心搏呼吸骤停患者心肺复苏流程选择的探讨
2017-12-21马春茂杨英
马春茂 杨英
(彭州市人民医院急诊科,四川彭州 611930)
心搏呼吸骤停患者心肺复苏流程选择的探讨
马春茂 杨英
(彭州市人民医院急诊科,四川彭州 611930)
目的:观察不同心肺复苏流程对心搏呼吸骤停患者复苏成功率的影响,为心搏呼吸骤停患者心肺复苏流程的选择提供参考依据。方法:回顾我院2015年1月至2017年1月期间抢救的心搏呼吸骤停患者情况,对资料完整的192例患者进行分析。按照患者心肺复苏流程,将接受胸部按压-气道-呼吸(C-A-B)者纳入CAB组,将接受电除颤-复苏药物(D)者纳入D组,将接受电除颤-复苏药物-胸部按压(D-C)者纳入DC组,将接受气道-呼吸-胸部按压-复苏药物(A-B-C-D)者纳入ABCD组,比较各组患者复苏成功率、复苏存活率以及复苏成功患者自主循环恢复时间,探讨心肺复苏流程的优化。结果:CAB组复苏成功率、复苏存活率均高于另3组,D组、DC组复苏成功率、复苏存活率均高于ABCD组,差异均有统计学意义(P<0.05)。CAB组自主循环恢复时间低于另3组,D组、DC组自主循环恢复时间亦低于ABCD组,差异均有统计学意义(P<0.05)。结论:对于心搏呼吸骤停患者而言,心肺复苏流程中强调胸部按压的优先级,对于提高复苏成功率、存活率,缩短自主循环恢复时间具有重要意义。
心搏呼吸骤停;心肺复苏;流程;成功率
当前我国院外心肺复苏的成功率仅为1%~18%,院内心肺复苏成功率亦只有12%~24%[1]。因此,如何提高心肺复苏成功率,一直是我国乃至全球医务工作者共同面对的挑战。心搏呼吸骤停的院内发生率接近50%,多数患者会在症状发生后的2 h内死亡[2]。复苏流程选择不当、症状出现后复苏开展时间较晚均被认为是影响心肺复苏成功率的危险因素[3-4]。此次研究就心肺复苏流程选择对心肺复苏成功率的影响进行了回顾性分析,希望能为优化复苏流程提供参考。
1 资料与方法
1.1 一般资料
分析2015年1月至2017年1月192例心搏呼吸骤停患者,排除临床资料不完整者。患者原发病包括脑源性疾病、心源性疾病、肺源性疾病、肾源性疾病以及创伤中毒性疾病等。患者均按照美国心脏协会(AHA)指南、国际心肺复苏(CPR)指南及心血管急救(ECC)指南要求接受心肺复苏[5-6],主要操作包括心脏胸外按压(频次100~120次/min,深度50~60 mm,按压放松比1:1,按压呼吸比30:2)、呼吸道疏通与清理、气管插管、气囊面罩呼吸、电除颤、静脉或气管内注射肾上腺素、吸氧等,每5次心肺复苏流程后检查生命体征,对于心肺复苏成功者,明确其病因并开展预防再发的对症治疗,以及维持血液循环、维持有效通气功能、低温、脑复苏、防治继发感染等提高长期生存和神经恢复的治疗[7]。按照患者心肺复苏流程,将接受胸部按压-气道-呼吸(C-A-B)者纳入CAB组(n=51),将接受电除颤-复苏药物(D)者纳入D组(n=40),将接受电除颤-复苏药物-胸部按压(D-C)者纳入DC组(n=38),将接受气道-呼吸-胸部按压-复苏药物(A-B-C-D)者纳入ABCD组(n=63)。
1.2 判别标准
复苏成功判断标准[8]:1)自主循环恢复,窦性心律恢复;2)面色由发绀转为红润;3)出现规则或不规则自主呼吸,或行器械通气可将血氧饱和度(SpO2)维持在90%以上;4)瞳孔由大变小,眼球活动或光反射恢复;5)脑复苏成功,意识恢复,生命体征平稳,未见严重脑功能障碍遗留。复苏存活判断标准[9]:意识转为清晰,心肺脑功能基本恢复至发病前水平,存活时间≥2周。
1.3 统计学分析
对本临床研究的所有数据采用SPSS18.0进行分析,性别、病因、复苏成功率等计数资料以(n/%)表示,并采用χ2检验,年龄、自助循环恢复时间等计量资料以()表示,并采用t检验或F检验,以P<0.05为差异有统计学意义。
2 结果
2.1 复苏率
CAB组复苏成功率高于D组、DC组、ABCD组,D组、DC组复苏成功率高于ABCD组,差异有统计学意义(P<0.05)。见表1。
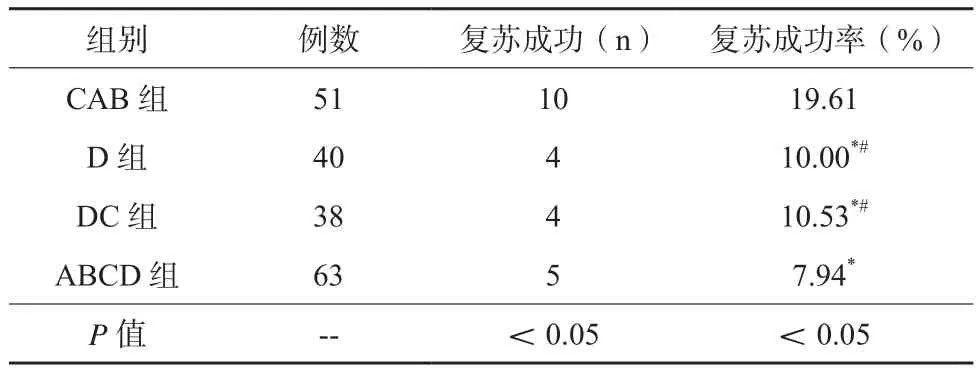
表1 四组患者复苏成功率比较
CAB组复苏存活率9.80%高于其余3组,D组复苏存活率5.00%、DC组存活率5.26%高于ABCD组的1.59%,差异有统计学意义(P<0.05)。
2.2 自主循环恢复时间
CAB组自主循环恢复时间为(7.71±2.64)min,低于其余 3 组,D 组、DC 组的(10.35±3.81)min、(10.08±3.44)min亦低于ABCD组的(13.86±4.04)min,差异有统计学意义(P<0.05)。
3 讨论
心肺复苏是临床一线急救时常用且最为重要的措施,由于心脏停搏、呼吸骤停并不意味着患者生命的结束,故及时、有效的复苏措施能够促进心跳、呼吸以及中枢神经功能的恢复,挽救患者生命[10]。当前发达国家每年投入大量资金用于心肺复苏知识、技能的培训与普及,使患者院外抢救成功率达到60%以上,但这一数字在我国仍处于较低水平,且存活患者中仅有20%可获得完全康复,多数患者遗留长期并发症,生活质量受到明显影响[11-12]。
21世纪初,各类心肺复苏指南均支持A-B-C-D流程,即首先注重保持呼吸道通畅,而后实施人工呼吸、胸外按压、电除颤和给予复苏药物,经过多年实践,这一心肺复苏流程在救治心搏呼吸骤停患者方面发挥了巨大作用,但也显现出某些不足:由于A-B-C-D框架过分强调呼吸道通畅,院前心肺复苏极易出现盲目等待气管插管现象,造成后续复苏流程滞后,影响救治效果[13];与此同时,非专业医务人员在开展心肺复苏时,实施口对口呼吸效果有限,待急救人员到达后,复杂的插管过程也使得最佳救治时机进一步贻误,最终造成复苏失败、患者死亡[14]。本研究结果示,接受A-B-C-D规范流程救治的63例患者,其复苏成功率仅为7.94%,自主循环恢复时间最高且死亡率高达98.41%,说明了传统框架在心搏呼吸骤停救治环节的局限性。
鉴于心肺复苏实践过程中救助对象状况、现场条件的变化以及救援人员多样,近年来各类指南对于心肺复苏流程的推荐呈多样化发展,如2005年心肺复苏指南即指出,对于无意愿或无能力行口对口呼吸者,可直接跳过这一流程,直接实施胸外按压[15]。在这一理念的支持下,当前临床已发展出C-A-B、D、D-C等多种心肺复苏流程,此次研究就各种流程的效果进行了对比,结果显示,D、D-C在心搏呼吸骤停救治中的作用均优于传统流程,其可能的机制为:在未开放气道的前提下,心搏呼吸骤停患者喘息样呼吸、胸廓被动恢复能够提供少量气体交换,也为其他后续步骤的改善奠定了一定基础[16];同时,口对口呼吸所致胃内容物反流风险上升、有效胸外按压时间减少,也是导致A-B-C-D流程救治效果不佳的重要原因[17]。
与D、D-C流程相比,C-A-B流程在救治心搏呼吸骤停方面发挥了最为显著的效果,这一流程将患者自主循环恢复时间缩短至10 min以内,且将患者复苏成功率、复苏存活率提升至19.61%、9.80%,其优势在于:多数心搏呼吸骤停患者具有可除颤心律,将胸外按压置于心肺复苏流程前置位,可使机体血液供应迅速恢复,而在保证持续胸外按压的同时,逐渐开放气道、应用救治药物,能够有效增加全身循环阻力,利于心搏、呼吸的及时恢复[18]。
综上所述,C-A-B流程对心搏呼吸骤停患者的救治效果明显优于其他流程,可作为心肺复苏的首选方案予以推广,但在实际应用中,不应局限于C-A-B流程框架,需按照现场及患者实际情况灵活组合各类复苏程序。
[1] RO Y S, DO SHIN S, LEE Y J, et al. Effect of dispatcherassisted cardiopulmonary resuscitation program and location of out-of-hospital cardiac arrest on survival and neurologic outcome[J]. Ann Emerg Med, 2017, 69(1): 52-61.
[2] WALDRON N, JOHNSON C E, SAUL P, et al. Development of a video-based education and process change intervention to improve advance cardiopulmonary resuscitation decisionmaking[J]. BMC Health Serv Res, 2016, 16(1): 555.
[3] FIELD R A, FRITZ Z, BAKER A, et al. Systematic review of interventions to improve appropriate use and outcomes associated with do-not-attempt-cardiopulmonary-resuscitation decisions[J]. Resuscitation, 2014, 85(11): 1418-1431.
[4] COUPER K, KIMANI P K, ABELLA B S, et al. The systemwide effect of real-time audiovisual feedback and postevent debriefing for in-hospital cardiac arrest: the cardiopulmonary resuscitation quality improvement initiative[J]. Crit Care Med,2015, 43(11): 2321.
[5] SHUSTER M, LIM S H, DEAKIN C D, et al. Part 7: CPR techniques and devices: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations[J]. Circulation,2010, 122(2):338-44.
[6] SONG K J, DO SHIN S, PARK C B, et al. Dispatcher-assisted bystander cardiopulmonary resuscitation in a metropolitan city:A before-after population-based study[J]. Resuscitation, 2014,85(1): 34-41.
[7] HAZINSKI M F. Measured Progress in Cardiopulmonary Resuscitation[J]. Circulation, 2016, 134(25): 2043-2045.
[8] BISWAS S, ALPERT A, LYON M, et al. Cardiopulmonary Resuscitation Complicated by Traumatic Hepatic Laceration:A Case Report and Review of Literature[J]. J Med Case, 2017,8(3): 93-97.
[9] KRAMER-JOHANSEN J, EDELSON D H, KOHLER K, et al. Uniform reporting of measured quality of cardiopulmonary resuscitation (CPR).[J]. Resuscitation, 2007, 74(3):406-417.
[10] NA J U, HAN S K, CHOI P C, et al. Effect of metronome rates on the quality of bag-mask ventilation during metronomeguided 30: 2 cardiopulmonary resuscitation: A randomized simulation study[J]. World J Emerg Med, 2017, 8(2): 136.
[11] CHESKES S, SCHMICKER R H, VERBEEK P R, et al. The impact of peri-shock pause on survival from out-of-hospital shockable cardiac arrest during the Resuscitation Outcomes Consortium PRIMED trial[J]. Resuscitation, 2014, 85(3): 336-342.
[12] SU L, SPAEDER M C, JONES M B, et al. Implementation of an extracorporeal cardiopulmonary resuscitation simulation program reduces extracorporeal cardiopulmonary resuscitation times in real patients[J]. Pediatr Crit Care Med, 2014, 15(9):856-860.
[13] 冯璐, 马青变. 心肺复苏后患者神经功能预后的预测策略研究进展[J]. 中华急诊医学杂志, 2016, 25(10): 1341-1344.
[14] BÖTTIGER B W, BERNHARD M, KNAPP J, et al. Influence of EMS-physician presence on survival after out-of-hospital cardiopulmonary resuscitation: systematic review and metaanalysis[J]. Crit Care, 2016, 20(1): 4.
[15] 沈洪. 概述:国际CPR与ECC指南2000-2005[C]// 首届北京国际急诊医学暨奥运急救论坛. 2007.
[16] DAMEFF C, VADEBONCOEUR T, TULLY J, et al. A standardized template for measuring and reporting telephone pre-arrival cardiopulmonary resuscitation instructions[J].Resuscitation, 2014, 85(7): 869-873.
[17] KWON M J, KIM E H, SONG I K, et al. Optimizing Prone Cardiopulmonary Resuscitation: Identifying the Vertebral Level Correlating With the Largest Left Ventricle Cross-Sectional Area via Computed Tomography Scan[J]. Anesth Analg, 2017,124(2): 520-523.
[18] GEOCADIN R G, WIJDICKS E, ARMSTRONG M J, et al. Practice guideline summary: Reducing brain injury following cardiopulmonary resuscitation Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology[J].Neurology, 2017, 88(22): 2141-2149.
Discussion on the selection of cardiopulmonary resuscitation processes in patients with breath and cardiac arrest
MA Chunmao, YANG Ying. (Department of Emergency, Pengzhou People’s Hospital,Pengzhou 611930 china)
Objective: The objective of this study was to observe the effect of different cardiopulmonary resuscitation processes on the success rate of resuscitation in patients with breath and cardiac arrest, and to provide references for the selection of cardiopulmonary resuscitation processes in patients with breath and cardiac arrest. Methods: A total sample of 192 cases with complete data of patients with breath and cardiac arrest rescued in our hospital between January 2015 and January 2017 were retrospectively analyzed. According to patients’ cardiopulmonary resuscitation process, patients receiving chest compressions-airway-breathing (C-A-B) were included in CAB group, patients receiving defibrillationresuscitation drugs (D) were included in D group, patients receiving defibrillation-resuscitation drugs-chest compressions(D-C) were included in DC group, patients receiving airway-breathing-chest compressions-resuscitation drugs were included in ABCD group. The success rate of resuscitation, the survival rate of resuscitation and the recovery time of spontaneous circulation in patients with successful resuscitation were compared among four groups, and the optimization of cardiopulmonary resuscitation process was also discussed. Results: The success rate and the survival rate of resuscitation of CAB group were both higher than those of the other three groups. The success rate and the survival rate of resuscitation of D group and DC group were all higher than that of ABCD group, and the differences were statistically significant (P<0.05). The recovery time of spontaneous circulation of CAB group was shorter than that of the other three groups. The recovery time of spontaneous circulation of D group and DC group were also shorter than that of ABCD group, and the differences were statistically significant (P<0.05). Conclusions: For patients with breath and cardiac arrest, the priority of chest compressions in cardiopulmonary resuscitation process is of great importance for improving the success rate and the survival rate of resuscitation, and shortening the recovery time of spontaneous circulation.
breath and cardiac arrest; cardiopulmonary resuscitation; process; success rate
R605
A
2095-5200(2017)06-020-03
10.11876/mimt201706008
马春茂,本科,主治医师,研究方向:急诊临床,Email:375654496@qq.com。
