“Malignant” right coronary artery presenting as an ST-segment elevation myocardial infarction—a case report
2018-08-17CherisseBaldeoKaranSeegobinDmitryYaranovFabianaRollini
Cherisse Baldeo, Karan Seegobin, Dmitry Yaranov, Fabiana Rollini
“Malignant” right coronary artery presenting as an ST-segment elevation myocardial infarction—a case report
Cherisse Baldeo1,*, Karan Seegobin1, Dmitry Yaranov2, Fabiana Rollini2
1Department of Internal Medicine, University of Florida, Jacksonville, Florida, USA2Department of Cardiology, University of Florida, Jacksonville, Florida, USA
J Geriatr Cardiol 2018; 15: 467468. doi:10.11909/j.issn.1671-5411.2018.07.001
Anomalous; Myocardial infarction; Right coronary artery
ST elevation on ECG in the setting of mesenteric ischemia has been reported.[1]From three prior reports, only one had a true ST elevation myocardial infarction (STEMI) coexisting with mesenteric ischemia. In patients with a strong cardiac history, distinguishing between these two conditions can be challenging. We present the case of a 79-year-old Caucasian female presented with 3-h history acute-onset epigastric pain. Medical history was significant for ischemic heart disease with prior coronary artery bypass grafts, ischemic cardiomyopathy with reduced ejection fraction and an implantable defibrillator device, and atrial fibrillation (on apixaban and sotalol). On examination, blood pressure 100/52 mmHg, pulse 85 beats/min, respiratory rate 22 beats/min, SpO2 99% and temperature 36.8°C. Examination revealed normal heart sounds with generalised abdominal tenderness to palpation without guarding or rebound and normal bowel sounds. Although a CT abdomen was initially ordered, prior to completion, she developed acute-onset chest pain with associated dyspnea. ECG showed atrial fibrillation with new ST elevations in the inferior leads (Figure 1). Troponins were elevated at 0.28 (0.00-0.04 ng/mL) as was lactic acid at 3.1 (0.7-2.7 mmol/L). Renal and liver function tests were all within normal limits. A decision was made to emergently activate the cardiac lab. Emergent left heart catheterization showed native coronary artery disease with patent grafts and no evidence of new obstructive disease. No intervention was performed. Left ventriculography showed apical ballooning and hyperkinetic base (Figure 2) suggestive of stress cardiomyopathy (Takotsubo), with estimated ejection fraction (EF) of 40%-45%. After return from the cardiac catherization lab, CT abdomen performed showed dilated caecum with air in adjacent ileocolic vessels with foci of air in the lower abdomen (Figure 3).
Exploratory laparotomy revealed ischemic caecum which was resected. Pathology showed extensive necrosis and acute on chronic inflammation. Repeat ECG in the post- operative period showed resolution of ST elevations, and her troponins trended down.
She had a stormy hospital course requiring repeat exploratory laparotomy for resection of necrotic bowel. Following this, she clinically improved postoperatively and was discharged to a rehab facility. She remained chest pain free and repeat echocardiogram prior to hospital discharge showed an improved left ventricular function with EF of 45%-50%. It is known that mesenteric ischemia can present with STEMI and stress cardiomyopathy.[1,2]Physician awareness about this is important with early identification of the abdominal and cardiac emergency being critical, as there has been a prior report of both STEMI and mesenteric ischemia coexisting simultaneously.[3]The likelihood of stress-induced cardiomyopathy was high in this woman who was undergoing severe physiologic stress while displaying left ventricular wall-motion abnormalities with associated ECG changes. In patients with significant risk factors for myocardial infarction as seen in our case; chest pain with new ST elevation on ECG and positive troponins cannot be disregarded. It is important to make a distinction between myocardial injury in association with stress (as in our case) and myocardial infarction in association with thrombus (a much worse prognosis). However, where there exists this diagnostic dilemma, chest pain with convincing evidence of possible STEMI may trump the treatment for mesenteric ischemia. In such a high cardiac risk patient, we felt it prudent to evaluate for a possible STEMI first and therefore activate the cardiac catherization lab. Our patient’s symptoms of “acute abdomen” did not appear severe enough to warrant urgent surgical intervention, whereas the chest pain and electrocardiographic changes (supported by rising tro-ponin levels) created strong clinical suspicion of acute coronary syndrome. In a busy clinical environment, with little time to make decisions, physicians are faced with great challenge in differentiating between the two emergencies. Where ‘time is heart,’ there must be strong evidence not to pursue cardiac catherization when faced with such a clinical dilemma.
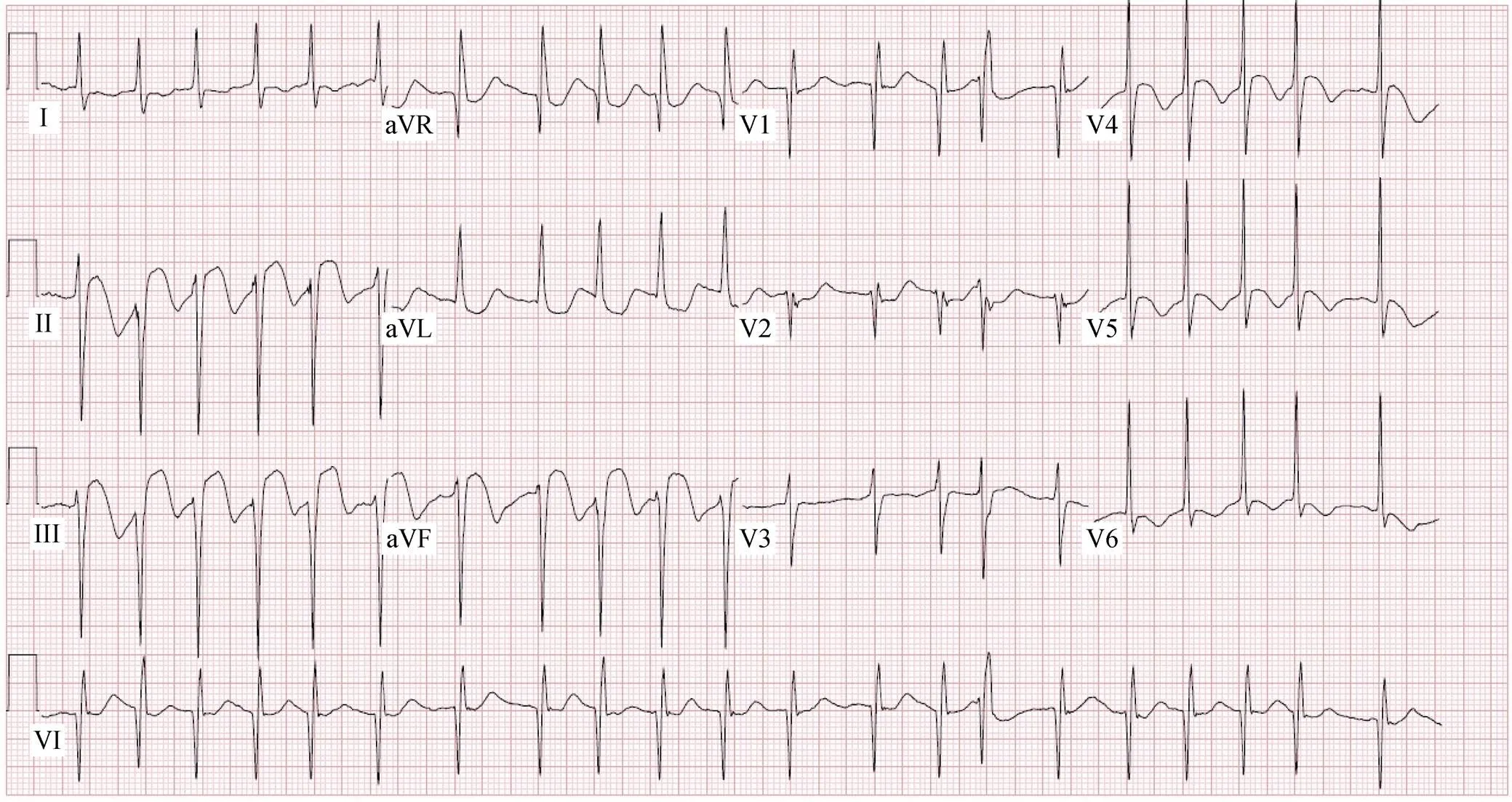
Figure 1. ECG showing atrial fibrillation with new ST elevation in the inferior leads.
Figure 2. Left ventriculography showing apical ballooning and hyperkinetic base suggestive of stress cardiomyopathy.
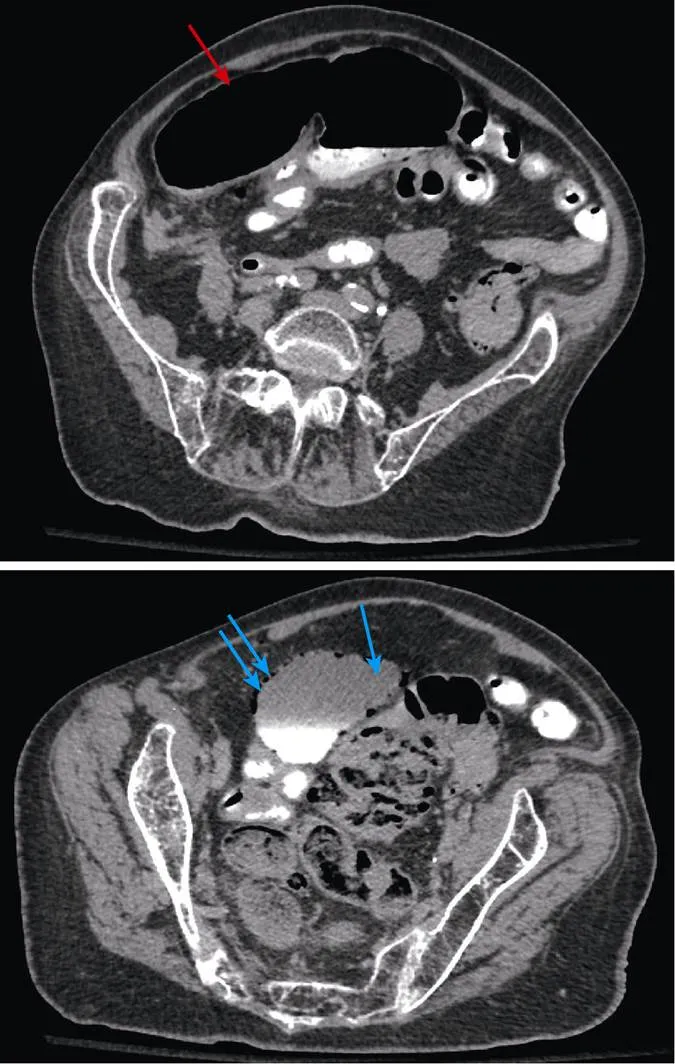
Figure 3. CT abdomen which showing dilated caecum (red arrow) with air in the adjacent ileocolic vessels and foci of extraluminal gas in lower abdomen (blue arrows).
Acknowledgements
The authors declare that there is no conflict of interestregarding the publication of this paper.
1 Yeh YT, Tu CM, Wu YW. Mesenteric ischemia mimicking ST-segment elevation myocardial infarction.2015; 373: 780-781.
2 Koci F, Eltibi R, Hadley M, Kumar D. Necrotic bowel induces takotsubo-like myocardial injury.2014; 41: 638-640.
3 The Heart of the Matter.2016; 18 (Suppl. B): B51–B57.
cherrieb21@hotmail.com
杂志排行
Journal of Geriatric Cardiology的其它文章
- Influenza vaccination in acute coronary syndromes patients in Thailand: the cost-effectiveness analysis of the prevention for cardiovascular events and pneumonia
- The trend of change in catheter ablation versus antiarrhythmic drugs for the management of atrial fibrillation over time: a meta-analysis and meta-regression
- Early mortality and safety after transcatheter aortic valve replacement using the SAPIEN 3 in nonagenarians
- Depression and chronic heart failure in the elderly: an intriguing relationship
- CIED implantation in elderly patients: a single-center experience
- Use of the reported Edmonton frail scale in the assessment of patients for transcatheter aortic valve replacement: a possible selection tool in very high-risk patients?
