老年冠心病慢性心力衰竭患者血浆同型半胱氨酸与心脏功能的相关性
2018-01-02马丽娜钱玉英
朱 红,马丽娜,刘 川,杨 伟,李 耘,钱玉英
·临床研究·
老年冠心病慢性心力衰竭患者血浆同型半胱氨酸与心脏功能的相关性
朱 红,马丽娜,刘 川,杨 伟,李 耘,钱玉英
目的观察老年冠状动脉粥样硬化性心脏病(冠心病)慢性心力衰竭(chronic heart failure, CHF)患者血浆同型半胱氨酸(Hcy)的水平与心脏功能的相关性。方法选择老年冠心病62例作为冠心病组,根据美国纽约心脏病学会(NYHA)心功能分级标准,分为CHF组(42例)和心功能代偿组(20例),其中CHF组又分为NYHA Ⅱ级组和NYHA Ⅲ~Ⅳ级组;选择同期体检健康的老年人20例作为对照组。比较各组血浆Hcy、N末端B型脑钠肽前体(NT-proBNP)、左室射血分数(LVEF)和左室舒张末期内径(LVEDD)变化,分析血浆Hcy水平与NT-proBNP、LVEF和LVEDD的相关性。结果与对照组比较,代偿组及CHF组血浆Hcy、NT-proBNP水平及CHF组LVEDD均升高,且CHF组LVEF降低,差异均有统计学意义(P<0.05);与代偿组比较,CHF组血浆Hcy、NT-proBNP水平及LVEDD均升高,LVEF降低,差异均有统计学意义(P<0.05)。NYHA Ⅱ级组与NYHA Ⅲ~Ⅳ级组血浆Hcy及NT-proBNP水平比较差异均有统计学意义(P<0.05)。老年CHF患者血浆Hcy水平与NT-proBNP、LVEDD呈正相关,与LVEF呈负相关。结论老年冠心病CHF患者血浆Hcy水平明显升高,且与NT-proBNP、LVEF和LVEDD呈明显相关性,可作为反映心力衰竭严重程度的参考指标。
冠心病;心力衰竭;同型半胱氨酸
随着社会老年人口比例增加,钙化性老年心脏瓣膜病、慢性心力衰竭(chronic heart failure, CHF)已成为老年人入院的主要原因,给社会带来巨大的经济负担[1-2],故明确危险因素并加以干预是防治CHF的关键。CHF患者血浆同型半胱氨酸(Hcy)水平升高,是CHF的危险因素,且与不良预后相关[3-5]。N末端B型脑钠肽前体(NT-proBNP)是诊断CHF的重要生物标志物之一[6-7]。本研究通过测定老年冠心病CHF患者血浆Hcy和NT-proBNP水平变化,探讨其相关性及与心脏功能的关系。
1 资料与方法
1.1研究对象 选取2013年10月—2015年9月我院收治的冠心病62例作为冠心病组,选择同期体检健康的老年人20例作为对照组。根据美国纽约心脏病学会(NYHA)心功能分级标准,冠心病组分为CHF组(其中NYHA Ⅱ级组24例,NYHA Ⅲ~Ⅳ级18例)和心功能代偿组(即代偿组,为NYHA I级组20例)。纳入标准:①有明确心肌梗死病史;②冠状动脉造影或CT动脉造影证实冠状动脉狭窄>50%;③有典型的心绞痛症状或心电图改变。排除CHF急性发作、急性冠脉综合征、血压控制不稳(收缩压>180 mmHg,舒张压>110 mmHg)、糖尿病、恶性肿瘤、严重肝肾功能不全及自身免疫性疾病等。
1.2观察指标及研究方法 记录患者的年龄、性别、身高及体重指数(BMI)。心脏超声检查采用Philip Ie33型心脏彩色多普勒超声诊断仪,记录患者左室射血分数(LVEF)和左室舒张末期内径(LVEDD)。禁食12 h,次日清晨抽取肘静脉血,采用全自动生化分析仪测定血浆Hcy、肌酐、血糖、甘油三酯和低密度脂蛋白胆固醇水平。NT-proBNP测定采用日本三菱公司生产的PATHFAST系统分析仪并使用化学免疫发光法进行检测。

2 结果
2.1一般资料比较 两组年龄、收缩压、舒张压、BMI、血糖、血肌酐、甘油三酯和低密度脂蛋白胆固醇比较差异无统计学意义(P>0.05),具有可比性,见表1。

表1 老年冠心病慢性心力衰竭两组一般资料比较
注:CHF指慢性心力衰竭,BMI指体重指数
2.2血浆Hcy、NT-proBNP、LVEF及LVEDD水平比较 与对照组比较,代偿组及CHF组血浆Hcy、NT-proBNP水平及CHF组LVEDD均升高,且CHF组LVEF降低,差异均有统计学意义(P<0.05);与代偿组比较,CHF组血浆Hcy和NT-proBNP水平及LVEDD升高,LVEF降低,差异有统计学意义(P<0.05),见表2。

表2 老年冠心病慢性心力衰竭两组血浆Hcy、NT-proBNP、LVEF及LVEDD水平比较
注:CHF指慢性心力衰竭,Hcy指同型半胱氨酸,NT-proBNP指N末端B型脑钠肽前体,LVEF指左室射血分数,LVEDD指左室舒张末期内径;与对照组比较,aP<0.05,bP<0.01;与代偿组比较,cP<0.05,dP<0.01
2.3不同心功能分级的CHF组血浆Hcy和NT-proBNP水平比较 NYHA Ⅱ级组血浆Hcy及NT-proBNP水平分别为(16.58±10.12)μmol/L、(1782.79±839.63)ng/L,NYHA Ⅲ~Ⅳ级组分别为(52.07±18.81)μmol/L、(2686.95±1486.51)ng/L,比较差异均有统计学意义(P<0.05)。
2.4老年CHF血浆Hcy水平与NT-proBNP、LVEF和LVEDD的相关性分析 Pearson相关性分析显示,老年CHF患者血浆Hcy水平与NT-proBNP、LVEDD呈正相关,与LVEF呈负相关,见图1。
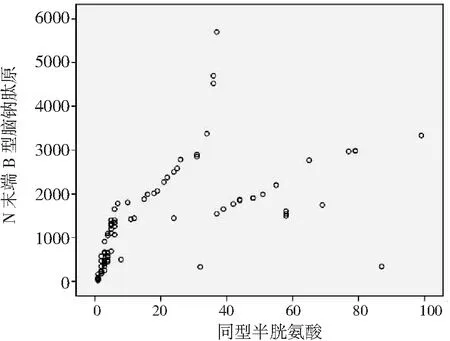
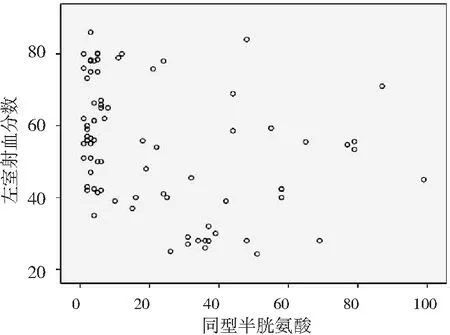

图1老年冠心病慢性心力衰竭患者血浆同型半胱氨酸水平与N末端B型脑钠肽前体、左室射血分数和左室舒张末期内径的相关性
3 讨论
Hcy是一种含硫氨基酸,主要由食物摄取的甲硫氨酸转化而来,其水平升高与血栓形成和动脉粥样硬化性血管疾病的风险增加有关[8]。McCully等率先发现并提出血浆Hcy水平升高是动脉粥样硬化性心血管疾病的潜在危险因素。血浆Hcy水平的升高可促进动脉粥样硬化的发生、发展,可能作用机制为内皮功能紊乱、平滑肌细胞增殖、炎症、氧化应激和胶原代谢改变[9-13],引发心脏重构和功能障碍,最终导致心力衰竭。脑钠肽是目前研究且得到证实最多的心脏生物学标志物,以多种形式存在,其中B型脑钠肽(BNP)是在猪脑中发现的32肽氨基酸,大量存在于心室肌细胞,而NT-proBNP与BNP来源相同且等摩尔分泌,均释放入血,但体内的清除途径不同。BNP通过肾脏、钠尿肽清除受体(NPR-C)和中性肽链内切酶(NEP)清除,而NT-proBNP由肾脏清除。两者的半衰期不同,NT-proBNP半衰期为120 min,明显长于BNP半衰期(22 min),故NT-proBNP体外相对稳定,适用于临床检验。
正常人血浆Hcy水平为5~15 μmol/L,按照其水平不同,高Hcy血症分为轻度(15~30 μmol/L)、中度(30~100 μmol/L)和重度(>100 μmol/L),轻度高Hcy血症常见,重度高Hcy血症少见,而后者多见于Hcy代谢酶的遗传缺陷。本研究对照组血浆Hcy水平正常,冠心病心功能代偿组血浆Hcy水平轻度升高,CHF组则中度升高,且NYHA Ⅱ级组血浆Hcy水平明显低于NYHA Ⅲ~Ⅳ级组,且其与NT-proBNP、LVEDD呈正相关,与LVEF呈负相关,表明血浆Hcy水平与CHF严重程度密切相关,可作为反映CHF病情严重程度的监测指标。
近年相关研究显示,CHF患者高Hcy血症不仅与CHF的发生、发展及严重程度有关,还与预后相关。Fournier等[14]研究显示CHF患者平均血浆Hcy水平较对照组显著升高(P<0.01),且与BNP呈正相关。有文献报道,血浆Hcy水平>15μmol/L的CHF患者5年生存率明显低于血浆Hcy水平<15 μmol/L的CHF患者(P<0.05),且高Hcy血症是CHF患者5年死亡的最强独立预测因素。May等[15]研究显示,伴高Hcy血症的CHF患者3年死亡率较血浆Hcy水平正常的CHF患者升高(P<0.05)。Ma等[16]探讨了高Hcy血症与急性心肌梗死短期预后的相关性,发现高Hcy组心力衰竭、心脏破裂、死亡的发生率和总心血管事件较正常Hcy组明显增加,但两组术后心绞痛和心肌梗死的发生率无明显变化,且急性心肌梗死30 d的不良事件发生率与年龄、Hcy水平密切相关,其中高Hcy是心肌梗死患者30 d心血管事件发生的独立预测因子。
综上,血浆Hcy水平与心脏功能的相关性较好,在一定程度上反映老年冠心病CHF患者心功能损害的严重程度,临床可结合NT-proBNP等传统的心力衰竭生物标记物及危险因素对患者进行评价,并以此开展治疗、评估预后,改善老年CHF患者的生活质量。
[1] Ziaeian B, Fonarow G C. Epidemiology and aetiology of heart failure[J].Nat Rev Cardiol, 2016,13(6):368-378.
[2] Danelich I M, Reed B N, Sueta C A. Stage A: can heart failure be prevented[J].Curr Cardiol Rev, 2015,11(1):4-9.
[3] Dunlay S M, Roger V L. Understanding the epidemic of heart failure: past, present, and future[J].Curr Heart Fail Rep, 2014,11(4):404-415.
[4] Washio T, Nomoto K, Watanabe I,etal. Relationship between plasma homocysteine levels and congestive heart failure in patients with acute myocardial infarction. Homocysteine and congestive heart failure[J].Int Heart J, 2011,52(2):224-228.
[5] 王芊,华川,郭旭,等.同型半胱氨酸等危险因子与冠心病的相关性分析[J].临床误诊误治,2012,25(3):42-44.
[6] Hunt S A, Abraham W T, Chin M H,etal. 2009 focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines Developed in Collaboration with the International Society for Heart and Lung Transplantation[J].J Am Coll Cardiol, 2009,53(15):1-90.
[7] NT-proBNP临床应用中国专家共识小组.NT-proBNP临床应用中国专家共识[J].中国心血管病研究,2011,9(6):401-408.
[8] 夏豫,周瑾,李春林,等.超敏C反应蛋白与血清同型半胱氨酸联合检测诊断冠心病的价值[J].临床误诊误治,2010,23(12):1140-1141.
[9] Joseph, J, Washington, A, Joseph L,etal. Hyperhomocysteinemia leads to adverse cardiac remodeling in hypertensive rats[J].Am J Physiol Heart Circ Physiol, 2002,283(6):2567-2574.
[10] Joseph, J, Joseph L, Shekhawat N S,etal. Hyperhomocysteinemia leads to pathological ventricular hypertrophy in normotensive rats[J].Am J Physiol Heart Circ Physiol, 2003,285(2):679-686.
[11] Devi S, Kennedy R H, Joseph L,etal. Effects of long-term hyperhomocysteinemia on myocardial structure and function in hypertensive rats[J].Cardiovasc Pathol, 2006,15(2):75-82.
[12] Miller A, Mujumdar V, Palmer L,etal. Reversal of endothelial dysfunction by folic acid in homocysteinemic hypertensive rats[J].Am J Hyperten, 2002,15(2 Pt 1):157-163.
[13] Walker E, Black J, Parris C,etal. Effect of experimental hyperhomocysteinemia on cardiac structure and function in the rat[J].Ann Clin Lab Sci, 2004,34(2):175-180.
[14] Fournier P, Fourcade J, Roncalli J,etal. Homocysteine in Chronic Heart Failure[J].Clin Lab, 2015,61(9):1137-1145.
[15] May H T, Alharethi R, Anderson J L,etal. Homocysteine levels are associated with increased risk of congestive heart failure in patients with and without coronary artery disease[J].Cardiology, 2007,107(3):178-184.
[16] Ma Y, Li L, Geng X B,etal. Correlation between hyperhomocysteinemia and outcomes of patients with acute myocardial infarction[J].Am J Ther, 2014,23(6):1464-1468.
CorrelationofSerumHomocysteineandCardiacFunctioninChronicHeartFailureElderlyPatientswithCoronaryAtheroscleroticHeartDisease
ZHU Hong, MA Li-na, LIU Chuan, YANG Wei, LI Yun, QIAN Yu-ying
(Department of Combination Medicine, Xuanwu Hospital, Capital University of Medical Sciences, Beijing 100053, China)
ObjectiveTo observe correlation between serum homocysteine (Hcy) levels and cardiac function in chronic heart failure (CHF) elderly patients with coronary atherosclerotic heart disease (CAD).MethodsA total of 62 elderly patients with CAD were selected as CAD group, and the patients were divided into CHF subgroup (n=42) and cardiac function compensatory subgroup (n=20) according to cardiac function classification criteria from New York Heart Association (NYHA), and then CHF subgroup were divided into NYHA grade Ⅱ subgroup and NYHA grade Ⅲ-Ⅳ subgroup; other 20 healthy elderly patients taking medical examination at the same period were selected as control group. Changes of serum Hcy, n-terminal pro-b-type natriuretic peptide (NT-proBNP), left ventricular ejection fraction (LVEF) and left ventricular end diastolic dimension (LVEDD) were compared, and correlations between serum Hcy levels with NT-proBNP, LVEF and LVEDD were analyzed in all groups and subgroups.ResultsCompared with those in control group, serum Hcy and NT-proBNP levels in compensatory and CHF subgroups and LVEDD level in CHF subgroup were significantly increased, while LVEF level in CHF subgroup was decreased (P<0.05). Compared with those in compensatory subgroup, serum Hcy, NT-proBNP and LVEDD levels were significantly increased, while LVEF level was significantly decreased in CHF subgroup (P<0.05). There were significant differences in serum Hcy and NT-proBNP levels between NYHA grade II and NYHA grade Ⅲ -Ⅳ subgroups (P<0.05). Serum Hcy level in CHF elderly patients with CAD were positively correlated with NT-proBNP and LVEDD levels, and negatively correlated with LVEF level.ConclusionSerum Hcy level in CHF elderly patients with CAD significantly increases, and it is significantly correlated with NT-proBNP, LVEF and LVEDD levels, which can be used as an index in reflection of severity of heart failure.
Coronary disease; Heart failure; Homocysteine
教育部人文社会科学研究青年项目基金(12YJCZH146)
100053 北京,首都医科大学宣武医院综合科
钱玉英,电话:010-83198707;E-mail:qyy_abc@sohu.com
R541.4;R541.6
A
1002-3429(2017)12-0070-04
10.3969/j.issn.1002-3429.2017.12.028
2017-07-06 修回时间:2017-08-21)
