Overnight pulse oximetry for screening of obstructive sleep apnea in at-risk adult patients in the primary care setting: prospective case series
2017-12-21LapKinChiangCheukWaiKamLornaNg
Lap-Kin Chiang, Cheuk-Wai Kam, Lorna V. Ng
1. Family Medicine and General Outpatient Department, Kwong Wah Hospital, Hong Kong
Overnight pulse oximetry for screening of obstructive sleep apnea in at-risk adult patients in the primary care setting: prospective case series
Lap-Kin Chiang1, Cheuk-Wai Kam1, Lorna V. Ng1
1. Family Medicine and General Outpatient Department, Kwong Wah Hospital, Hong Kong
Objective:To estimate prevalence of OSA among at risk adult patients in primary care setting.To test the correlation and agreement between overnight pulse oximetry and polysomnography(PSG). To test the OSA screening performance of overnight pulse oximetry.Design and Setting:Prospective case series involving adult Chinese patients with risk factors for OSA at a primary care clinic of Hong Kong.Methods:The prevalence and severity of OSA were established based on overnight pulse oximetry derived oxygen desaturation index (ODI). Screening performance of overnight pulse oximetry was compared directly with gold standard diagnostic test PSG.Results:Three hundred and five male and 229 female patients were recruited. Snoring(48.3%) was the top presenting symptom. Three hundred and twenty five patients (60.9%) were screened positive to have OSA. One hundred and nine patients had performed PSG, the ODI_4 and apnoea-hypopnea index (AHI) had Pearson correlation coefficient 0.71 (P<0.001). Bland and Altman plot showed good agreement. Using designation criteria of ODI_4≥5 events/hr, the sensitivity and specificity for OSA diagnosis are 94.4% and 78.9% respectively.Conclusion:The prevalence of OSA is 60.9% among adult primary care population who are at risk for OSA. Overnight pulse oximetry shows good performance as a screening tool for the screening of OSA.
Obstructive sleep apnea; overnight pulse oximetry; primary care
Introduction
Obstructive sleep apnea (OSA) is a common sleep condition characterized by complete or partial airway obstruction caused by pharyngeal collapse during sleep, resulting in health impairment and other related injuries. The prevalence of OSA was estimated to be as high as 20%—30% in the middle-aged population [1, 2].According to an epidemiological study in Hong Kong, the prevalence of OSA (apnea—hypopnea index (AHI) ≥5) was 8.8% in men and 3.7%in women, and the prevalence of OSA syndrome (AHI ≥5 and daytime sleepiness)was 4.1% in men and 2.1% in women [3, 4].Cardiovascular [5—10], metabolic [11—13],and neuropsychological morbidities [14—16]and increased risk of motor vehicle accidents[17—19] have been demonstrated in individuals with untreated OSA. Overnight full-channel polysomnography (PSG) performed in a sleep laboratory remains the gold standard diagnostic test.However, PSG is time-consuming and costly and requires expertise for interpretation [20]. Young et al. [21] reported that in 82% of men and 93% of women with moderate to severe sleep apnea, sleep apnea had not been diagnosed.
There is some evidence that the prevalence of OSA among patients in the primary care setting is higher than in epidemiological studies conducted in the community because of the higher prevalence of risk factors or comorbidities associated with OSA [22]. The pretest probability for OSA is approximately 30% [23, 24]. Because of limitations of clinical assessment and the lack of a diagnostic test, the usual practice for primary health care physicians is referral of all such patients to a respiratory physician or sleep center for a confirmation test.According to Flemons et al. [25], the waiting time for the sleep service in five countries ranged from 2 to 60 months.
Oximetry alone is often used as the first screening tool for OSA because of the universal availability of cheap recording pulse oximeters [26]. According to a review by Nikolaus et al.[27], there is a broad range of sensitivity and specificity for pulse oximetry as a screening tool for sleep-disordered breathing, with sensitivity ranging from 31% to 98% and specificity ranging from 41% to 100%.
Chiang et al. [28] conducted a study in a regional primary care clinic in Hong Kong and concluded that overnight pulse oximetry has good correlation with PSG. This study recruited consecutive subjects to estimate the prevalence of OSA among at-risk adult patients in the primary care setting to test the correlation and agreement between overnight pulse oximetry and PSG and to test the screening performance of portable overnight pulse oximetry.
Methods
Study population
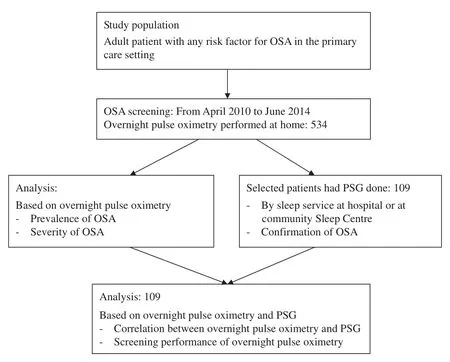
Fig. 1. Study fl ow chart.
Consecutive patients aged 18 years or older attending a primary care clinic affiliated with a regional hospital in Hong Kong with one or more of the following criteria were selected for OSA screening: body mass index greater than 25 kg/m2;neck circumference greater than 16 inches for women and greater than 17 inches for men; young hypertension;1Young hypertension refers to diagnosed hypertension and to antihypertensive treatment before the age of 40 years.poorly controlled hypertension;2Poorly controlled hypertension refers to blood pressure persistently higher than 140/90 mm Hg despite optimal treatment with three or more antihypertensive agents.poorly controlled type 2 diabetes mellitus;3Poorly controlled type 2 diabetes mellitus refers to two consecutive glycated hemoglobin measurements greater than 8% despite optimal treatment with oral hypoglycemic agents.congestive heart failure; cardiac arrhythmia; erectile dysfunction of undetermined cause; subjective daytime sleepiness; excessive snoring during sleep; ambulatory blood pressure monitoring — confirmed nocturnal nondipper; and cerebrovascular disorders. Exclusion criteria included the following: hemoglobin level below 10 g/dL; poor tissue perfusion (such as Raynaud disease, nail vanish, fungal infection of nails); chronic obstructive pulmonary disease; and difficulty in cooperation (such as dementia).
Study design
After operation of the portable pulse oximeter had been mastered, the machine was loaned to recruited patients to perform overnight pulse oximetry by themselves at home (Fig. 1). The computer-generated overnight pulse oximetry data were manually verified by the investigator for validity. If the report suggested the patient had moderate or severe OSA, the patient was referred to the sleep service for further confirmation. Besides,patients could consider having an overnight sleep study (PSG)performed at the community sleep study center. The polysomnograms of selected patients if done were collected for analysis.
Measurement
Portable pulse oximeter:A Konica Minolta Pulsox-300i portable pulse oximeter was used for this study. Pulse rate and arterial oxygen saturation (SaO2) were continuously measured overnight, and the data were stored in the oximeter. Recorded data were then transferred to a computer for processing and analysis. The SaO2analysis, pulse rate analysis, oxygen desaturation index (ODI; number of oxygen desaturation events per hour of measurement time), and pulse disorder index (pulse rise events per hour of measurement time) will be generated in oximetry report.
Polysomnography:Some patients had at-home PSG done by the community sleep center. All PSG data were recorded by a computerized polysomnographic system (Alice 5, Philips).These included standardized montage: two-channel electroencephalograms, electro-oculograms, submental and leg electromyograms, electrocardiograms, airflow measurement by a thermistor, thoracoabdominal movements measured by inductive plethysmography, and SaO2measured with a pulse oximeter.
Event definition:For both PSG and overnight pulse oximetry, apneas, hypopneas, AHI, oxygen desaturation, and ODI were defined according to standard criteria. The PSG AHI was considered as the diagnostic definition for OSA, where OSA severity is categorized as mild (AHI=5—14 events per hour),moderate (AHI=15—30 events per hour), and severe (AHI>30 events per hour) [29].
Oxygen desaturation was defined as a decrease of 4% or more from the baseline SaO2[27]. ODI_4 was used as the screening diagnostic criterion in this study. Participants who had sleep-disordered breathing events associated with five or more oxygen desaturation events of the peripheral artery of 4% or more per hour (ODI_4≥5 events per hour) were defined as screening-positive patients. For screening-positive patients,the severity of OSA was also determined by cutoff as mild(ODI_4=5—14 events per hour), moderate (ODI_4=15—30 events per hour), or severe (ODI_4>30 events per hour).
Statistical analysis
Descriptive statistics including mean, standard deviation (SD),frequency, and percentage were used to summarize the characteristics of the variables. The diagnosis of OSA was determined by PSG (i.e., the gold standard test). The correlation and agreement of overnight pulse oximetry and PSG in the diagnosis of OSA were assessed by Pearson’s product-moment correlation coefficient (rvalue) and Bland—Altman plots [30] respectively.The sensitivity and specificity of overnight pulse oximetry at various cutoff points in screening of OSA were tabulated and plotted as a receiver operating characteristic (ROC) curve. The analysis was conducted with MedCalc (version 14.10.2).
Ethics approval
The study was approved by Hong Kong Hospital Authority Kowloon West Cluster Research Ethics Committee.
Results
From April 1, 2010, to June 30, 2014, 305 male patients (57.1%)and 229 female patients (42.9%) were involved in the OSA screening study. Table 1 summarizes the patients’ characteristics, anthropomorphic measurements, and overnight pulse oximetry results.
Their mean (SD) age was 54.1 (13.5) years, the mean(SD) body mass index was 27.0 (4.7) kg/m2, the mean (SD)neck circumference was 37.8 (2.9) cm, and the mean (SD)Epworth Sleepiness Scale score was 9.8 (5.5). Two of the leading presenting symptoms were snoring (48.3%) and excessive daytime sleepiness (15.2%), while the commonest comorbidities were hypertension (44.9%), obesity (44.9%), and hyperlipidemia(20.2%). The mean clinic blood pressure was 130.1/77.6 mm Hg.
Prevalence of OSA
On the basis of the screening designation of overnight pulse oximetry (ODI_4≥5 events per hour), 60.9% patients(325/534) were screened as having OSA. The proportions of mild, moderate, and severe OSA based on ODI_4 determination were 57.6% (187/325), 28.9% (94/325), and 13.5%(44/326) respectively.
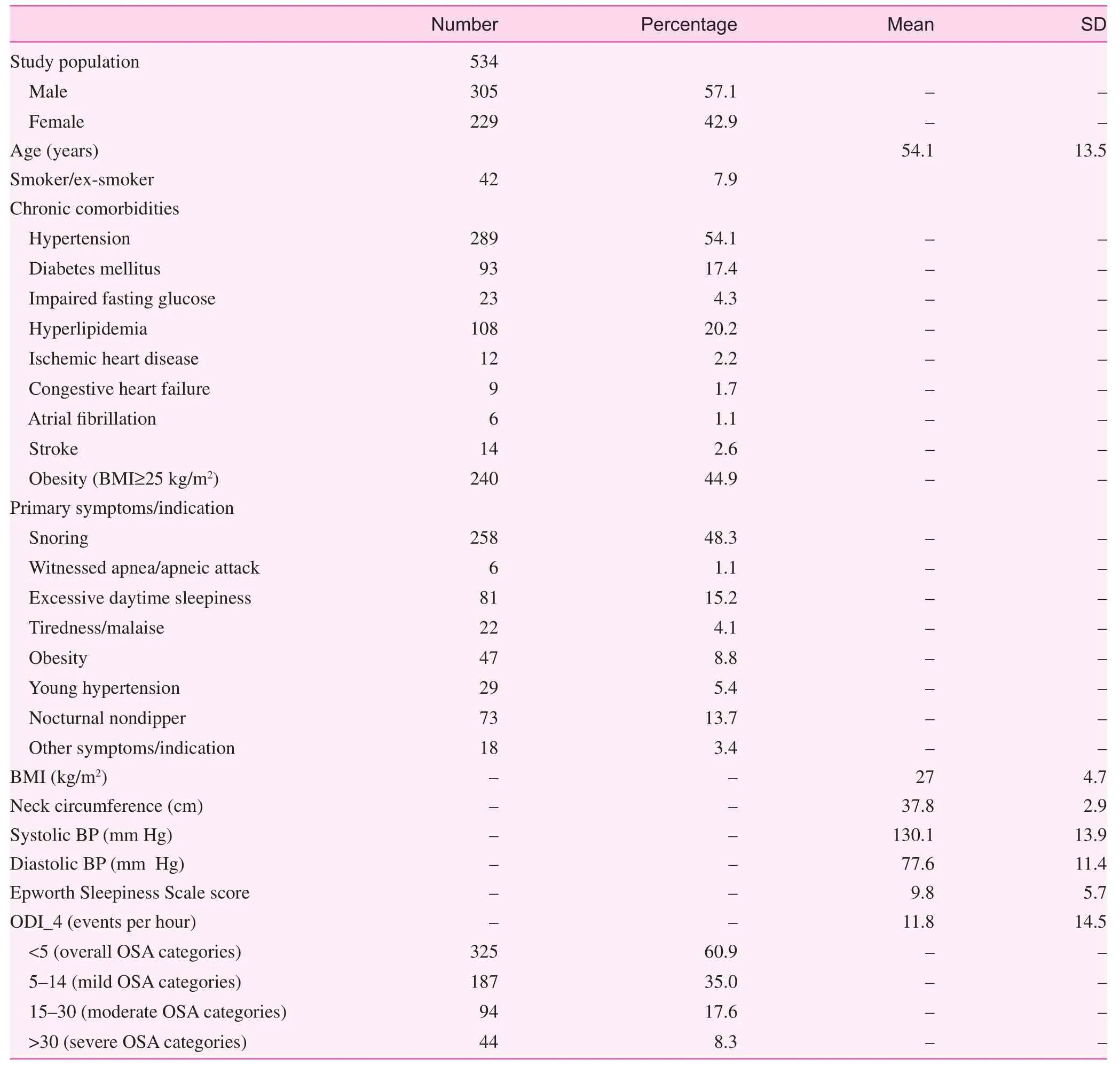
Table 1. Summary of patient characteristics
Overnight pulse oximetry and PSG
In 109 patients PSG was performed either at the hospital sleep center or at home by the community sleep service center.The PSG-derived AHI was a mean 29.2 events per hour and the SD was 24.6 events per hour, while overnight pulse oximetry—derived ODI_4 was a mean 18.6 events per hour and the SD was 17.7 events per hour.
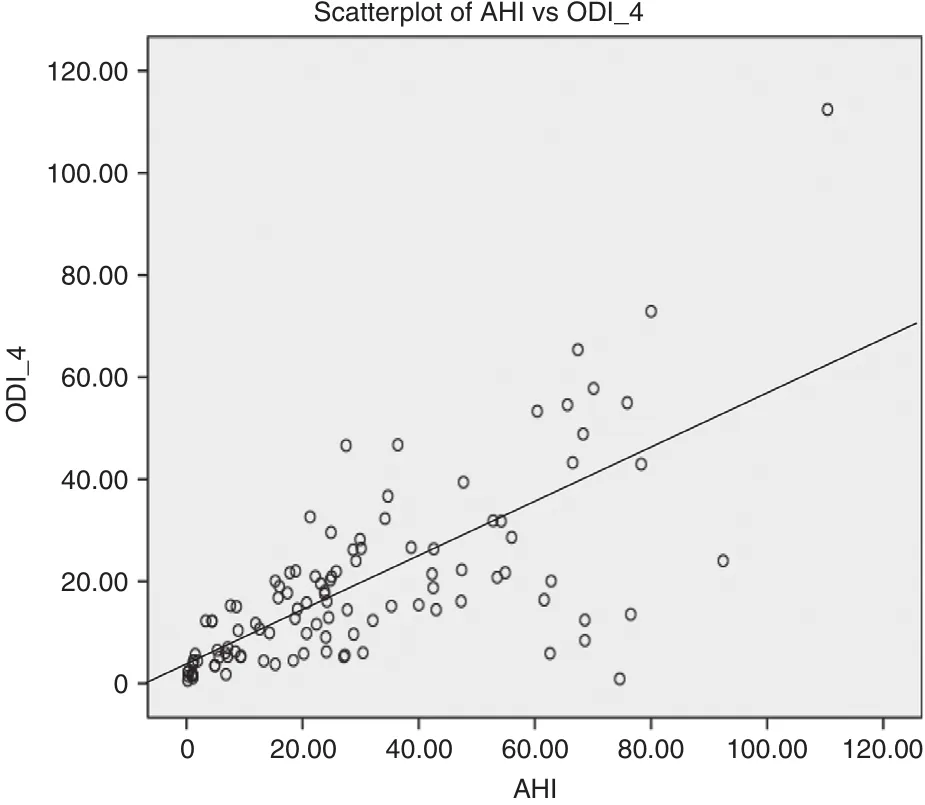
Fig. 2. The scatterplot of ODI_4 against apnea—hypopnea index (AHI).
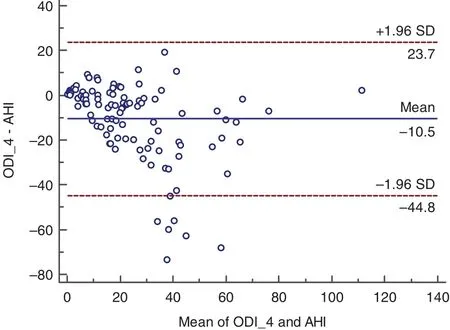
Fig. 3. Bland—Altman plot illustrating the agreement between ODI_4 and apnea—hypopnea index (AHI).
The scatter plot (Fig. 2) demonstrates a linear relationship between ODI_4 and AHI. ODI_4 and AHI haver=0.71 (95%confidence interval 0.59—0.79,P<0.001). The mean difference between ODI_4 and AHI is -10.5 events per hour, while the SD of the difference is 8.9 events per hour. The Bland—Altman plot is illustrated in Fig. 3. The mean difference between AHI and ODI_4 and its ±1.96 SD gives the limits of agreement between the two measurement tools. Most of the dots lie between the boundary of ±1.96 SD of the mean difference lines except for a few outliers, which indicates good agreement between ODI_4 and AHI.
Screening performance of overnight pulse oximetry
The screening performance of overnight pulse oximetry at various values of ODI_4 is tabulated in Table 2. An ROC curve of ODI_4 in the diagnosis of OSA is shown in Fig. 4. On the basis of the ROC curve of ODI_4, the best cutoff criterion is 4.42 events per hour, with sensitivity of 76.7% and specificity of 78.9%. With use of the case designation criterion of five or more events per hour for ODI_4, the sensitivity and specificity for OSA diagnosis are 94.4% and 78.9% respectively.
Discussion
This prospective case series study revealed that OSA is common among at-risk adult patients in the primary care setting,and that overnight pulse oximetry shows good performance as a screening tool for OSA.
A vast number of patients have risk factors or are suspected of having OSA in primary care. Oximetry alone is often used as the first screening tool for OSA because of the universal availability of cheap recording pulse oximeters [26]. In Japan, overnight pulse oximetry has been used for OSA screening for workers in transport, construction,retail, and security companies [31]. Nikolaus et al. [27] concluded that there is wide range of sensitivity and specificityfor overnight pulse oximetry and there is no uniform definition for a normal or abnormal ODI [27]. In the studies by Stradling and Crosby [32] and Kripke et al. [33] the threshold for an abnormal ODI was five or more desaturation events per hour. With use of the same cutoff designation of ODI_4 in our study, 60.9% of the selected population in primary care was screened positive for OSA, while 42.4% had at least moderate severity.

Table 2. Screening performance of overnight pulse oximetry for various designation
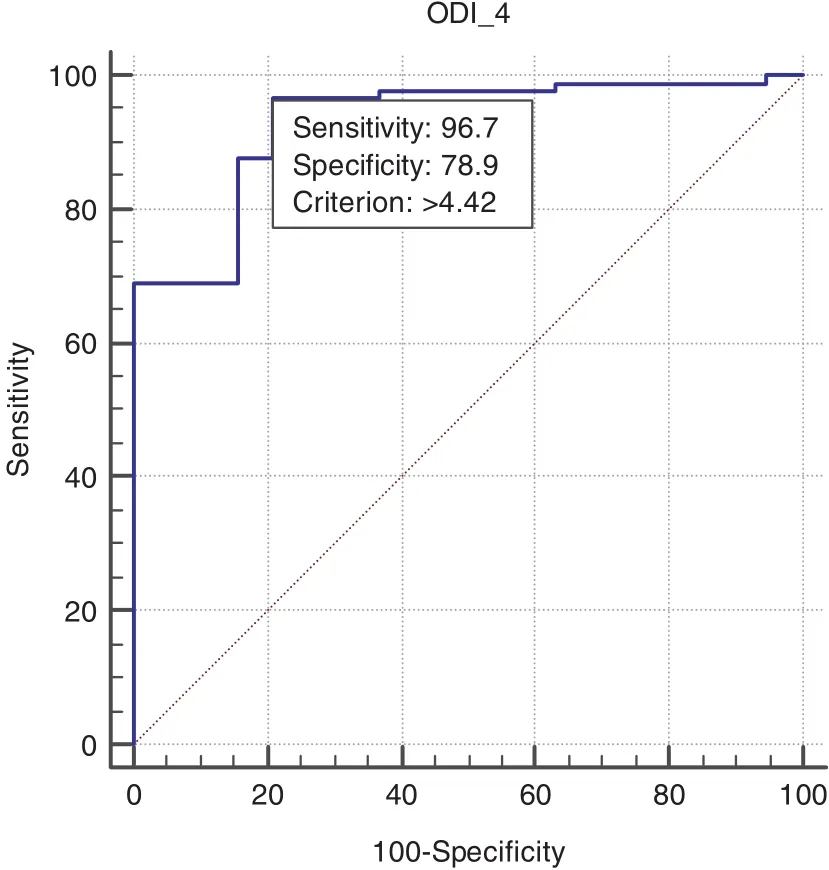
Fig. 4. Receiver operating characteristic curve of ODI_4 designation in the diagnosis of obstructive sleep apnea.
For a screening test, sensitivity measures how good the test is at correctly identifying ‘diseased’ individuals and specificity measures how good the test is at correctly identifying‘nondiseased’ individuals. To be an effective screening tool for OSA, overnight pulse oximetry must be able to screen out patients with all levels of disease severity and to rule out patients without disease in a manner that is less expensive than current diagnostic procedures. We investigated the performance of overnight pulse oximetry as a screening tool for OSA by comparing its screening performance directly with that of PSG.
In our study, ODI_4 and AHI had good correlation.Nevertheless, ODI_4 was globally less useful than AHI, the reasons for which are unclear. Decreased sleep efficiency may decrease the ODI since it is derived from the total probe-on time and not the total sleep time [34]. Furthermore, technical limitations may impair the detection of hypopneic changes.The typical cyclical drop in SaO2in patients with OSA lags 45—60 s behind a respiratory event and should be accurately detected at this measurement speed [35]. With use of this designation in our study, the sensitivity and specificity are 94.4%and 78.9% respectively, while the positive predictive value and negative predictive value are 95.5% and 75.0% respectively.The results support the proposition of overnight pulse oximetry as the screening tool for OSA for selected populations in the primary care setting.
Implications
On the basis of current available evidence or recommendations from American Academy of Sleep Medicine, it is suggested that continuous positive airway pressure might be initiated in selected patients if they have OSA-associated symptoms and overnight pulse oximetry—confirmed OSA of at least moderate severity [29]. It can avoid unnecessary referrals and the current long waiting time needed to see a respiratory specialist in the public health sector. It can also expedite early management of OSA, resulting in prevention of OSA-related complications.For those patients with severe OSA (i.e., indication for continuous positive airway pressure), urgent referral to a respiratory specialist is justified.
Limitation
This is a case series study, and not all patients with risk factors for OSA were recruited for OSA screening, and there may have limitations in the generalizability of the results. A welldesigned cross-sectional study may be constructed to investigate the actual prevalence of OSA in the primary care setting.Most PSG investigations are done by a community sleep center, and computer-generated PSG reports may be limited in their validity.
Conclusion
It is estimated that there is high prevalence of OSA among atrisk adult patients in primary care. Overnight pulse oximetry shows good correlation and agreement with PSG and has good screening performance as a screening tool for the screening of OSA in the primary care setting.
Conflicts of interest
The authors declare no conflict of interest.
Funding
Tung Wah Group of Hospitals Research Fund provided funding.
Significance statement
Pulse oximetry is often used as the first screening tool for obstructive sleep apnea (OSA) but with variable range of sensitivity and specificity. This study recruits consecutive and representative patients from the primary care setting indicated for OSA screening with overnight pulse oximetry. There is high prevalence of screening positive OSA among at-risk patients in primary care. As compared directly with gold standard diagnostic test polysomnography (PSG), overnight pulse oximetry shows good screening performance and is a good screening tool for OSA in the primary care.
1. Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S, et al.The occurrence of sleep-disordered breathing among middleaged adults. New Engl J Med 1993;328(17):1230—5.
2. Young T, Evans L, Finn L, Palta M. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep 1997;20:705—6.
3. Ip MS, Lam B, Lauder IJ, Tsang KW, Chung KF, Mok YW, et al.A community study of sleep-disordered breathing in middle-aged Chinese men in Hong Kong. Chest 2001;119(1):62—9.
4. Ip MS, Lam B, Tang LC, Lauder IJ, Ip TY, Lam WK. A community study of sleep-disordered breathing in middle-aged Chinese women in Hong Kong. Chest 2004;125:127—34.
5. Young T, Peppard P, Palta M, Hla KM, Finn L, Morgan B, et al.Population-based study of sleep-disordered breathing as a risk factor for hypertension. Arch Intern Med 1997;157(15):1746—52.
6. Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Eng J Med 2000;342(19):1378—84.
7. O’Connor GT, Caffo B, Newman AB, Quan SF, Rapoport DM,Redline S, et al. Prospective study of sleep-disordered breathing and hypertension: the Sleep Heart Health Study. Am J Respir Crit Care Med 2009;179(12):1159—64.
8. Mehra R, Benjamin EJ, Shahar E, Gottlieb DJ, Nawabit R,Kirchner HL, et al. Association of nocturnal arrhythmias with sleep-disordered breathing: the Sleep Heart Health Study. Am J Respir Crit Med 2006:173(8):910—6.
9. Sorajja D, Gami AS, Somers VK, Behrenbeck TR, Garcia-Touchard A, Lopez-Jimerz F. Independent association between obstructive sleep apnea and subclinical coronary artery disease.Chest 2008;133:927—33.
10. Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM,Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. New Engl J Med 2005;353(19):2034—41.
11. Resnick HE, Redline S, Shahar E, Gilpin A, Newman A, Walter R, et al. Diabetes and sleep disturbance: findings from the sleep heart health study. Diabetes Care 2003;26(3):702—9.
12. Punjabi NM, Sorkin JD, Katzel LI, Goldbery AP, Schwartz AR,Smith PL. Sleep-disordered breathing and insulin resistance in middle-aged and overweight men. Am J Respir Crit Care Med 2002;165(5):677—82.
13. Steiropoulos P, Tsara V, Nena E, Fitili C, Kataropoulou M,Froudarakis M, et al. Effect of continuous positive airway pressure treatment on serum cardiovascular risk factors in patients with obstructive sleep apnea-hypopnea syndrome. Chest 2007;132(3):843—51.
14. Engleman HM, Martin SE, Deary IJ, Douglas NJ. Effect of continuous positive airway pressure treatment on daytime function in sleep apnea/hypopnoea syndrome. Lancet 1994;343:572—5.
15. Aloia MS, Arnedt JT, Davis JD, Riggs RL, Byrd D. Neuropsychological sequelae of obstructive sleep apnea-hypopnea syndrome:a critical review. J Int Neuropsychol Soc 2004;10:772—85.
16. Beebe DW, GroeszL, Wells C, Nichols A, McGee K. The neuropsychological effects of obstructive sleep apnea: a metaanalysis of norm-referenced and case-controlled data. Sleep 2003;26:298—307.
17. Young T, Blustein J, Finn L, Palta M. Sleep-disordered breathing and motor vehicle accidents in a population based sample of employed adults. Sleep 1997;20:608—13.
18. Barbé F, Pericás J, Muñoz A, Findley L, Antó JM, Agustí AG,et al. Automobile accidents in patients with sleep apnea syndrome. An epidemiological and mechanistic study. Am J Respir Crit Care Med 1998;158(1):18—22.
19. Horstmann S, Hess CW, Bassetti C, Gugger M, Mathis J.Sleepiness-related accident in sleep apnea patients. Sleep 2000;23(3):383—92.
20. Ross SD, Allen IE, Harrison KJ, Kvasz M, Connelly J,Sheinhait IA. Systematic review of the literature regarding the diagnosis of sleep apnea. Evidence Reports/Technology Assessments, No. 1. AHCPR Publication no. 99-E002. Rockville, MD: Agency for Health Care Policy and Research; 1999.
21. Young T, Evans L, Finn L, Palta M. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep 1997;20:705—6.
22. Dement WC, Netzer NC. Primary care: is it the setting to address sleep disorders? Sleep Breath 2000;4:1—6.
23. Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med 1999;131:485—91.
24. Netzer NC, Hoegel JJ, Loube D, Netzer CM, Hay B, Alvarez-Sala R, et al. Prevalence of symptoms and risk of sleep apnea in primary care. Chest 2003;124:1406—14.
25. Flemons WW, Douglas NJ, Kuna ST, Rodenstein DO, Whealtley J. Access to diagnosis and treatment of patients with suspected sleep apnea. Am J Respir Crit Care Med 2004;169;668—72.
26. Management of obstructive sleep apnea/hypopnea syndrome in adults. A national clinical guideline. Scottish Intercollegiate Guidelines Network. ISBN 1 899893 33 4. First published 2003.
27. Nikolaus N, Eliasson AH, Cordula N, Kristo DA. Overnight pulse oximetry for sleep-disordered breathing in adults: a review.Chest 2001;120(2):625—33.
28. Chiang LK, Ng PT, Kam CW, Ng VL, Wong CY, Yee KS, et al.Usefulness in using portable overnight pulse oximeter for screening obstructive sleep apnea in adult patients in primary health care setting. Hong Kong Pract 2011;33:146—52.
29. Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med 2009;5(3):263—76.
30. Bland JM, AltmanDG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;1(8476): 307—10.
31. Kuniyuki N, Kazuhiko E, Hiroko H, Shunsuke S, Tetsuya M,Yasuo M. The usefulness of sleep apnea syndrome screening using a portable pulse oximeter in the workplace. J Occup Health 2007;49:1—8.
32. Stradling JR, Crosby JH. Predictors and prevalence of obstructive sleep apnea and snoring in 1001 middle aged men. Thorax 1991;46:85—90.
33. Kripke DF, Acoli-Israel S, Klauber MR, Wingard DL, Mason WJ,Mullaney DJ. Prevalence of sleep-disordered breathing in ages 40—64 years: a population-based survey. Sleep 1997;20:65—76.
34. Vazquz JC, Tsai WH, Flemon WW, Masuda A, Brant R, Hajduk E, et al. Automated analysis of digital oximetry in the diagnosis of obstructive sleep apnea. Thorax 2000;55(4):302—7.
35. Warley AR, Mitchell JH, Stradling JR. Evaluation of the Ohmeda 3700 pulse oximeter. Thorax 1987;42(11):892—6.
Lap-Kin Chiang
Family Medicine and General Outpatient Department, 1/F, Tsui Tsin Tong Outpatient Building,Kwong Wah Hospital, 25 Waterloo Road, Mongkok, Hong Kong
Tel.: +852-35-172301
Fax: +852-35-172401
E-mail: chialk@ha.org.hk
24 September 2016;
Accepted 21 March 2017
杂志排行
Family Medicine and Community Health的其它文章
- Health is primary
- Assessing the accuracy of patient report of the 5As (ask, assess,advise, assist, and arrange) for smoking cessation counseling
- Mental health problems due to community violence exposure in a small urban setting
- Burden of road traffic accidents in Nepal by calculating disability- adjusted life years
- Effect of an educational intervention and parental vaccine refusal forms on childhood vaccination rates in a clinic with a large Somali population
- Tobacco cessation pharmacotherapy use among racial/ethnic minorities in the United States: Considerations for primary care
