Clinical features and treatment options for mitral regurgitation in elderly inpatients
2018-08-17RuiQiZHUGEXiaoPeiHOUXiLingQIYongJianWUMingZiZHANG
Rui-Qi ZHUGE, Xiao-Pei HOU, Xi-Ling QI, Yong-Jian WU, Ming-Zi ZHANG
Clinical features and treatment options for mitral regurgitation in elderly inpatients
Rui-Qi ZHUGE1, Xiao-Pei HOU1, Xi-Ling QI1, Yong-Jian WU1, Ming-Zi ZHANG2
1Department of Cardiology, Fuwai Hospital, National Center for Cardiovascular Disease, Peking Union Medical College, Chinese Academy of Medical ciences, Beijing, China2Department of Plastic Surgery, Peking Union Medical College Hospital, Peking Union Medical College, Chinese Academy of Medical Sciences, Beijing, China
To summarize clinical characteristics and treatment strategy of Chinese elderly mitral regurgitation (MR) inpatients under the current guidelines, and to identify factors related to treatment options in them.A single center retrospective study was conducted in which patients hospitalized in Fuwai hospital from May 1stof 2014 to April 30 of 2015 with moderate to severe MR assessed by transthoracic echocardiography were enrolled consecutively (= 1741). Patients > 60 years old were grouped as elderly group (= 680) and patients < 60 years were grouped as control group (= 1061). The elderly group was categorized into two subgroups based on surgical status.The mean age of the elderly group was 66.98 ± 5.94 years. The most common reason of MR in elderly group was degenerative MR (41.18%). Atherosclerotic risk factors such as hypertension, diabetes or hyperlipidaemia were more commonly observed in elderly group than the control group (45.44%. 25.17%,< 0.001; 19.56%. 8.48%,< 0.001; 35.29%. 19.51%,< 0.001). Elderly group had higher EuroscoreⅡscore (5.54 ± 2.423.15 ± 1.66), greater left ventricular end diastolic diameter (LVEDD) (57.72 ± 12.3. 57.33 ± 10.19 mm) and a lower surgery rate (54.71%63.91%);< 0.05. Age, left ventricular ejection fraction (LVEF), regurgitation grade, EuroScore-II high risk stratification and having diabetes were identified as factors associated with therapy decisions in elderly MR patients.Valve surgery was denied in 45.29% of elderly MR inpatients. Older age, impaired LVEF, lower regurgitation grade, EuroScore-II high risk stratification, and having diabetes were factors most significantly associated with surgery denial among elderly Chinese inpatients with MR.
J Geriatr Cardiol 2018; 15: 428433. doi:10.11909/j.issn.1671-5411.2018.06.005
Clinical features; Elderly patients; Mitral regurgitation; Treatment
1 Introduction
In industrialized countries, mitral regurgitation (MR) is the second most frequently identified valvular heart disease overall and the leading valvular heart disease in elderly patients over the age of 65 years.[1,2]Severe valvular disease has been reported to be associated with heart failure, arrhythmia and death.[3]As medication therapy is often ineffective for the treatment of advanced MR, surgery is recommended within the 2014 AHA/ACC guidelines for the management of patients with valvular heart disease.[4]However, older adults are often deemed to be a high-risk group for surgery, especially in the presence of comorbidities and frailty.[5]Few reports are available regarding the associations between clinical and echocardiographic features and treatment decisions for elderly MR patients in China. Furthermore, the applicability of the ACC/AHA guidelines has not yet been studied. In the present study, we aimed to assess the clinical features and treatment options for elderly MR inpatients in a single cardiovascular center in China and identify factors associated with treatment decisions.
2 Methods
2.1 Study population
This was a retrospective single-centre study conducted at Fuwai Hospital, National Centre for Cardiovascular Disease, the well-known cardiovascular centre in China. Patients hospitalized in Fuwai hospital from May 1stof 2014 to April 30 of 2015 with moderate to severe MR assessed by transthoracic echocardiography were enrolled consecutively (= 1741). Patients≥ 60 years old were grouped as elderly group (= 680) and patients < 60 years old were grouped as control group (= 1061).
To analyse factors that may influence decisions regarding the treatment of elderly MR patients, we categorized the elderly group into the following two subgroups based on surgical status: the medication group (= 372) and the surgery group (= 308).
2.2 Statistical analysis
Quantitative variables are expressed as the mean ± SD. Comorbidities were analysed individually and in combination using the EuroSCORE-II system. Univariable comparisons were performed using the unpaired Student-test for quantitative variables and the chi-square test for qualitative variables. All data analyses were performed using commercially available statistical analysis software packages (StatView version 4.1, Abacus Concepts, Inc., Berkeley, CA, USA or SPSS version 9.0, SPSS Inc., Chicago, IL, USA). Variables with< 0.05 were entered in a multivariable logistic model and were selected using a backward procedure with a threshold of< 0.05.
3 Results
3.1 Clinical characteristics
The baseline character of elderly MR patients was list in Table 1. The mean age of the 680 elderly patients was 66.98 ± 5.94 years. Of these patients, 159 (23.38%) were aged 70–80 years, and 30 (4.41%) were> 80 years. Male patients accounted for 58.99% in the elderly group. In total, 275 (40.44%) elderly MR patients were graded as severe regurgitation by echocardiography. Among the elderly MR, degenerative aetiologies were most commonly identified (41.18%), followed by rheumatic aetiologies and ischaemic aetiologies. 45.29% elderly patients were denied surgery, and surgery denial rate increased with age (Figure 1). Comparisons between different age groups were showed in Table 2.
3.2 Clinical characteristics and treatment decision comparisons
The two groups differed significantly by aetiology (Table 3). Degenerative mitral regurgitation (DMR) was most commonly observed in both the elderly group and control group, but DMR accounted for a greater percentage of cases in the elderly group (41.18%. 33.74%,< 0.001). No significant between-group differences were identified in MR grade or NYHA class.

Table 1. Baseline characteristics and echocardiographic parameters of elderly group and control group.
Data presented as mean ± SD or(%).*In primary MR, the pathology of ≥ 1 of the components of the valve (leaflets, chordae tendineae, papillary muscles, annulus) causes valve incompetence with systolic regurgitation;#In secondary MR, the mitral valve is usually normal.The abnormal and dilated left ventricle caused by cardiovascular disease or related MI (ischemicMR) leads to papillary muscle displacement, which in turn results in leaflet tethering with associated annular dilation. LVEF: left ventricular ejection fraction; MI: myocardial infarction; MR: mitral regurgitation.

Figure 1. The association between age stratification and treatment option in MR inpatients. MR: mitral regurgitation.

Table 2. Clinical characteristics and surgery status of older patients.
Data presented as mean ± SD or(%). LVEF: left ventricular ejection fraction; MR: mitral regurgitation.
Atherosclerotic risk factors such as hypertension, diabetes or hyperlipidaemia were more commonly observed in the elderly group than control group (45.44%. 25.17%,< 0.001; 19.56%. 8.48%,< 0.001; 35.29%. 19.51%,< 0.001). The mean EuroSCORE-II index was much higher than that observed in control group members (5.54 ± 2.42. 3.15 ± 1.66,< 0.001). Remarkably, more patients were assessed as being high risk based on the EuroSCORE risk stratification in the elderly group than the control group (41.3%. 8.29%,< 0.001). An impaired left ventricular ejection fraction (LVEF) was identified in 57.79% of the elderly patients, which was a much higher prevalence than that identified in the control group (47.22%,< 0.001). Mean left ventricular end diastolic diameter (LVEDD) was greater in the elderly group than the control group (57.33 ± 10.19. 57.72 ± 12.37 mm,< 0.001).
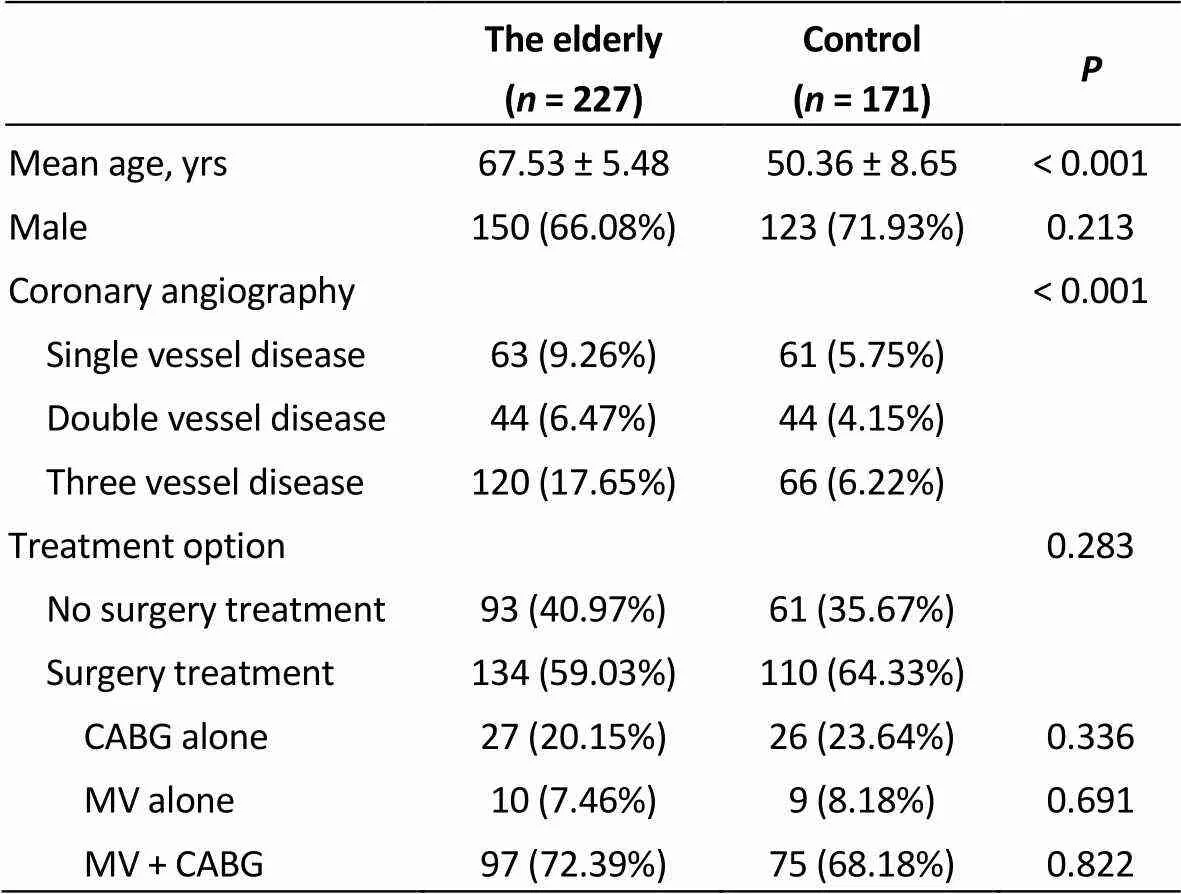
Table 3. Characteristics and treatment of MR patients with primary indications for cardiac revascularization in both groups.
Data presented as mean ± SD or(%). CABG: coronary artery bypass grafting; MR: mitral regurgitation; MV: mitral valve.
Of the 680 elderly MR patients included in this study, 308 were denied surgery (45.29%), which was much higher than the rate of denial observed in the control group (45.29%. 36.10%,< 0.001). No difference was observed in operative methods (repair or replacement,= 0.293). Among patients who underwent valve replacement, bioprosthetic valves were more often used than mechanical valves in the elderly group than in the control group (53.88%. 18.67%,< 0.001). No significant between-group difference was identified in the rate of in-hospital mortality.
Two hundred and twenty seven patients in elderly group and 171 patients in the control group had primary indications for cardiac revascularization and their coronary angiography results differed from those of control group (< 0.001). Of these 227 elderly MR patients, 134 (59.03%) underwent surgery, in which 27 (20.15%) had coronary artery bypass grafting (CABG) alone, 10 (7.46%) had mitral valve (MV) surgery alone and 97 (72.39%) had concomitant surgical revascularization with MV surgery (Table 3).
3.3 Factors associated with treatment decisions in elderly MR patients
Clinical features of medication subgroup and surgery group were compared in univariate analysis and the results were presented in Table 4. In the multivariate analysis, the characteristics associated with increased probability of undergoing surgery among elderly MR patients were severe regurgitation and normal LVEF. The factors associated with decreased probability of undergoing surgery were increased age, diabetes and EuroSCORE-II high risk stratification (Table 5).
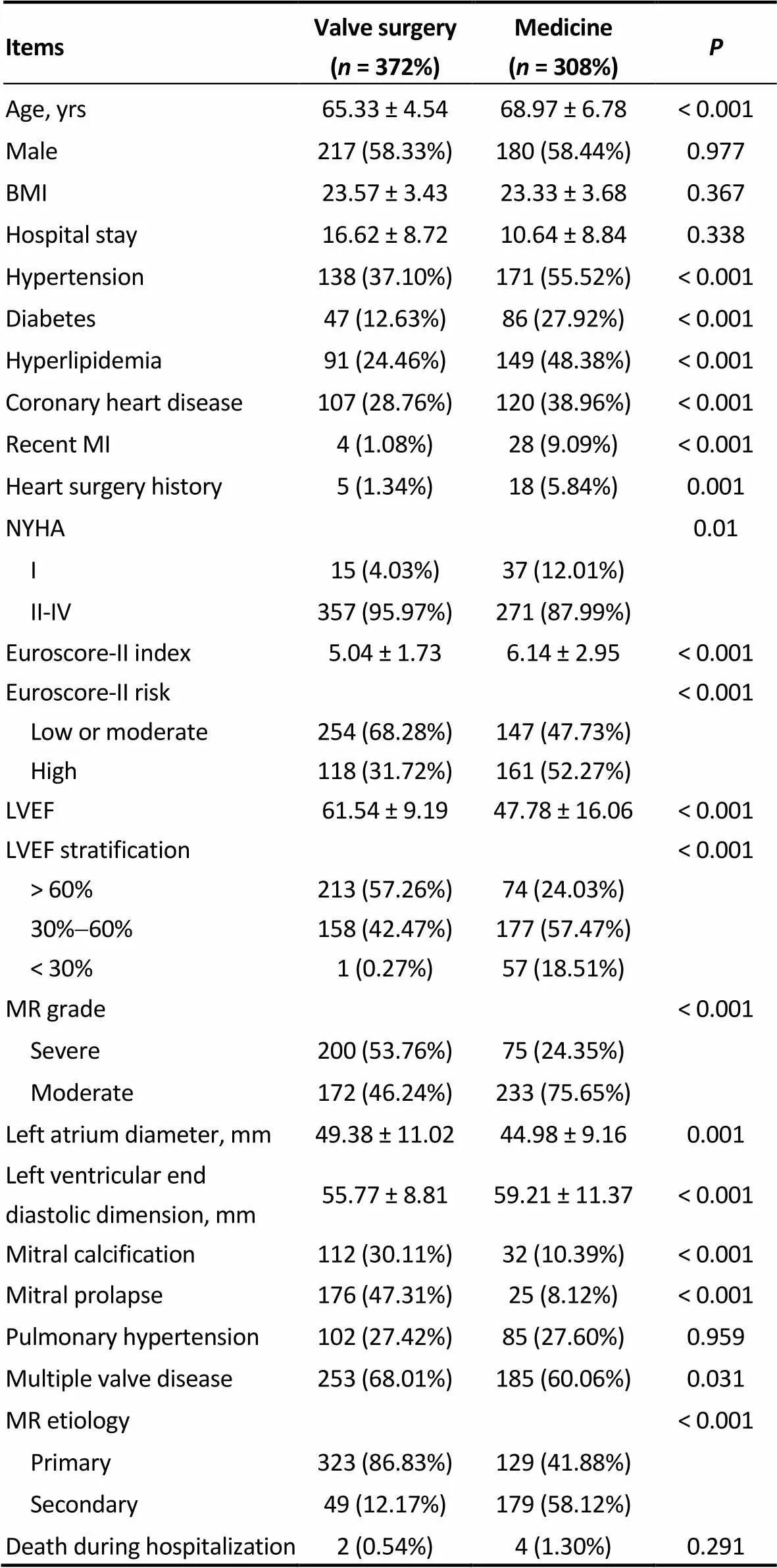
Table 4. Baseline clinical characteristics and echocardiographic parameters of valve surgery sub-group and medicine sub- group of elderly patients.
Data presented as mean ± SD or(%). BMI: body mass index; LVEF: left ventricular ejection fraction; MI: myocardial infarction; MR: mitral regurgitation.
4 Discussion
Valvular heart disease is a common disease that may greatly influence quality of life and survival in elderly patients. MR has been identified as the most frequently diagnosed valvular heart disease in elderly people in industrialized countries.[2]In this study, we found that elderly MR patients accounted for a high proportion (39.06%) of all MR patients included, with patients aged over 80 years constituting 4.41%.
In this study, we observed that even under the current guidelines, the rate of surgery in elderly MR patients was far from that which would be expected, as many factors may influence treatment decisions. In this single-centre study, the rate of surgical intervention of mitral valve was only 60.31% in the included 1741 MR patients overall, and even lower in the elderly group (54.71%). This finding was consistent with a previous study conducted in Western countries.[6]In addition to being of advanced age, the elderly patients included in this study also had a higher EuroSCORE grade, with higher comorbidity and coronary heart disease (CHD) prevalence rates and lower LVEF when compared with control group patients. Thus, in this study, we observed that elderly patients were at greater risk prior to treatment initiation, which may be the reason for the lower rate of surgery observed in this population. We identified factors influencing decisions regarding the treatment of elderly patients; these factors included age, regurgitation degree, LVEF, EuroSCORE-II risk stratification, and having diabetes and multiple valve diseases. These results are consistent with those identified in a previous study of MR,[6]and another study of aortic stenosis in the elderly, particular in terms of older age and impaired LVEF.[7]
Regurgitation degree was most strongly associated with the decision to operate. Although there has been controversy regarding the optimal timing of intervention in moderate MR patients, consensus suggests that valvular surgery should be advised in severe MR patients, as shown by the corresponding class I recommendation in the ACC/AHA guidelines.[4]In this study, we observed that severe MR patients were more likely to undergo surgery than moderate MR patients. Nevertheless, the rate of surgery in severe patients was not ideal. A previousstudy reported that approximately 50% of severe MR patients were denied surgery before the current guidelines were implemented.[6]Of the elderly severe MR patients (=275) included in this study, 75 (27.27%) did not undergo surgery. This finding was somewhat understandable, as the rate of long-term mortality has been found to increase with MR severity and was estimated to be 42% at 5 years’ follow-up in patients with severe regurgitation in a previous study.[8]
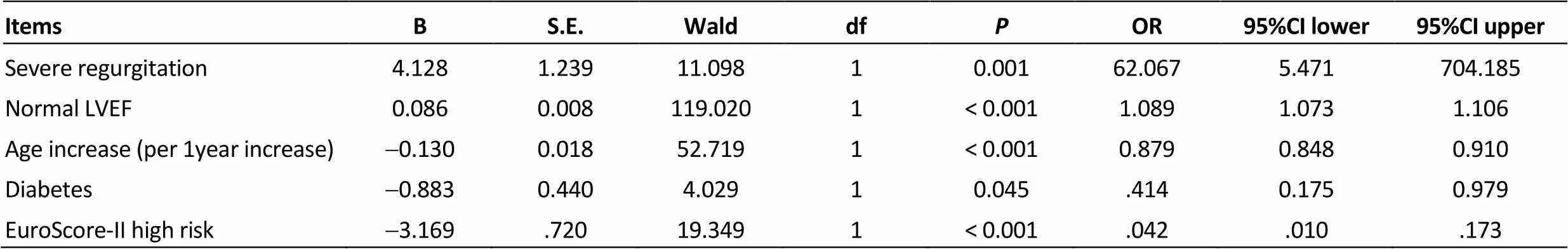
Table 5. Factors associated with the treatment option of surgery (multivariable analysis).
LVEF: left ventricular ejection fraction.
Another study showed that age was an important factor influencing treatment decisions in general MR patients. We would like to note that, in this study, age was an important influencing factor, even among elderly patients. As patients became older, their rate of surgery decreased (Figure1). Actually, only a moderate increase in the risk of surgery has been identified in patients <80 years old.[5]This finding highlights the importance of the diagnosis of MR in elderly patients before they become too old to undergo surgery. Based on the results of the OxVALVE Population Cohort Study,[9]the early diagnosis rate was far from that which would be expected, as in the overall elderly cohort with no history of VHD, 6.4% were diagnosed with moderate to severe VHD for the first time.
LVEF was associated with decisions regarding the treatment of elderly and severe MR patients (Figure2). Low LVEF has been identified as a predictive factor for spontaneous mortality,[10]post-operative mortality,[11]and post-operative LVEF[12]in MR. Despite the higher operative risk and less satisfying long-term results observed in impaired LVEF patients relative to those with normal LVEF, patients with moderately impaired left ventricular function may benefit from surgery since particularly poor outcomes have been observed in association with medication therapy in this patient population.[13]However, in this study, we observed that patients with moderately impaired LVEF had a rate of surgery that was less than 50%,which suggests the use of a more conservative treatment strategy in this group.
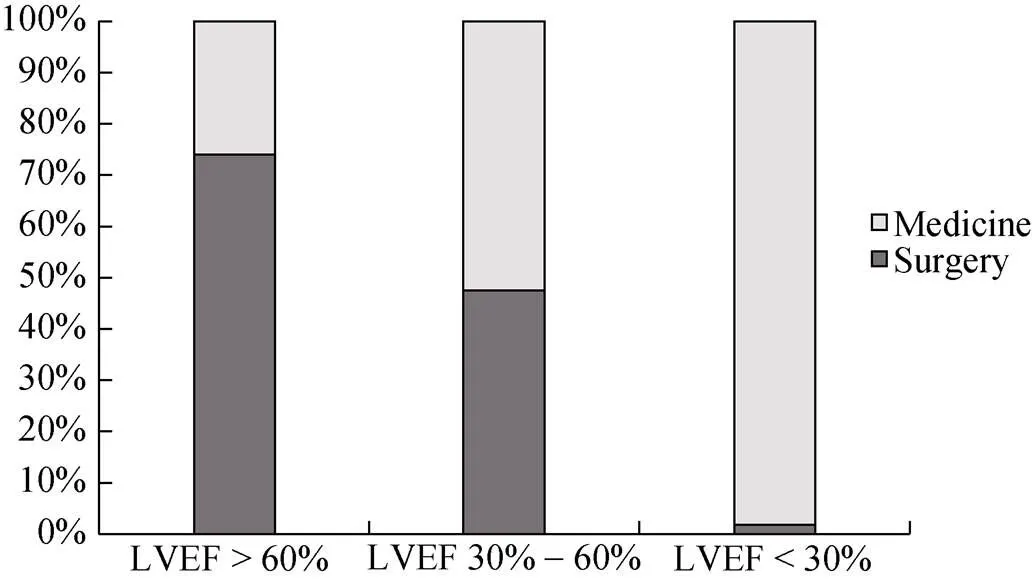
Figure 2. The association between LVEF stratification and treatment option in elderly MR inpatients. LVEF: left ventricular ejection fraction; MR: mitral regurgitation.
EuroScore-II high risk, which indicates presence of various comorbidities, was in association with a decision not to operate. This decision may be understandable since having an increased EuroSCORE index had been found to have a negative impact on life expectancy,[14]and most comorbidities are also associated with increased operative risk.[15]The high prevalence of comorbidities may be one explanation for the high proportion of patients who were denied surgery in the present study.
The presence of diabetes was also a factor that influenced treatment decisions in the elderly group. The relationship between diabetes and MR is under heat debate. On the one hand, diabetes can exert a bad influence on recovery after surgery and study showed diabetes predicted MR progression after MV repair.[16]On the other hand, new study showed that MR is a common pathologic condition in patients with type 2 diabetes and is independently associated with an increased risk of both all-cause and cardiovascular mortality.[17]
While degeneration has been identified as the most common aetiology of valvular disease in developed countries,[1,2]rheumatic disease has been consistently identified as the leading reason for valvular disease in developing countries over the past several decades.[2]However, in this study, degenerative mitral disease was the leading aetiology of MR in both elderly group and control group patients. In addition, degenerative MR was more frequently observed in the elderly group, with a prevalence rate of 41.18%. These results are in accordance with statistics derived based on a Chinese adult surgery database, which showed that the incidence of degenerative valve disease has increased dramatically since the 1990s and that rheumatism may no longer be the most common reason for valve disease.[18]To a large extent, this transition may have occurred due to vast improvements in the diagnosis, treatment and prevention of rheumatic diseases, which may also be increasing due to the increasing number of aged people in China.
Ischaemic MR was another type of MR frequently observed in this Chinese cohort. The abnormal and dilated left ventricle caused by CHD or related MI (ischemic MR) leads to papillary muscle displacement, which in turn results in leaflet tethering with associated annular dilation. Among elderly patients, the prevalence of ischaemic MR was especially high at 18.24%. In this study, the prevalence rates of coronary heart disease, myocardial infarction history and atherosclerotic risk factors were higher in the elderly group, and these results were likely related to the higher incidence of ischaemic MR observed in the elderly group. Coronary artery disease may be associated with increased operative risk, but its weight in the decision to operate could hardly be objectively assessed since the performance of coronary angiography is also closely linked to the decision to operate. In this study, most MR patients combined with CHD underwent MV surgery with concomitant surgical revascularization, which was consistent with the principle of ACC/AHA guidelines about ischaemic MR surgery recommendations.
In conclusion, many elderly patients with more advanced age, worse heart function and more comorbidities may not be able to undergo surgery in China. Novel technologies based on percutaneous intervention, such as Mitraclip,[19]are rapidly evolving and currently recommended for high risk patients on whom ordinary surgeries cannot be performed in western countries (IIB recommendation).[4]In China, such interventional technologies are not yet prevalent but may serve as a good option. As based on this study, the elderly MR patients who were considered high risk was high and is likely to continue increasing. On the other hand, early diagnosis of MR is highly important in elderly patients to improve prognosis. General transthoracic echocardiography screening regularly in elderly population could serve as a useful measure to improve early diagnosis rate, especially in rural area of China.
This study was meaningful in that it provided information regarding the diagnosis and treatment of elderly MR patients and to some extent remedied knowledge gaps in this field in China. However, the results of this study are not generalized to all of China. A prospective, multi-centre study should be conducted in the future to further explore survival and prognosis in elderly MR patients and provide a more precise view of treatment trends.
Acknowledgments
This work was supported by National Key Technology Support Program of China (2015BAI12B02). There was no conflict of interests to be declared.
1 Iung B, Baron G, Butchart EG,. A prospective survey of patients with valvular heart disease in Europe: the Euro Heart Survey on valvular heart disease.2003; 24: 1231–1243.
2 Iung B, Vahanian A. Epidemiology of acquired valvular heart disease.2014; 30: 962–970.
3 Green P, Rosner GF, Schwartz A. Valvular heart disease in older adults: evolving technology to meet the needs of aging patients.2013; 9: 205–215.
4 Nishimura RA, Otto CM, Bonow RO,. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association task force on practice guidelines.2014; 63: 2438–2488.
5 Ambler G, Omar RZ, Royston P,. Simple risk stratification model for heart valve surgery.2005; 112: 224–231.
6 Mirabel M, Iung B, Baron G,. What are the characteristics of patients with severe, symptomatic, mitral regurgitation who are denied surgery?2007; 28: 1358–1365.
7 Iung B, Cachier A, Baron G,. Decision making in elderly patients with severe aortic stenosis: why are so many denied surgery?2005; 26: 2714–2720.
8 Enriquez-Sarano M, Avierinos JF, Messika-Zeitoun D,. Quantitative determinants of the outcome of asymptomatic mitral regurgitation.2005; 352: 875–883.
9 D’Arcy JL, Coffey S, Loudon MA. Large-scale community echocardiographic screening reveals a major burden of undiagnosed valvular heart disease in older people: the OxVALVE Population Cohort Study.2016; 37: 3515–3522.
10 Avierinos JF, Gersh BJ, Melton LJ,. Natural history of mitral valve prolapse in the community.2002; 106: 1355–1361.
11 Enriquez-Sarano M, Tajik AJ, Schaff HV,. Echocardiographic prediction of survival after surgical correction of organic mitral regurgitation.1994; 90: 830–837.
12 Enriquez-Sarano M, Tajik AJ, Schaff HV,. Echocardiographic prediction of left ventricular function after correction of mitral regurgitation: results and clinical implications.1994; 24: 1536–1543.
13 Ling LH, Enriquez-Sarano M, Seward JB,. Clinical outcome of mitral regurgitation due to flail leaflet.1996; 335: 1417–1423.
14 Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classify- ing prognostic comorbidity in longitudinal studies: development and validation.1987; 40: 373–383.
15 Roques F, Nashef SA, Michel P, Gauducheau E,. Risk factors and outcome in European cardiac surgery: analysis of the EuroSCORE multinational database of 19030 patients.1999; 15: 816–823.
16 Tatum JM, Bowdish ME, Mack WJ,. Outcomes after mitral valve repair: A single-center 16-year experience.2017; 154: 822–830.e2.
17 Rossi A, Zoppini G, Benfari G,. Mitral regurgitation and increased risk of all-cause and cardiovascular mortality in patients with type 2 diabetes.2017; 130: 70–76.
18 Rao C, Zhang H, Gao H,. The chinese cardiac surgery registry: design and data audit.2016; 101: 1514–1520.
19 Orban M, Braun D, Orban M,. Established interventions for mitral valve regurgitation.2016; 41: 19–25.
Yong-Jian WU, Department of Cardiology, Fuwai Hospital, National Center for Cardiovascular Disease, Peking Union Medical College, Chinese Academy of Medical Sciences, No.167 North Lishi Road, Xicheng District, Beijing, China. E-mail: ruiqizhuge@163.com.
August 4, 2017
January 10, 2018
January 25, 2018
June 28, 2018
杂志排行
Journal of Geriatric Cardiology的其它文章
- “Malignant” right coronary artery presenting as an ST-segment elevation myocardial infarction—a case report
- Influenza vaccination in acute coronary syndromes patients in Thailand: the cost-effectiveness analysis of the prevention for cardiovascular events and pneumonia
- The trend of change in catheter ablation versus antiarrhythmic drugs for the management of atrial fibrillation over time: a meta-analysis and meta-regression
- Early mortality and safety after transcatheter aortic valve replacement using the SAPIEN 3 in nonagenarians
- Depression and chronic heart failure in the elderly: an intriguing relationship
- CIED implantation in elderly patients: a single-center experience
