Mental health problems due to community violence exposure in a small urban setting
2017-12-21FarazAhmadJimMedderJenenneGeskeJannetteTaylorRuthMargalit
Faraz Ahmad, Jim Medder, Jenenne Geske, Jannette Taylor, Ruth Margalit
1. Case Western University,School of Medicine, 2109 Adelbert Rd, Cleveland, OH 44106,USA
2. UNMC Dept. of Family Medicine, 983075 Nebraska Medical Center, Omaha, NE 68198-3075,USA
3. UNMC College of Medicine, 985520 Nebraska Medical Center, Omaha, NE 68198-5520,USA
4. Creighton University, School of Law, 2500 California Plaza,Omaha, NE 68178, USA
5. UNMC College of Public Health, 984355 Medical Center,Omaha, NE 68198-4355, USA
Mental health problems due to community violence exposure in a small urban setting
Faraz Ahmad1, Jim Medder2, Jenenne Geske3, Jannette Taylor4, Ruth Margalit5
1. Case Western University,School of Medicine, 2109 Adelbert Rd, Cleveland, OH 44106,USA
2. UNMC Dept. of Family Medicine, 983075 Nebraska Medical Center, Omaha, NE 68198-3075,USA
3. UNMC College of Medicine, 985520 Nebraska Medical Center, Omaha, NE 68198-5520,USA
4. Creighton University, School of Law, 2500 California Plaza,Omaha, NE 68178, USA
5. UNMC College of Public Health, 984355 Medical Center,Omaha, NE 68198-4355, USA
Objective:Studies conducted in large metropolitan inner-city communities with high violent crime rates have demonstrated an association between exposure to violence and mental health problems; therefore the purpose of this study was to determine if similar trends exist in smaller inner-city communities with substantially lower violent crime rates.Methods:One hundred twenty-six children and young adults living in inner-city Omaha,Nebraska, were screened for posttraumatic stress disorder (PTSD), depression, and anxiety symptoms and assessed for community violence exposure (CVE). Pearson’s correlation and analysis of variance were used to determine the relationship between PTSD, depression, and anxiety symptoms and CVE.Results:A statistically significant relationship was found between CVE and PTSD and anxiety symptoms among participants despite their having lower rates of exposure to violent events in comparison with other studies. No association was found between violence and depression symptoms.Additionally, the presence of anxiety and depression, as well as increased age of participants, was associated with higher rates of PTSD symptoms.Conclusion:We recommend that health care providers in smaller cities, where the effects of violent crime may be underestimated or overlooked, be informed of the existence of this public health problem within their community and that they screen at-risk patients for mental health problems.
Community violence; inner city; posttraumatic stress disorder; depression; anxiety
Background
Exposure to serious forms of community violence such as experiencing or witnessing stabbings, shootings, or fights, knowing a person killed, or seeing someone killed is prevalent among inner-city residents, including children and adolescents. Studies have found that approximately 85% of inner-city youths have personally witnessed a violent act and 70% have actually been victims of a violent act [1, 2]. A study conducted in Philadelphia followed 119 inner-city children from birth,and reported that by age 7 years 75% had heard gunshots, 18% had seen a dead body,10% had witnessed a shooting or stabbing at home, and 61% worried some or a lot of the time that they might be killed [3]. A sample of more than 2000 students in an urban public school system found that more than 40%reported exposure to a shooting or stabbing within the past year [4]. In a study examining the association between community violence exposure (CVE) and asthma-related health outcomes in adults living in inner-city neighborhoods, 91% of adults reported CVE [5].
CVE has been shown to have harmful effects on physical and mental health. A 2010 study demonstrated a relationship between the incidence of community crime and childhood asthma morbidity [6]. This finding was in agreement with a previous study that was conducted across seven large US cities and reported a gradient increase in asthma-related symptom days with increasing exposure to violence among children after adjustment for income, employment status, caretaker education, housing problems, and other adverse life events [7].A similar association has been reported in adults [5].
Several studies have reported that exposure to violence affects adolescents’ blood pressure and heart rate [8—11].Abnormal blood pressures at a young age may increase these adolescents’ long-term risk of developing health problems,such as hypertension and cardiovascular disease. Additionally,a recent long-term study found that children who were exposed to two or more acts of domestic violence or were victims of frequent bullying and physical maltreatment had significantly more telomere erosion than children not exposed to such acts of violence, which may increase their susceptibility to various diseases [12]. It is reasonable to suspect that exposure to innercity violence may have similar risks.
The association between violence exposure and physical health problems may be mediated by psychological distress.Violence serves as a constant source of psychological stress,taxing vulnerable individuals and altering the hypothalamic—pituitary—adrenal axis, which affects cortical and catecholamine secretion patterns that contribute to asthma morbidity,cardiovascular dysfunction, and other health problems [7, 8,13, 14]. In regard to asthma, which is an inflammatory disease, stress can lead to changes in the levels of cytokines and other inflammatory mediators that may increase a genetically predisposed individual’s risk of developing asthma and may aggravate asthma symptoms [8, 13, 15—18]. Additionally,prolonged exposure to stress can affect the parasympathetic function, leading to bronchoconstriction and causing asthma symptoms [19—21]. Changes in parasympathetic function due to stress may also serve as another explanation for the changes observed in blood pressure and heart rate. Furthermore,Krenichyn et al. [9] and Clark et al. [10] postulate that changes in cardiovascular function may be caused by a defeated coping response of an individual due to prolonged stress resulting from exposure to violence and the individual’s acceptance that he or she cannot control or change his or her circumstance.
The link between violence and psychological stress as well as other mental health problems has been well documented. A critical 1999 study of adolescents surveyed from an inner-city neighborhood in Brooklyn observed that a distinct relationship existed between exposure to violence and posttraumatic stress disorder (PTSD) symptoms [22]. This finding is supported by other studies on the topic, including two meta-analysis studies that found a strong correlation between CVE and PTSD symptoms [1, 23—27].
Several studies have found a strong relationship between CVE and externalizing problems such as aggression, antisocial behavior, and oppositional disorder among children and adolescents [4, 26—33]. A 2008 meta-analysis study found that externalizing behavior more than any other mental health problem was related to CVE [28]. This relationship was maintained even after prior aggression or antisocial behavior had been controlled for [3, 4, 28, 32, 34].
The evidence for the relationship between CVE and internalizing problems, which include symptoms of depression and anxiety, is more complex and less clear in comparison with PTSD symptoms and externalizing behaviors [26, 27].Most studies on the topic have observed a positive correlation between CVE and symptoms of depression and anxiety among children, adolescents, and young adults [4, 25, 26, 29—31, 33,35, 36]. However, two of the studies reported only a small to moderate association between CVE and symptoms of depression and anxiety [30, 31]. Another study found no significant relationship between CVE and depression and anxiety symptoms, and two studies found no significant correlation between CVE and symptoms of depression [25, 28, 37].
The evidence is clear that inner-city youths and young adults are exposed to higher rates of community violence, which may increase their risk of suffering from mental health problems.Many of the studies on this subject have been conducted in large inner-city communities in places such as Chicago and Washington, District of Columbia, which have high rates of violent crime. The goal of this study was to determine if similar trends are observed in an inner-city community in a smaller city such as Omaha, Nebraska, where health care providers may overlook or underestimate the consequences and level of violent crime in their area of practice. The information gathered in this study could serve to educate local health care providers about the existence of this problem, which may be wrongfully viewed as being limited to large metropolitan communities.
Methods
Study design and participants
This study was designed and pursued after the principal investigator had met local community leaders who expressed concern for the growing violence in certain Omaha neighborhoods and its consequences for the youth living in those communities. The Institutional Review Board at the University of Nebraska Medical Center authorized this study (Institutional Review Board no. 486-12-EX). We worked closely with Impact One — a local grassroots organization that addresses issues affecting young people, including community violence. With its assistance, four additional local community organizations working directly with at-risk children, teenagers, and young adults were recruited to participate in this study to investigate the impact of CVE on the mental health of children and young adults. These community organizations were operating in areas of Omaha that have the highest rates of violence and poverty. Our approach to sample at-risk youths was consistent with other studies on the subject, which were also conducted in communities with high rates of violence.
The only eligibility criterion for participation in the study was that participants must belong to and receive services from one of the five community organizations that agreed to partake in the study. We conducted a group of surveys based on a series of validated tools for measuring CVE and anxiety,depression, and PTS symptoms, which are described later.Each participating organization agreed to administer the surveys and to return the data to the principal investigator for analysis. The principal investigator provided instructions to the facilitators on how each survey used in the study should be properly administered. Participants for this investigation were not excluded on the basis of age, race, or sex. Each organization administered the surveys to convenience samples of clients during group activities. The surveys were conducted in small groups.
Measurements
Demographics:Participants provided their age, sex, race,and zip code of residence.
Exposure to Violence Questionnaire:The Exposure to Violence Questionnaire (EVQ) [22] is a 21-item yes—no questionnaire used to measure the amount of community violence to which an individual has been exposed in the past year. It was developed by Mazza and Reynolds [22] for their studies on exposure to violence and exploring its relationship with mental health problems. Each item marked as “yes” indicates exposure to a violent event, and the totaled responses constitute an index.
Revised Children’s Manifest Anxiety Scale: Second Edition:The short form of the Revised Children’s Manifest Anxiety Scale: Second Edition (RCMAS-2) [38] was used to assess individuals for anxiety symptoms. The test was designed for ages 6—19 years. The short form of RCMAS-2 has good internal consistency (α=0.82) and test—retest reliability(r=0.54).It consists of 10 “yes” or “no” questions regarding how participants feel about themselves and how others may view them. At the end, all the “yes” answers are added to give a raw score and a correspondingTscore. ATscore less then 40 indicates that the participant is anxiety-free, a score between 40 and 60 indicates the participant has no more anxiety then most others, a score between 60 and 70 indicates the participant has some difficulty with anxiety, and a score higher then 70 indicates anxiety is extremely problematic.
Center for Epidemiologic Studies Depression Scale
The Center for Epidemiologic Studies Depression Scale(CES-D) [39] is a 20-question scale to measure self-reported depression. It has good internal consistency (α=0.85—0.9), and has been widely used to measure depressive symptoms; however, it is not used for diagnosis of depression. For each survey question, the CES-D uses a scale ranging from 0 to 3 to capture symptom intensity. Four of the 20 questions are scored in reverse and indicate nondepressive symptoms. The scores are then totaled, and a score of 16 or higher is considered indicative of depressive symptoms.
PTSD Checklist – Civilian Version:The PTSD Checklist — Civilian Version (PCL-C) [40] is a 17-question checklist designed for the general public to assess PTSD symptoms. It has high internal consistency (α=0.94), good retest reliability (r=0.66), and was found to be superior to other tests measuring PTSD symptoms [41]. Each item in the test uses a scale ranging from 0 to 5 to indicate symptom severity, and specific questions assess for the three types of PTSD symptoms, known as B, C, or D symptoms. There are several ways to score the test. A score of 3 or more to a question is typically considered symptomatic. A symptomatic response of at least one B item is considered positive for B symptoms,a symptomatic response of at least three C items is positive for C symptoms, and a symptomatic response of at least two D items is positive for D symptoms. To reduce the number of false positives, another recommended criterion was used,which consisted in our adding up all the scores from the 17 items and using a total score of 30 or more, which was recommended by a previous study to signify PTSD symptoms [42].Thus participants were considered to be positive for signs of PTSD if they had at least one positive item along with a total score of 30 or more.
Statistical analysis
Using IBM SPSS Statistics version 21.0, we performed attest to compare means across two categories and analysis of variance (ANOVA) to compare means across more than two categories, and Tukey’s test was used to run all parallel comparisons. More specifically, Pearson’s correlation was used to assess the association between dependent variables of PTSD scores and violence exposure and the independent variable of age. ANOVA was used to evaluate the association between dependent variables of violence exposure and PTSD scores and independent variables of sex, race, participants feeling depressed, and participants who have anxiety. ANOVA was also used to determine the association between violence exposure and PTSD symptoms. Finally, follow-up analysis using Tukey’s tests was done when we were analyzing the dependent variables ofviolence exposure and PTSD scores with different levels of anxiety (none, moderate, extreme).
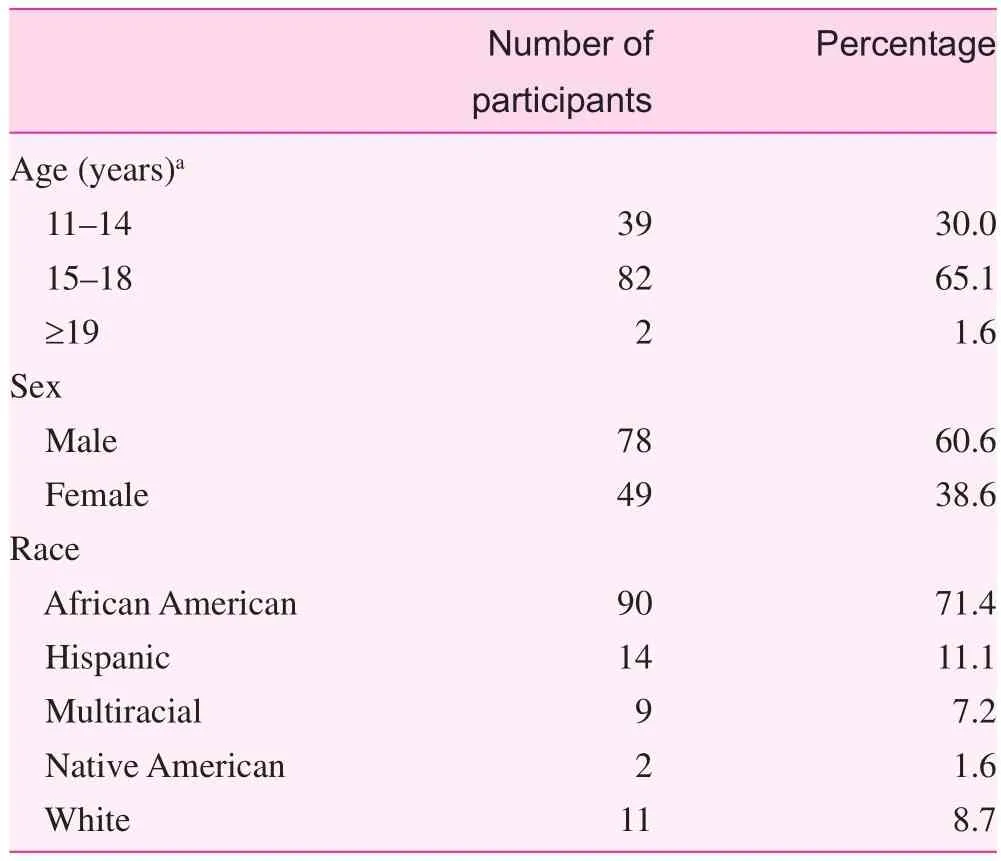
Table 1. Demographics
Results
Demographics
The total number of participants in the study was 126. The participants ranged in age from 11 to 24 years, with an average age of 15.3 years (standard deviation 1.783 years). Most of the participants (71.4%) identified themselves as African American (Table 1).
Exposure to violence
On the basis of responses to the EVQ, participants on average had been exposed to 7.47 violent events in the past year. The average number of exposures to violent events was 7.69 for males and 7.12 for females. The difference in scores between males and females in regard to violence exposure was not found to be statistically significant (P=0.522). Likewise, there was no statistically significant difference between age or race groups (P=0.849 andP=0.966, respectively). Further investigation into the responses to specific questions asked in the EVQ showed that 20.6% of participants had been physically attacked and 80.1% knew someone who had been killed in the past year (Table 2).
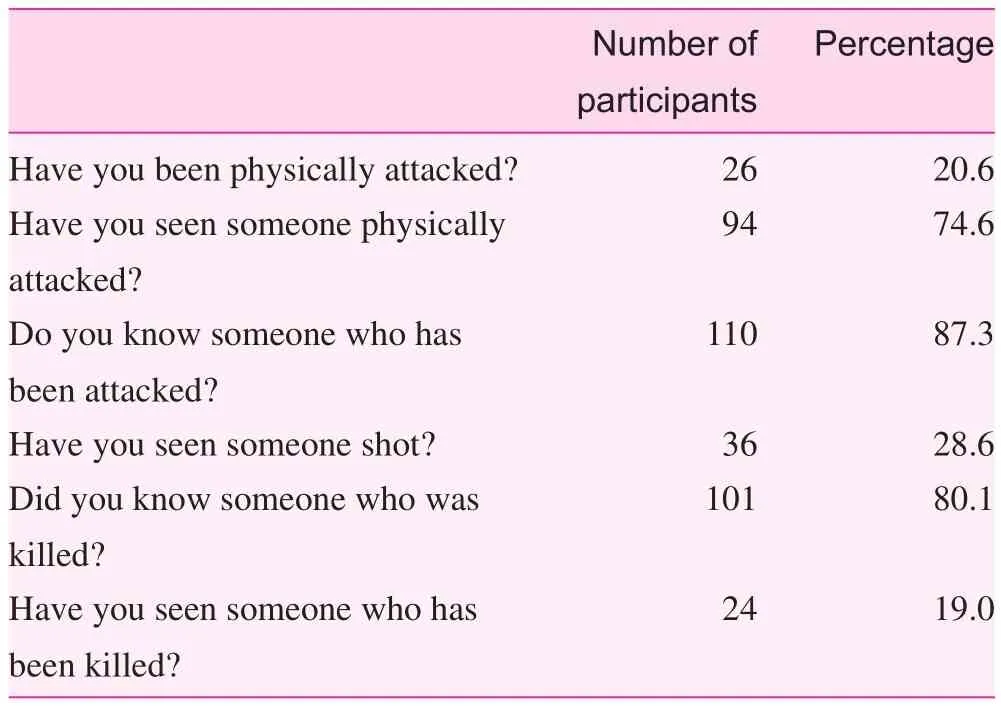
Table 2. Exposure to violent events
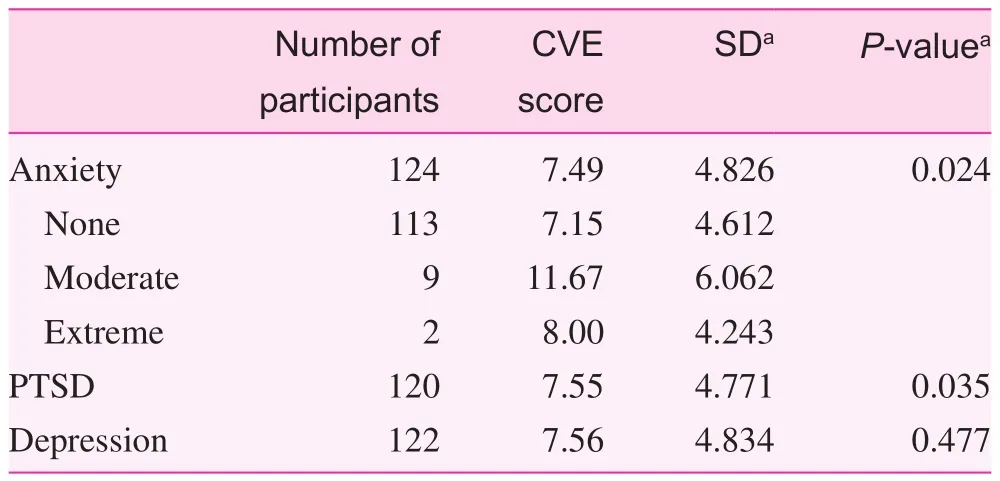
Table 3. Relationship between community violence exposure scores and anxiety, posttraumatic stress disorder, and depression
PTSD symptoms
Forty-nine participants (40.5%) were found to be positive for PTSD symptoms, 72 participants did not show signs of PTSD(59.5%), and five participants did not complete the PCL-C.
There was a significant difference (P=0.035) in violence scores and the presence or absence of PTSD symptoms(Table 3). Those who were negative for PTSD signs had an average violence score of 6.79. Participants positive for signs of PTSD had an average violence score of 8.65.
There were no statistically significant differences in total PTSD scores across different races or sexes (P=0.592 andP=0.102, respectively). However, there was a statistically significant relationship (P=0.047) between age and total PTSD scores. As the age of the participant increased, total PTSD scores increased.
Depression symptoms
There was no statistically significant difference (P=0.477)between exposure to violence scores and depression symptoms (Table 3). However, there was a significant difference(P<0.001) between those with and without depression symptoms and PTSD scores. Participants with no signs of depression had lower PTSD scores (average 29.16). Those who showed signs of depression had higher PTSD scores (average 46.94).
Anxiety symptoms
Only two participants (1.6%) were positive for extreme anxiety symptoms. Nine were positive (7.3%) for moderate anxiety symptoms. The rest of the participants (91.1%) showed no signs of anxiety. Three people did not complete the RCMAS-2.
There was a statistically significant difference (P=0.024)in CVE scores based on anxiety symptoms (Table 3). Those who showed no signs of anxiety had significantly lower exposure to violence scores (average 7.15). In comparison, those who were positive for moderate or extreme signs of anxiety had higher exposure to violence scores (average 11.67 and 8,respectively). There was no difference between moderate and extreme anxiety signs and violence scores.
Additionally, participants without signs of anxiety had significantly lower PTSD scores (average 29.5) than those with moderate or extreme signs of anxiety (average 54.56). There was no difference between moderate and extreme anxiety symptoms and PTSD scores.
Discussion
The aim of this study was to determine if mental health problems due to CVE, which has been found to be present in innercity communities of large cities with significant violent crime,is also present in the inner city of a relatively smaller city,where the level and consequences of violence may be underestimated or overlooked. The results obtained by this study had many similarities to those of previous studies conducted in Chicago, Washington, District of Columbia, and other large cities, and demonstrate that health problems due to CVE are not confined to large metropolitan areas.
The participants in this study had lower rates of exposure to violent events in comparison with other studies conducted in large inner-city communities. This is not surprising considering that Omaha has a lower violent crime index (average of 567 over 5 years) compared with other cities where similar studies have been conducted, such as in Chicago (average of 1167 over 5 years) and Philadelphia(average of 1403 over 5 years) [43]. Nonetheless, Omaha’s violent crime rate is 20.66% higher than the national level.In 2007 the city ranked third in the nation in black homicide rate, and in 2009 nearly half of all black homicide victims were aged between 16 and 24 years [44]. A look at police mappings of violent crimes shows a significant concentration of those crimes occurring in specific areas of the city,which generally involve of residents of lower socioeconomic status [45—47]. Many of the participants in this study live in these areas.
In this study, there was a distinct relationship between PTSD symptoms and CVE. This finding is in agreement with previous studies that have consistently shown a correlation between violence exposure and PTSD [1, 23—27]. Conflicting observations are found in the literature as to whether there any differences among males and females and PTSD symptoms.A 1993 study found females were more vulnerable to having PTSD symptoms after being a victim of violence or witnessing violence compared with males [1]. However, other studies,including a 2009 meta-analysis study, have shown few sex differences [27, 48, 49]. In our study, we did not find any statistical difference between males and females and total PTSD scores.
We did observe that as the age of participants increased for those who tested positive for PTSD symptoms, their total PTSD scores increased as well. Previous studies have also reported increased PTSD symptomatology with increased age [50, 51]. Additionally, a meta-analysis study showed that there is evidence that exposure to violence has a greater effect on mental health of adolescents in comparison with children[27]. It is reasonable to speculate that adolescents and young adults are susceptible to more violence exposure during their lifetime, or put another way, have experienced more chronic violence exposure, which may worsen PTSD signs and/or severity.
Another explanation may be that older participants are at increased risk of other mental health problems, such as depression and anxiety, the presence of which may exacerbate PTSD symptoms. In our study, those who tested positive for anxiety or depression symptoms had higher total PTSD scores.Many of the symptoms required for the diagnosis of anxiety and depression according toDSM-IVare present in PTSD, and these mental health problems along with others may affect one another in a complex manner.
Further understanding of this complex relationship between different mental health problems and CVE is demonstrated in Mazza and Reynolds’s study [22] in which they found that when PTSD and suicidal ideation were controlled for, the significant positive association between CVE and depression lost significance. Multiple other studies have also found no relationship between depression and CVE [25, 28,37]. Furthermore, Mazza and Reynolds [22] found that the relationship between PTSD and CVE was still significant even after controlling for depression and suicidal ideation.They went on to suggest that the relationship between CVE and depression symptoms may be indirect and that PTSD may serve as a mediating variable between exposure to violence and depression [22].
A potential limitation of this study is that members from the participating community organizations administered the surveys. Although administrators were instructed on how to administer each survey, they were not supervised, and it is possible that the proper instructions on filling in the survey were not given to all or some participants. For example, the EVQ specifically asked about violent events that have occurred in the past year. If the administrators did not tell the participants this or if participants failed to read the instructions, it is possible that they may have interpreted the questions to pertain to their lifetime or the past week.
Several studies have looked into factors that may help prevent at-risk youths from developing mental health problems due to CVE [14, 52]. They have shown that child characteristics, parental support, school support, and peer support can help protect individuals [52—54]. This suggests that parents,teachers, and local community leaders and organizations can serve as major players in addressing this problem. However,given that this issue deals with significant health problems, it is reasonable to recommend that health care providers can and should also play a crucial role.
The clinical implications given the findings of this and other studies are that health care providers must be aware of the consequences of CVE for an individual’s physical and mental well-being. The Adverse Childhood Experiences study conducted by Kaiser Permanente and the Centers for Disease Control and Prevention showed that children who suffered from adverse and traumatic childhood experiences were likelier to have chronic diseases and mental health problems as adults [55]. Health care providers working in an urban setting should avoid being misled by focusing on their city’s overall violent crime rate and should instead be aware of the crime rate of the communities and neighborhoods where their patients reside.
It is recommended that providers screen at-risk patients for CVE and mental health disorders, such as PTSD, anxiety,depression, and externalizing behaviors, so as to identify susceptible patients who require preventive measures and those who have already developed problems that require proper psychiatric referrals and treatment, which may include, but are not limited to, therapy sessions, developing coping mechanisms,lifestyle changes, and medications. Additionally, providers,particularly psychiatrists and primary care physicians, should be encouraged to work closely with local community organizations and leaders that serve at-risk youths and young adults to provide these screening tests. By working closely with such groups and individuals, providers can reach more at-risk youths and young adults and will have a better understanding of their patient’s environment and needs. Additionally,health care workers can help train these organizations and individuals to better serve at-risk youths and young adults by instructing them how to teach coping mechanisms, conduct group therapy sessions, etc. This approach falls in line with the Attorney General’s Task Force for Children Exposed to Violence assertion that violence is a public health crisis,which thus demands that health care providers join teachers,parents, public health workers, and community organizations and leaders to address this problem in a more comprehensive and efficient manner [56].
Acknowledgments
Thanks are due to the Hope Center for Kids, Boys and Girls Clubs of the Midlands (Carl & Joyce Mammel South Unit),Eastern Nebraska Community Action Partnership, and Urban League of Nebraska for participating in this study. Thanks are also due to Iqbal Ahmad and Johnie Rose for critical reading of the manuscript.
Conflicts of interest
The authors declare no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author contributions
Dr. Faraz Ahmad — principal investigator. Participated in the study conception and design of the study, acquisition of data,analysis and interpretation of data, drafting of manuscript, and critical revision.
Dr. Jim Medder participated in the study conception and design of the study and critical revision.
Dr. Jenenne Geske participated in the analysis and interpretation of data.
Janette Taylor participated in the acquisition of data.
Dr. Ruth Margalit participated in the drafting of the manuscript and critical revision.
Significance statement
Several studies have reported on the association between community violence exposure and mental health problems. These studies have been conducted in large inner-city communities,which have some of the highest violent crime rates in America.The purpose of this study was to determine if similar trends are present in smaller inner-city communities with relatively less violent crime. Indeed, our study did demonstrate that a similar association was present between community violence exposure and mental health issues in a smaller inner-city community with less violent crime. The significance of this finding is to challenge the view that mental health issues due to community violence exposure is confined to only large urban communities with above average levels of violence.
1. Fitzpatrick K, Boldizar J. The prevalence and consequences of exposure to violence among African-American youth. J Am Acad Child Adolesc Psychiatry 1993;32(2):424—30.
2. Schubiner H, Scott R, Tzelepis A. Exposure to violence among inner-city youth. J Adolesc Health 1993;14(3):214—9.
3. Hunt H, Malmud E, Brodsky N, Giannetta J. Exposure to violence: psychological and academic correlates in child witnesses.Arch Pediatr Med 2001;155(12):1351—6.
4. Schwab-Stone M, Ayer T, Kasprow W, Voyce C, Barone C,Shriver T, et al. No safe haven: a study of violence exposure in an urban community. J Am Acad Child Adolesc Psychiatry 1995;43(10):1343—52.
5. Apter A, Garcia L, Boyd R, Wan X, Bogen D, Have T. Exposure to community violence is associated with asthma hospitalizations and emergency department visits. J Allergy Clin Immunol 2010;126(3):552—7.
6. Gupta R, Zhang X, Springston E, Sharp L, Curtis L, Shalowitz M, et al. The association between community crime and childhood asthma prevalence in Chicago. Ann Allergy Asthma Immunol 2010;104(4):299—306.
7. Wright R, Mitchell H, Visness C, Cohen S, Stout J, Evans R,et al. Community violence and asthma morbidity: the inner-city asthma study. Am J Public Health 2004;94(4):625—32.
8. Wilson D, Kliewer W, Teasley N, Plybon L, Sica D. Violence exposure, catecholamine excretion, and blood pressure nondipping status in African American male versus female adolescents.Psychosom Med 2002;64(6):906—15.
9. Krenichyn K, Saegert S, Evans G. Parents as moderators of psychological and physiological correlates of inner-city children’s exposure to violence. J Appl Dev Psychol 2001;22(6):581—602.
10. Clark R, Benkert R, Flack J. Violence exposure and optimism predict task-inducted changes in blood pressure and pulse rate in a normotensive sample of inner-city black youth. Psychosom Med 2006;68(1):73—9.
11. Murali R, Chen E. Exposure to violence and cardiovascular and neuroendocrine measures in adolescents. Ann Behav Med 2005;30(2):155—63.
12. Shalev I, Moffitt T, Sugden K, Williams B, Houts R, Danese A,et al. Exposure to violence during childhood is associated with telomere erosion from 5 to 10 years of age: a longitudinal study.Mol Psychiatry 2013;18(5):576—81.
13. Wright R, Steinbach S. Violence: an unrecognized environmental exposure that may contribute to greater asthma morbidity in high risk inner-city populations. Environ Health Perspect 2001;109(10):1085—9.
14. Lynch M. Consequences of children’s exposure to community violence. Clin Child Fam Psychol Rev 2003;6(4):265—74.
15. Kiecolt-Glaser J, Glaser R. Psychosocial moderators of immune function. Ann Behav Med 1987;9(2):16—20.
16. Kiecolt-Glaser, J, Glaser R. Stress and immune function in humans.In: Ader R, Felten D, Cohen N, editors. Psychoneuroimmunology II. San Diego: Academic Press; 1991. pp. 849—67.
17. Cohen S, Tyrell D, Smith P. Psychological stress and susceptibility to the common cold. N Engl J Med 1991;325:606—12.
18. Graham N, Douglas R, Ryan P. Stress and acute respiratory infection. Am J Epidemiol 1986;124(3):389—401.
19. Gelhorn E. The neruophysiological basis of anxiety: a hypothesis. Perspect Biol Med 1965;8(4):488—515.
20. Vingerhoets A. The role of the parasympathetic division of the autonomic nervous system in stress and the emotions. Int J Psychosom 1985;32(3):28—34.
21. Nadel J, Barne P. Autonomic regulation of the airways. Annu Rev Med 1984;35:451—67.
22. Mazza J, Reynolds W. Exposure to violence in young inner-city adolescents: relationships with suicidal ideation, depression,and PTSD symptomatology — posttraumatic stress disorder. J Abnorm Child Psychol 1999;27(3):203—13.
23. Horowitz K, Weine S, Jekel J. PTSD symptoms in urban adolescent girls: compounded community trauma. J Am Acad Child Adolesc Psychiatry 1995;34(10):1353—61.
24. Cuffe S, Addy C, Garrison C, Waller J, Jackson K, McKeown R, et al. Prevalence of PTSD in a community sample of older adolescents. J Am Acad Child Adolesc Psychiatry 1998;37(2):147—54.
25. Cooley-Quille M, Boyd R, Frantz E, Walsh J. Emotional and behavioral impact of exposure to community violence in innercity adolescents. J Clin Child Psychol 2001;30(2):199—206.
26. McDonald C, Richmond T. The relationship between community violence exposure and mental health symptoms in urban adolescents. J Psychiatr Ment Health Nurs 2008;15(10):833—49.
27. Fowler P, Tompsett C, Braciszewski J, Jacques-Tiura A, Baltes B.Community violence: a meta-analysis on the effect of exposure and mental health outcomes of children and adolescents. Dev Psychopathol 2009;21(1):227—59.
28. Farrell A, Bruce S. Impact of exposure to community violence on violent behavior and emotional distress among urban adolescents. J Clin Child Psychol 1997;26(1):2—14.
29. Lynch M, Cicchetti D. An ecological—transactional analysis of children and contexts: the longitudinal interplay among child maltreatment, community violence, and children’s symptomology. Dev Psychopathol 1998;10(2):739—59.
30. Gorman-Smith D, Tolan P. The role of exposure to community violence and developmental problems among inner-city youth.Dev Psychopathol 1998;10(1):101—16.
31. Schwab-Stone M, Chen C, Greenberger E, Silver D, Lichtmn J, Voyce C. No safe haven II: the effects of violence exposure on urban youth. J Am Acad Child Adolesc Psychiatry 1999;38(4):359—67.
32. Miller L, Wasserman G, Neugebauer R, Gorman-Smith D,Kamboukos D. Witnessed community violence and antisocial behavior in high-risk urban boys. J Clin Child Psychol 1999;28(1):2—11.
33. Gorman-Smith D, Henry D, Tolan P. Exposure to community violence and violence perpetration: the protective effects of family functioning. J Clin Child Adolesc Psychol 2004;33(3):439—49.
34. DuRant R, Cadenhead C, Pendergrast R, Slavens G, Linder C.Factors associated with the use of violence among urban black adolescents. Am J Public Health 1994;84(4):612—7.
35. Kliewer W, Lepore S, Oskin D, Johnson P. The role of social and cognitive processes in children’s adjustment to community violence. J Consult Clin Psychol 1998;66(1):199—209.
36. Rosenthal B. Exposure to community violence in adolescence: trauma symptoms. Adolescence 2000;35(138):271—84.
37. Overstreet S, Dempsey M, Graham D, Moely B. Availability of family support as a moderator of exposure to community violence. J Clin Child Psychol 1999;28(2):151—9.
38. Reynolds C, Richmond B. Revised children’s manifest anxiety scale. 2nd ed. Torrance: Western Psychological Services;2008.
39. Radloff S. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977;1(3):385—401.
40. Weathers F, Litz B, Huska J, Keane T. Posttraumatic stress disorder checklist. Boston: National Center for PTSD, Behavioral Science Division; 1994.
41. Cobybeare D, Behar E, Solomon A, Newman M, Borkovec T. The PTSD Checklist-Civilian Version: reliability, validity, and factor structure in a nonclinical sample. J Clin Psychol 2012;66(6):699—713.
42. Bliese P, Wright K, Adler A, Cabrera O, Castro C, Hoge C.Validating the primary care posttraumatic stress disorder Screen and the posttraumatic stress disorder checklist with soldiers returning from combat. J Consul Clin Psychol 2008;76(2):272—81.
43. CityRating.com. Crime Statistics Report (U.S. Crime Rates).2017 [accessed 2017 February 22]. Available from: http://www.cityrating.com/crime-statistics/.
44. Cordes H. Epidemic of poverty, violence. Omaha World- Herald.February 21, 2010.
45. Crimemapping.com. Crimemapping. 2016 [accessed 2017 February 22]. Available from: https://www.crimemapping.com/Share/eebe9690b9a140d5b94669990612dff2.
46. City-Data.com. Crime rate in Omaha, Nebraska. 2017 [accessed 2017 February 22]. Available from: https://www.neighborhoodscout.com/ne/omaha.
47. Neighborhoodscout.com. Neighborhood Scout. 2017 [accessed 2017 February 22]. Available from: https://www.neighborhoodscout.com/ne/omaha/crime.
48. Pynoos S, Frederick C, Nader C, Arroyo W, Steinberg A, Eth S,et al. Life threat and post-traumatic stress in school-aged children. Arch Gen Psychiatry 1987;44(12):1057—63.
49. Schwarz E, Kowalski J. Malignant memories: PTSD in children and adults after a school shooting. J Am Acad Child Adolesc Psychiatry 1991;30(6):936—44.
50. Merikangas K, He J, Burstein M, Swanson S, Avenevoli S, Cui L, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication—Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry 2010;49(10):980—9.
51. Denson T, Marshall G, Schell T, Jaycox L. Predictors of posttraumatic distress 1 year after exposure to community violence: the importance of acute symptom severity. J Consult Clin Psychol 2007;75(5):683—92.
52. Mazza J, Overstreet S. Children and adolescents exposed to community violence: a mental health perspective for school psychologists. School Psych Rev 2000;29(1):86—101.
53. Hill H, Madhere S. Exposure to community violence and African-American children: a multidimensional model of risks and resources. J Community Psychol 1996;24(1):26—43.
54. O’Donnell D, Schwab-Stone M, Muyeed A. Multidimensional resilience in urban children exposed to community violence.Child Dev 2002;73(4):1265—82.
55. Felitti V, Anda R, Nordenberg D, Williamson D, Spitz A, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) study. Am J Prev Med 1998;14(4):245—58.
56. Listenbee R, Torre J, Boyle G, Cooper S, Deer S, Durfee D,et al. Report of the attorney general’s national task force on children exposed to violence. Washington: Department of Justice; 2012.
Faraz Ahmad, MD
Case Western University, School of Medicine, 2109 Adelbert Rd,Cleveland, OH 44106, USA
Tel.: +1-402-3215424
E-mail: fxa117@case.edu
11 March 2017;
Accepted 15 June 2017
杂志排行
Family Medicine and Community Health的其它文章
- Health is primary
- Assessing the accuracy of patient report of the 5As (ask, assess,advise, assist, and arrange) for smoking cessation counseling
- Burden of road traffic accidents in Nepal by calculating disability- adjusted life years
- Effect of an educational intervention and parental vaccine refusal forms on childhood vaccination rates in a clinic with a large Somali population
- Tobacco cessation pharmacotherapy use among racial/ethnic minorities in the United States: Considerations for primary care
- Understanding cultures beyond medicine
