients with myocardial infarction
- Value of cystatin C in predicting atrial fibrillation recurrence after radiofrequency catheter ablation
- Perspective of delay in door-to-balloon time among Asian population
- Characterization of coronary atherosclerotic plaques in a homozygous familial hypercholesterolemia visualized by optical coherence tomography
- Contralateral pneumothorax in the subacute phase after pacemaker implantation: lead retention and follow-up
- Hypertension, abnormal blood pressure circadian pattern, and frailty:data from the literature
