Effect of an educational intervention and parental vaccine refusal forms on childhood vaccination rates in a clinic with a large Somali population
2017-12-21DianeMadlonKayEmilySmith
Diane J. Madlon-Kay, Emily R. Smith
1. University of Minnesota Medical Center Family Medicine Residency Program, 2020 E. 28th Street, Minneapolis, MN 55407,USA
2. North Memorial Family Medicine Residency Program, 1020 W Broadway Ave, Minneapolis,MN 55411, USA
Effect of an educational intervention and parental vaccine refusal forms on childhood vaccination rates in a clinic with a large Somali population
Diane J. Madlon-Kay1, Emily R. Smith2
1. University of Minnesota Medical Center Family Medicine Residency Program, 2020 E. 28thStreet, Minneapolis, MN 55407,USA
2. North Memorial Family Medicine Residency Program, 1020 W Broadway Ave, Minneapolis,MN 55411, USA
Objective:The purpose of this study is to improve vaccination rates at a clinic with a large Somali population, and many vaccine hesitant parents. The study evaluated the effectiveness of some new materials for vaccine hesitant parents.Methods:Educational sessions were given to providers and staff to give “talking points” and to introduce a vaccine refusal form. Chart reviews were done for notes from 50 random well child visits per month of children less than six years old for 7 months before and after the intervention.Results:Before the intervention, 44% of Somali children who needed shots did not get them at their well child visit. Afterwards, 34% of the Somali children did not get their needed shots. Of non-Somali children, 16.8% did not get needed shots before the intervention, and 12.7% did not get needed shots after the intervention (P=0.07). The MMR was the most frequent vaccine omitted.After the intervention, 29 parents signed the vaccine refusal form.Conclusion:The “talking points” and vaccine refusal form were associated with improvements in immunization rates in this challenging patient population that were not statistically signifi-cant. Refusal form use was not well documented, so its true value requires further study.
Vaccination; immunization; MMR; Somali
Introduction
Vaccines have been a great public health success, second only to the introduction of safe drinking water in reducing disease-associated mortality [1]. The success of vaccines depends on enough parents being willing to vaccinate their children to provide adequate immunization coverage. Unfortunately, there has been an increase in parental concerns about vaccine adverse effects, making many hesitant to vaccinate their children [1]. These parents may refuse vaccinations for their children, or want an alternative schedule. The unvaccinated children then put their communities at risk of disease outbreaks. To continue effective vaccination programs and protect public health,more research is needed to guide physicians on effective methods to reduce parental vaccine refusal.
Parental refusal for vaccination is thought to be the cause of several measles outbreaks,including one in Minnesota in 2011 [2].Twenty-one cases of measles were reported in Minnesota, more cases than in the previous 14 years combined. This outbreak was traced back to an unvaccinated Somali child who had recently returned to Minnesota from abroad. Most of the cases in the Minnesota outbreak were in children of Somali descent. In 2012, only 46% of Somali children who were 24 months old had received the first recommended MMR dose, compared with 88% of non-Somali children in Hennepin County, Minnesota [3]. Many Somali parents believe that the MMR vaccine causes autism. This belief has contributed to the low vaccination rates [3, 4].
Several large national organizations are concerned about parental vaccine refusal and the increasing demand for alternative vaccination schedules. In response, tools have been developed to help physicians to work with vaccination-hesitant parents. The Centers for Disease Control and Prevention(CDC), the American Academy of Family Physicians, and the American Academy of Pediatrics (AAP) [5] partnered to develop a variety of materials that make up their “Provider Resources for Vaccine Conversations with Parents” [6]. The Immunization Action Coalition and the American Academy of Pediatrics have developed vaccine refusal forms that can provide a more formal documentation of parental choice and a format for discussion of the risks of withholding vaccinations[7, 8]. It has been recommended that parents who refuse one or more immunizations sign the refusal form, which should then be kept in the medical record. While this idea is similar to other medical documentation processes, such as informed consent and “against medical advice” documentation, and generally seems to make sense, there has been little to no research on the effectiveness of these materials and forms. The purpose of this study was to evaluate whether the use of new physician resources and refusal forms would be associated with an improvement in childhood vaccination rates at a family medicine clinic in Hennepin County with a large Somali population and many vaccination-hesitant parents.
Methods
The study took place at a family medicine residency clinic in Minneapolis, Minnesota, where well-child care is provided by family medicine residents, faculty, and one nurse practitioner. The nursing staff who work with patients hold different degrees, such as medical assistant and registered nurse, and are referred to as patient care staff (PCS). The clinic serves a diverse urban population; approximately two-thirds of the patients have government insurance, and about one-third are from Africa, primarily from Somalia. In 2011, 71% of Somali 24—35-month-olds at the clinic had received MMR immunization compared with 94% of non-Somali children of this age [9]. The clinic uses the Epic electronic health record, and this was queried for vaccine status and demographic information. The study was approved by the University of Minnesota Institutional Review Board.
The investigators developed “talking points” to address common parental concerns about immunizations, on the basis of material developed by the CDC [6] and the Autism Scientific Foundation. The talking points were incorporated into attractive fl yers and displays that were placed in multiple locations throughout the clinic, including all of the examination rooms. A graphic designer developed the theme of “ARM Your Patients: Address. Reeducate. Make note,” which was incorporated into all materials. The investigators presented an educational session to the physicians and PCS to review common knowledge gaps about vaccines and the talking points.The investigators also introduced the “Decision to not vaccinate my child” refusal form developed by the Immunization Action Coalition, and educated physicians and PCS on its use as a counseling tool and sign of the importance placed on immunizations [8]. Vaccine refusal forms were placed in all of the examination rooms.
A new vaccination process for well-child visits was put into place after this educational session. Before the intervention, the PCS determined which vaccines were required and informed the physician. With the intervention, the PCS would determine what vaccines a child needed and inform the parent. If the parent declined one or more vaccines, the PCS was encouraged to ask the parent why. If the reason was one for which a talking point was provided, the PCS was encouraged to give a brief counterargument. If the parent still declined the vaccine, the PCS informed the physician and gave him or her the vaccine refusal form. The physician then discussed the reason for vaccine refusal or delay with the parent. If the parent continued to decline the vaccine, the physician reviewed the refusal form with the parent. The parent then signed the form,which was scanned into the electronic health record.
Medical record reviews of immunization status were done by a trained reviewer. The reviewer examined notes from 350 medical records from random well-child visits of children younger than 6 years before and after the intervention.The following information was obtained: age of child, sex,language spoken by parent, use of interpreter, race/ethnicity,physician name, vaccines given, vaccines not given, reason(s)for vaccine(s) not given, and documentation of signing of the refusal form. Vaccination rates and rates of use of refusal forms were to be presented at monthly all clinic meetings.
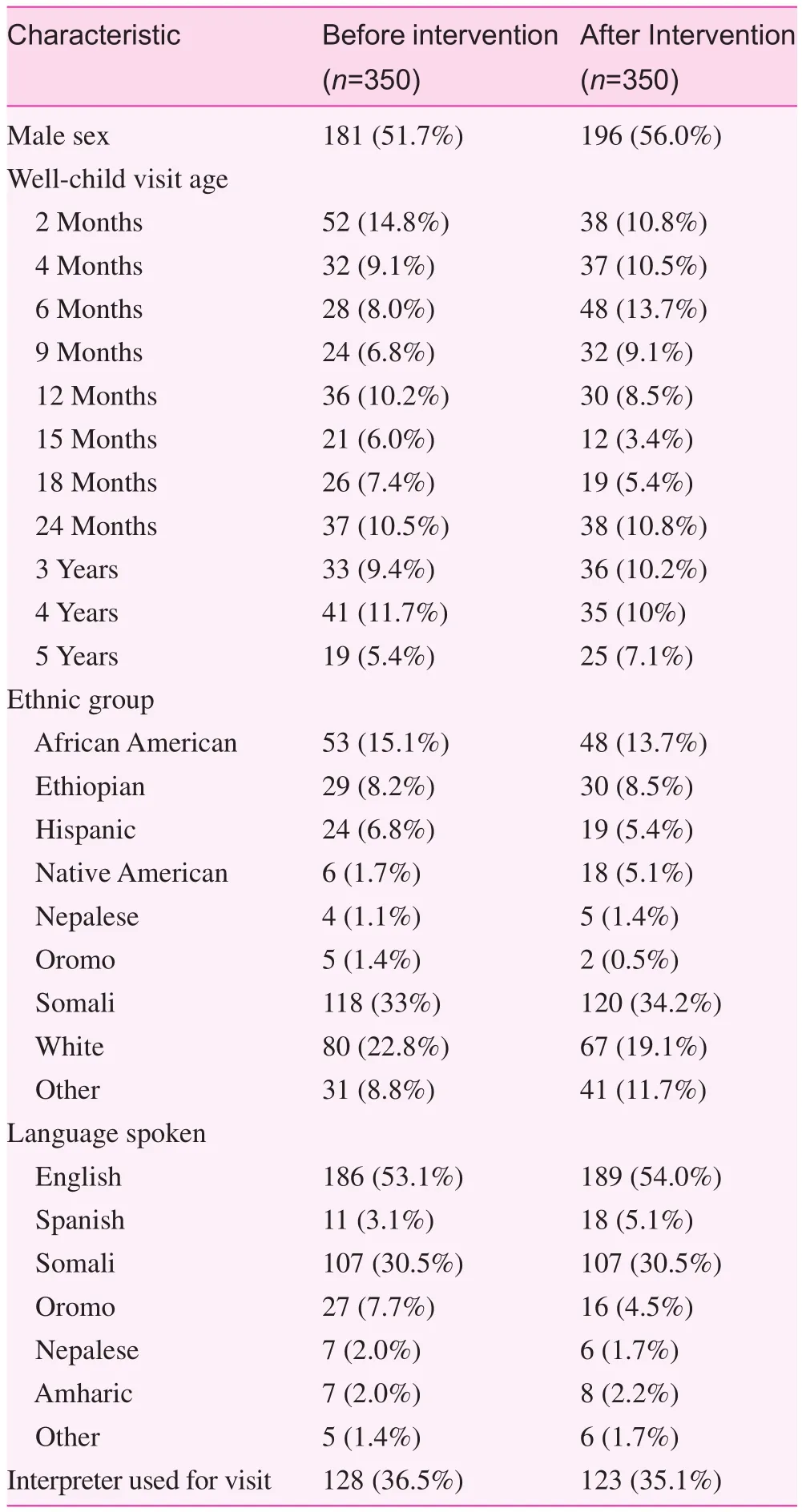
Table 1. Characteristics of children on medical record review
Descriptive statistics were used to summarize the data collected. Fisher’s exact tests were used to compare the rates of omitted vaccines between the two periods and between Somali and non-Somali children. We consideredP<0.05 to be statistically significant. SAS version 9.3 was used for the analyses.
Results
The demographics of the children are shown in Table 1.One-third of the children were Somali, and 21% were white.English was the primary language for 53% of parents.Interpreters were used for 35% of visits. Vaccines were omitted at 23% of the well-child visits overall. Vaccines were omitted at 26.0% of visits before the intervention and at 20.1% of visits after the intervention (P=0.07). As shown in Table 2, fewer vaccines were omitted after the intervention.However, the decrease was not statistically significant.
Significantly more vaccines were omitted in Somali children than in non-Somali children (39% vs. 14.8%P<0.0001).MMR vaccine was the vaccine most frequently omitted. It should have been given and was not given at 106 well-child visits. Somali children also had significantly more MMR vaccines omitted than non-Somali children (52% vs. 11%P<0.0001). All other vaccines were refused by some parents.For example, DTap vaccine was refused at 49 visits and hepatitis A vaccine was refused at 43 visits. The reason for the refusal was documented in some medical records. Concern about autism was a common reason to refuse the MMR vaccine. Other concerns were that the child was ill, too many vaccines were given at one time, or the parent had a preferred schedule for the vaccines. After the intervention, 29 parentssigned the vaccine refusal form, 42% of those who refused a vaccine. Four parents refused to sign the form. In 36 visits, parents refused vaccines but there was no mention in the record about the refusal form.
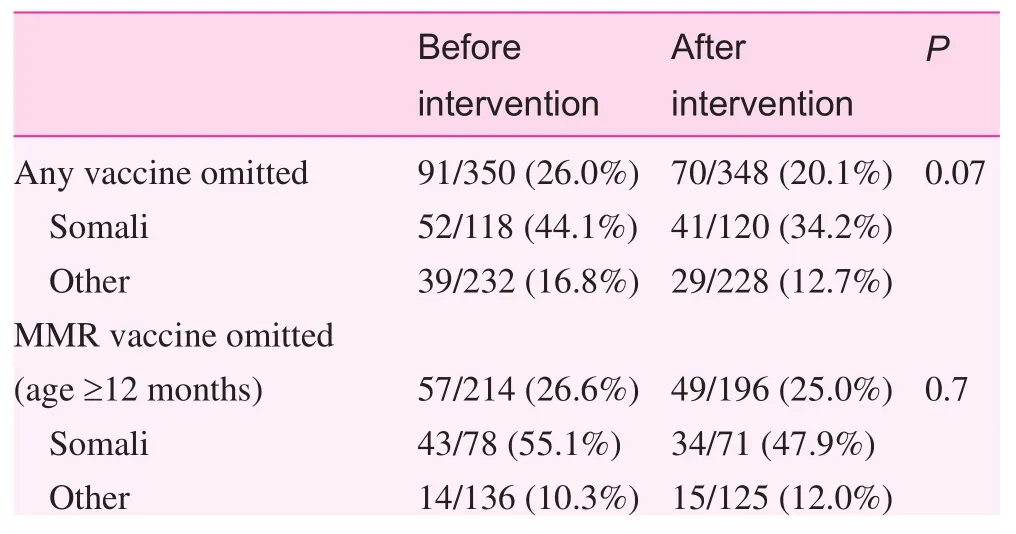
Table 2. Vaccines omitted
Discussion
Many previous efforts to improve childhood vaccination rates have been unsuccessful [10, 11], A systematic review of seven randomized controlled trials evaluating the effects of faceto-face interventions delivered to parents found that they did not improve immunization rates [11]. A systematic review by Sadaf et al. [1] of 30 studies of interventions for reducing parental vaccination hesitancy concluded that there was no convincing evidence of effective interventions to address vaccination hesitancy and refusal, and that further research was needed.
The interventions used in this study were associated with a nonsignificant decrease in omitted immunizations. The physician and PCS talking point materials were all developed from information from the CDC immunization website. The authors are not aware of any other published evaluation of these materials. Use of vaccine refusal forms by both family physicians and pediatricians has been reported previously [12, 13]. A 2012 survey found that 64% of pediatricians and 29% of family physicians often or always require parents to sign a form if they refuse vaccination (P<0.0001) [13]. The AAP has a clear policy recommending use of a refusal form, and has developed its own form. This may explain why more pediatricians than family physicians report using one. However, refusal forms have not previously been evaluated for their effectiveness at improving vaccination rates.
This study was complicated by poor documentation in the electronic health record regarding use of the refusal form for many parents who refused vaccinations. The documentation process was made as simple as possible for physicians by inclusion of the form completion as an item in the wellchild check note template; therefore, when documentation is missing, a form was probably not signed. This may have happened for a variety of reasons, including PCS forgetting to give the form to the physician, the physician forgetting to use it, or the physician not feeling comfortable having the parent sign the form. All of these reasons would decrease the effectiveness of the refusal form. Another limitation of the study is that the planned regular feedback to physicians and PCS did not happen because of delays in reports from the medical record reviewer. In addition, the study has the limitation of occurring in one clinic, without a comparison group.
The study clinic serves a large Somali population, who are particularly hesitant about the MMR vaccine because of fears about autism [3, 4, 9, 14]. Immunization with the MMR vaccine was the immunization most frequently omitted in the study. This concern about the MMR vaccine and autism has been noted in Somali refugees not only in Minnesota but also in Washington State, the United Kingdom, and Sweden [15—17]. The Minnesota Department of Health did a 2-year investigation to better understand vaccination hesitancy among Somali Minnesotans. It then proposed some strategies for increasing vaccination rates in this population [3]. It recommends an approach demonstrated to be effective by Opel et al.[18] where the physician presents a strong recommendation for a vaccine, and continues to strongly recommend the vaccine despite parental hesitancy.
The Department of Health suggested strategies for addressing the low MMR vaccination rate in the Somali population that could be applied to other hesitant parents [3]. Similarly,the AAP Committee on Infectious Disease and the AAP Committee on Practice and Ambulatory Medicine published a clinical report with a variety of suggested strategies to counter vaccination hesitancy [5]. Unfortunately, at this time only the approach of Opel et al. described earlier has been studied, and may have limited generalizability; Opel et al.’s study was done with 16 pediatric physicians dealing with Englishspeaking, white parents with high socioeconomic status from one geographic location [18]. The conclusion of Sadaf et al.[1] from 2013 remains true today: there continues to be a need for good-quality evidence that can guide recommendations on effective strategies to reduce parental vaccine refusal.
Conflicts of interest
The authors have no conflicting or competing interests.
Funding
The study was funded by the UCare Foundation.
Significance statement
Parental refusal for vaccination has contributed to measles outbreaks. Outbreaks in Minnesota have been traced to Somali children, who are less likely to receive the MMR vaccine.Efforts were made to improve vaccination rates in a family medicine clinic in Minnesota with a large Somali population.New strategies used that were not previously studied included educational sessions for providers and staff, displays of “talking points” and use of a vaccine refusal form. Immunization rates improved with these strategies, but not significantly.Somali children received significantly fewer vaccines than non-Somali children. MMR was the most frequent vaccine omitted. There continues to be a need for effective strategies to reduce parental vaccine refusal.
1. Sadaf A, Richards J, Glanz J, Salmon D, Omer S. A systematic review of interventions for reducing parental vaccine refusal and vaccine hesitancy. Vaccine 2013;31:4293—304.
2. Centers for Disease Control and Prevention. Measles outbreak— Hennepin County, Minnesota, February-March 2011. MMWR Morb Mortal Wkly Rep 2011;60:421.
3. Bahta L, Ashkir A. Addressing MMR vaccine resistance in Minnesota’s Somali community. Minn Med 2015;98(10):33—6.
4. Gahr P, De Vries A, Wallace G, Miller C, Kenyon C, Sweet K,et al. An outbreak of measles in an undervaccinated community.Pediatrics 2014;134(1):e220—8.
5. Edwards KE, Hackell JM, The committee on infectious diseases,The committee on practice and ambulatory medicine. Countering vaccine hesitancy. Pediatrics 2016;138(3):e20162146.
6. Centers for Disease Control and Prevention. Provider resources for vaccine conversations with parents [cited 2017 Feb 23].Available from: www.cdc.gov/vaccines/hcp/patient-ed/conversations/index.html.
7. American Academy of Pediatrics. Documenting parental refusal to have their children vaccinated 2013 [cited 2017 Feb 23].Available from: www.aap.org/en-us/Documents/immunization_refusaltovaccinate.pdf.
8. Immunization Action Coalition. Decision to not vaccinate my child 2013 [cited 2017 Feb 23]. Available from: www.pdffiller.com/268875-fillable-decision-not-to-vaccinate-formiac-immunize.
9. Madlon-Kay DJ, Munib S. Autism screening and MMR vaccination in children of Somali refugees. Int J Clin Med Res 2016;3(1):17—9.
10. Fu LY, Zook K, Gingold JA, Gillespie CW, Briccetti C,Cora-Branble D, et al. Strategies for improving vaccine delivery:a cluster-randomized trial. Pediatrics 2016;137(6):e20154603.
11. Kaufman J, Synnot A, Ryan R, Hill S, Horey D, Willis N, et al.Face to face interventions for informing or educating parents about early childhood vaccination. Cochrane Database Syst Rev 2013;(5):CD010038.
12. Kempe A, Daley M, McCauley M, Crane L, Suh C, Kennedy A,et al. Prevalence of parental concerns about childhood vaccines.The experience of primary care physicians. Am J Prev Med 2011;40:548—55.
13. O’Leary ST, Allison MA, Fisher A, Crane L, Beaty B, Hurley L, et al. Characteristics of physicians who dismiss families for refusing vaccines. Pediatrics 2015;136(6):1103—11.
14. Wolff E, Madlon-Kay D. Childhood vaccine beliefs reported by Somali and non-Somali parents in a Minneapolis family medicine clinic. J Am Board Fam Med 2014;27:458—64.
15. Kulane A, Johansson A, Robleh I, Bagenholm G. Somali parents’acceptance of MPR vaccination for their children. An exploratory study. Stockholm: Karolinska Institutet; 2007.
16. Tomlinson N, Redwood S. Health beliefs about preschool immunisations: an exploration of the views of Somali women resident in the UK. Divers Equal Health Care 2013;10:101—13.
17. Wolf E, Rowhani-Rahbar A, Tasslimi A, Matheson J, DeBolt C.Parental country of birth and childhood vaccination uptake in Washington State. Pediatrics 2016;138(1):e20154544.
18. Opel D, Heritage J, Taylor J, Mangione-Smith R, Salas H, DeVere V, et al. The architecture of provider-parent vaccine discussions at health supervision visits. Pediatrics 2013;132:1037—46.
Diane J. Madlon-Kay
University of Minnesota Medical Center Family Medicine Residency Program, 2020 E. 28thStreet, Minneapolis, MN 55407,USA
E-mail: madlo001@tc.umn.edu
24 February 2017;
Accepted 1 April 2017
杂志排行
Family Medicine and Community Health的其它文章
- Health is primary
- Assessing the accuracy of patient report of the 5As (ask, assess,advise, assist, and arrange) for smoking cessation counseling
- Mental health problems due to community violence exposure in a small urban setting
- Burden of road traffic accidents in Nepal by calculating disability- adjusted life years
- Tobacco cessation pharmacotherapy use among racial/ethnic minorities in the United States: Considerations for primary care
- Understanding cultures beyond medicine
