骨性III类错采用正畸联合双颌手术治疗前后上气道变化的Meta分析
2017-11-11陈德余郭婉露王豫蓉
陈德余 郭婉露 王豫蓉

陈德余 郭婉露 王豫蓉

骨性III类错牙合; 正畸治疗; 正颌手术; 气道; Meta分析

1 材料与方法
1.1 纳入排除标准

1.1.3 干预措施 采用双颌手术(上颌行Lefort I型前徙,下颌行SSRO或IVRO后退)并配合术前、术后正畸治疗。排除单独上颌前徙或单独下颌后退者;排除正畸正颌外还联合其他治疗方式者。
1.1.4 结局指标 鼻咽部体积(nasopharyngeal volume,NPV)、口咽部体积(oropharyngeal volume,OPV)及鼻咽口咽总体积(total volume,TV)的变化值。纳入测量方法采用CT、CBCT或是其它三维测量方式者。排除采用头颅侧位片等二维手段作为测量方式者。
1.2 文献检索
1.2.1 检索来源 电子检索中英文数据库:Cochrane library,Embase,PubMed,Web of Science、中国生物医学文献数据库(CBM)、万方数据库(Wanfang)、中文科技期刊数据库(VIP)、中国期刊全文数据库(CNKI)。手动检索中华正畸学杂志、中华口腔医学杂志以及中国循证医学等。并追踪已检索文献的参考文献以查缺补漏。语言包括英语和汉语。检索截止时间2015-12。
1.2.2 检索策略 英文检索式:#1.skeletal class III malocclusion;#2.mandibular prognathism;#3.#1 OR #2;#4.orthodontic*;#5.orthognathic surgery;#6.#3 AND #4 AND #5;#7.airway;#8.phayrngeal space;#9.pharynx;#10.OR(7-9);#11.#6 AND #10。中文检索式:#1.骨性III类;#2.下颌前突;#3.#1 OR #2;#4.正畸治疗;#5.正颌治疗;#6. #3 AND #4 AND #5;#7.气道;#8.咽部;#9. #7 OR #8;#10. #6 AND #9。
1.3 文献筛选及资料提取
2 位评价者独立地进行文献筛选及数据提取。然后资料汇总,遇分歧则通过讨论解决或请第三方介入。本研究主要提取信息包括:第一研究作者、样本量、发表时间、研究对象的性别及年龄、干预措施、结局指标。
1.4 质量评价
采用Cochrane协作网推荐的NOS(newcastle-ottawa scale)量表[5]对纳入文献进行质量评价:总分9 分,高质量>7 分,中等质量6~7 分,低质量≤5 分。
1.5 统计分析
数据分析采用Revman 5.3软件完成。本研究纳入文献的结果为连续型变量资料,效应量选择加权均数差(WMD)和95%CI。异质性检验采用I2检验[6],只要I2小于50%,异质性可被接受[7];I2大于50%时需要首先解释异质性来源,可通过亚组分析、随机效应模型等处理。发表偏倚的检测采用漏斗图分析。
2 结 果
2.1 文献检索流程及结果
按照检索策略初步得到文献488 篇(中文281 篇,英文207 篇),排除重复文献220 篇,阅读题目和摘要排除215 篇,仔细阅读全文排除44 篇,最终纳入文献9 篇[8-16](英文7 篇,中文2 篇)。
2.2 纳入研究特征及质量评价

2.3 Meta分析结果



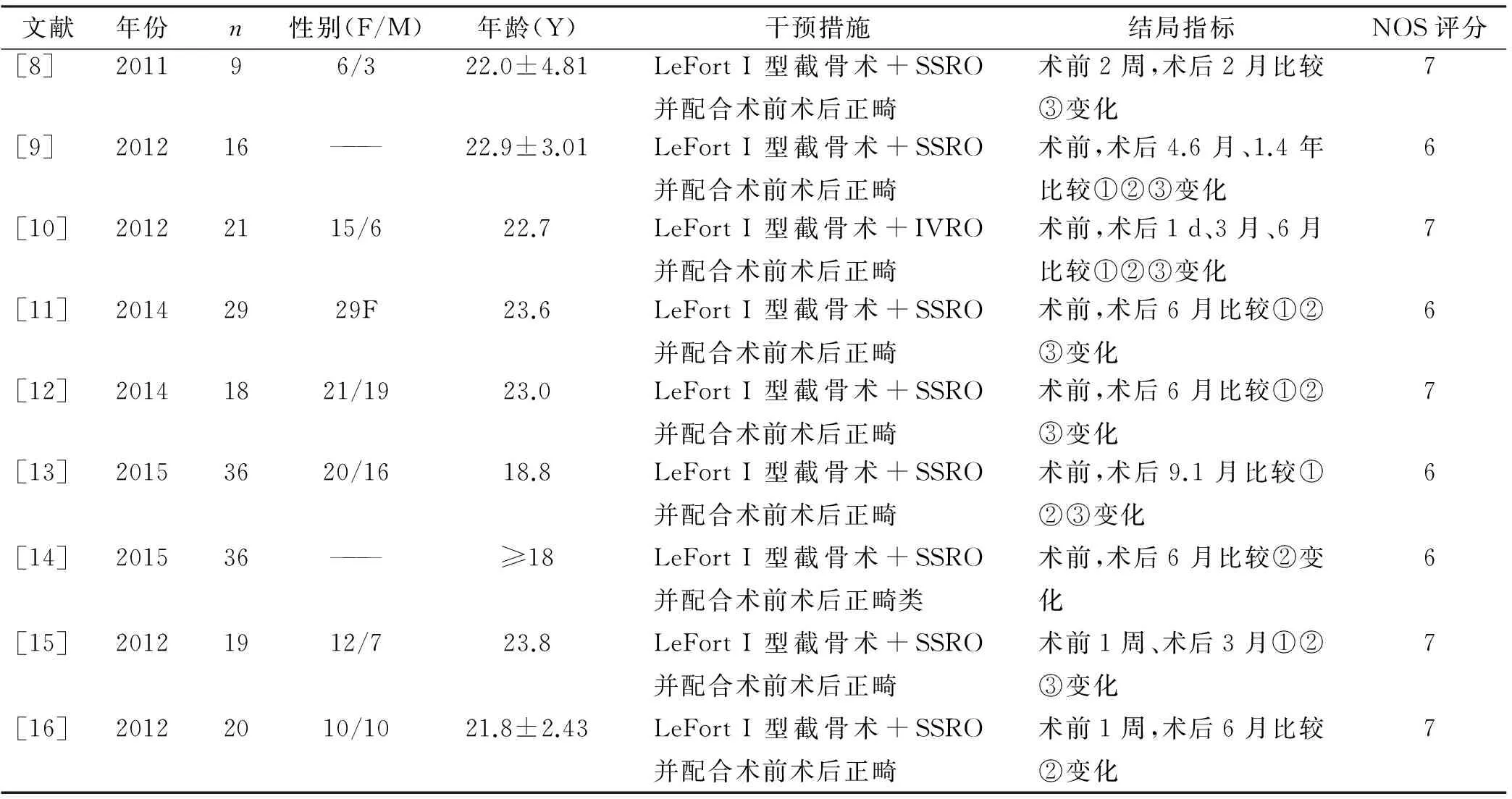
表 1 纳入研究基本特征
注: ——: 文献未提及; SSRO: 下颌矢状劈开术; IVRO: 下颌垂直切开术; ①NPV: 鼻咽体积; ②OPV: 口咽体积; ③TV: 总体积
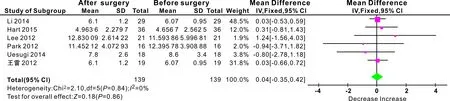
图 1 鼻咽体积变化的Meta分析结果
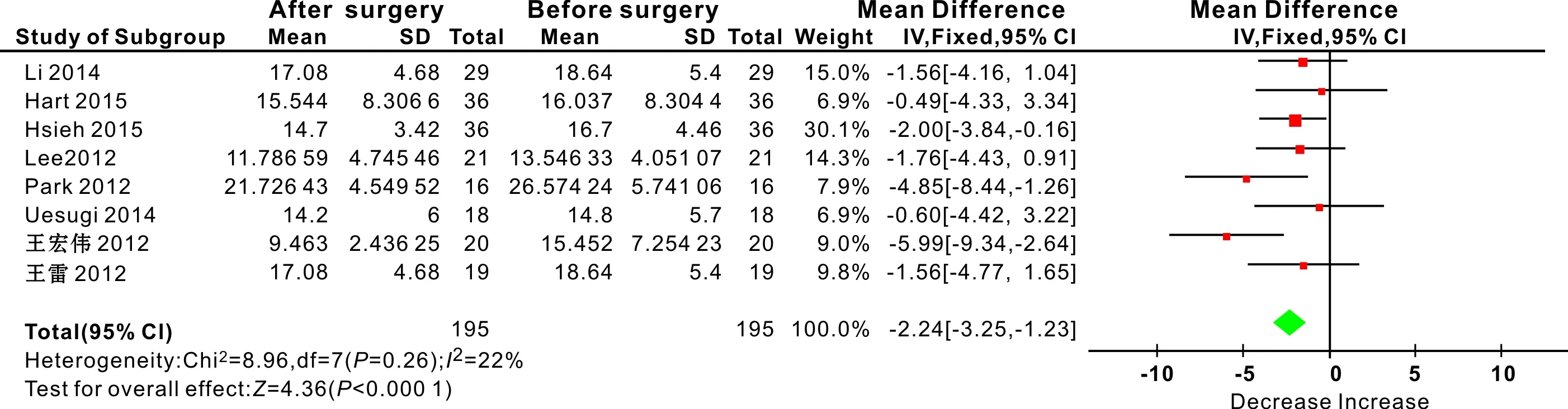
图 2 口咽体积变化的Meta分析结果
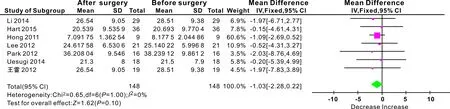
图 3 总体积变化的Meta分析结果
2.4 敏感性分析
Lee[10]报道中,患者采取的术式为LeFort I型截骨术+IVRO,其余各报道中均采用LeFort I型截骨术和SSRO;在Park[9]、Yuh[14]研究中,患者的性别比例文献中未提及,而Li[11]研究中研究对象均为女性,其余各研究均由男女组成。
2.4.1 鼻咽体积变化 排除Lee[10]行敏感性分析,结果显示:鼻咽部体积变化无统计学意义(WMD=0.01 cm3,95%CI[-0.38,0.40]);各研究间同质性好(I2=0,P=0.85)。排除Park[9]、Li[11]行敏感性分析,结果示:鼻咽部体积变化无统计学意义(WMD=0.08 cm3,95%CI[-0.47,0.63]);各研究间同质性好(I2=0,P=0.66)。各项分析结果未见明显改变(表 2)。
2.4.2 口咽体积变化 排除Lee[10]行敏感性分析,结果显示:口咽部体积变化有统计学意义(WMD=-2.32 cm3,95%CI[-3.41,-1.23]);各研究间有轻度异质性(I2=32%,P=0.18)。排除Park[9]、Li[11]、Yuh[14]行敏感性分析,结果示:口咽部体积变化有统计学意义(WMD=-2.17 cm3,95%CI[-3.64,-0.70]);各研究间有轻度异质性(I2=39%,P=0.16)。各项分析结果未见明显改变(表 2)。
2.4.3 总体积变化 排除Lee[10]行敏感性分析,结果显示:总体积的变化无统计学意义(WMD=-1.10 cm3,95%CI[-2.42,0.23]);各研究间同质性好(I2=0,P=0.99)。排除Park[9]、Li[11]行敏感性分析,结果示:总体积的变化无统计学意义(WMD=-0.92 cm3,95%CI[-2.24,0.40]);各研究间同质性好(I2=0,P=0.89)。各项分析结果未见明显改变(表 2)。

表 2 各项敏感性分析
2.5 发表偏倚
各项结局指标的漏斗图如图 4,均未见明显不对称,说明没有明显发表偏倚。
3 讨 论
本研究纳入的文献均采用CBCT作为测量方式,避免了使用侧位片测量时存在的左右影像重叠不清、无法精确定位等缺点,更加准确的定位、减少伪影,实现三维体积的测量[17],更加真实准确的反映气道变化情况。
3.1 正畸-双颌手术对鼻咽体积的影响

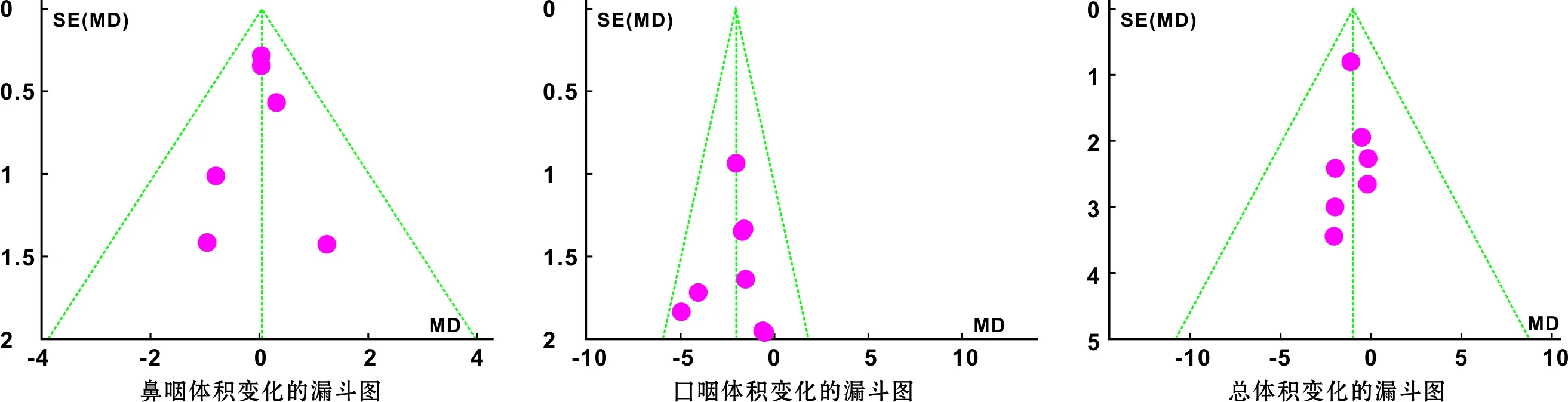
图 4 各结局指标漏斗图分析
3.2 正畸-双颌手术对口咽体积的影响

3.3 正畸-双颌手术对总体积的影响

3.4 本研究的临床意义及局限性

本研究纳入文献数量有限,质量评价均为中等质量,存在一定的风险偏倚;同时本次检索仅限于英文和中文文献,可能会影响资料收集的全面性。除此之外,正颌手术不仅移动上下颌骨,而且与颌骨相关的软腭、舌骨及神经也会随之发生改变,而周围软硬组织的改变也会带来上气道体积的变化,所以观察气道改变的长期性研究也十分必要,本研究只纳入一篇相关文献[9],无法进行Meta分析。今后尚需样本量更多、设计更为完善的高质量研究开展。
[1] Jakobsone G, Neimane L, Krumina G. Two- and three-dimensional evaluation of the upper airway after bimaxillary correction of Class III malocclusion[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2010, 110(2): 234-242.
[3] Degerliyurt K, Ueki K, Hashiba Y, et al. A comparative CT evaluation of pharyngeal airway changes in Class III patients receiving bimaxillary surgery or mandibular setback surgery[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2008, 105(4): 495-502.
[4] Mattos CT, Vilani GNL, Sant' Anna EF, et al. Effects of orthognathic surgery on oropharyngeal airway: A Meta-analysis[J]. Int J Oral Maxillofac Surg, 2011, 40(12): 1347-1356.
[5] Stang A.Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in Meta-analyses[J].Eur J Epidemiol,2010,25(9): 603-605.
[6] Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses[J]. BMJ, 2003, 327(7414): 557-560.
[7] Higgins JP, Seditors G. Cochrane Reviewers' Handbook 5.1.0[OL]. available from http://www.cochrane-handbook.org/
[8] Hong JS, Park YH, Kim YJ, et al. Three-dimensional changes in pharyngeal airway in skeletal class III patients undergoing orthognathic surgery [J]. J Oral Maxillofac Surg, 2011, 69(11): e401-e408.
[9] Park SB, Kim YI, Son WS, et al. Cone-beam computed tomography evaluation of short- and long-term airway change and stability after orthognathic surgery in patients with Class III skeletal deformities: Bimaxillary surgery and mandibular setback surgery[J]. Int J Oral Maxillofac Surg, 2012, 41(1): 87-93.
[10]Lee Y, Chun YS, Kang N, et al. Volumetric changes in the upper airway after bimaxillary surgery for skeletal Class III malocclusions: A case series study using 3-dimensional cone-beam computed tomography[J]. J Oral Maxillofac Surg, 2012, 70(12): 2867-2875.
[11]Li YM, Liu JL, Zhao JL, et al. Morphological changes in the pharyngeal airway of female skeletal Class III patients following bimaxillary surgery: A cone beam computed tomography evaluation[J]. Int J Oral Maxillofac Surg, 2014, 43(7): 862-867.
[12]Uesugi T, Kobayashi T, Hasebe D, et al. Effects of orthognathic surgery on pharyngeal airway and respiratory function during sleep in patients with mandibular prognathism[J]. Int J Oral Maxillofac Surg, 2014, 43(9): 1082-1090.
[13]Hart PS, Mcintyre BP, Kadioglu O, et al. Postsurgical volumetric airway changes in 2-jaw orthognathic surgery patients[J]. Am J Orthod Dentofacial Orthop, 2015, 147(5): 536-546.
[14]Hsieh YJ, Chen YC, Chen YA, et al. Effect of bimaxillary rotational setback surgery on upper airway structure in skeletal Class III deformities[J]. Plast Reconstr Surg, 2015, 135(2): 361e-369e.

[16]王宏伟, 齐素青, 王建国,等. 下颌后退术后舌骨、舌体位置和咽腔间隙变化的锥形束CT分析[J]. 华西口腔医学杂志, 2012, 30(6): 650-654.
[17]Park SH, Yu HS, Kim KD, et al. A proposal for a new analysis of craniofacial morphology by 3-dimensional computed tomography[J]. Am J Orthod Dentofacial Orthop, 2006, 129(5): 600, e23-e34.
[18]高雪梅, 曾祥龙. 鼻咽腔大小对阻塞性睡眠呼吸暂停综合征的影响[J]. 中华耳鼻咽喉头颈外科杂志, 1999, 34(3): 166-169.
[19]Jakobsone G, Stemik A, Espeland L. The effect of maxillary advancement and impaction on the upper airway after bimaxillary surgery to correct Class III malocclusion[J]. Am J Orthod Dentofacial Orthop, 2011, 139(4 Suppl): e369-e376.
[20]Kim H S, Kim G T, Kim S, et al. Three-dimensional evaluation of the pharyngeal airway using cone-beam computed tomography following bimaxillary orthognathic surgery in skeletal Class III patients[J]. Clin Oral Investig, 2016, 20(5): 915-922.
[21]陈科名, 杨崇实, 邓锋. 不同矢状骨面型错殆畸形患者气道大小形态的CBCT研究[J]. 口腔医学研究, 2012, 28(1): 54-57.
[22]Riley R, Guilleminault C, Herran J, et al. Cephalometric analyses and flow-volume loops in obstructive sleep apnea patients[J]. Sleep, 1983, 6(4): 303-311.
[23]Pereira-Filho VA, Castro-Silva LM, de Moraes M, et al. Cephalometric evaluation of pharyngeal airway space changes in Class III patients undergoing orthognathic surgery[J]. J Oral Maxillofac Surg, 2011, 69(11): e409-415.
[24]Wenzel A, Williams S, Ritzau M. Relationships of changes in craniofacial morphology, head posture, and nasopharyngeal airway size following mandibular osteotomy[J]. Am J Orthod Dentofacial Orthop, 1989, 96(2): 138-143.
[25]Ishiguro K, Kobayashi T, Kitamura N, et al. Relationship between severity of sleep-disordered breathing and craniofacial morphology in Japanese male patients[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2009, 107(3): 343-349.
Volumetricchangesintheupperairwayafterorthodontic-orthoganthicsurgeryforthetreatmentofskeletalClassIIImalocclusion:Ameta-analysis
CHENDeyu,GUOWanlu,WANGYurong.
401147,DepartmentofOrthodontics,AfiliatedHospitalofStomatology,ChongqingMedicalUniversity;ChongqingKeyLaboratoryforOralDiseasesandBiomedicalScience,China
Objective: To evaluate volumetric changes in the upper airway after orthodontic-bimaxillary surgery for the treatment of skeletal class III malocclusion.MethodsLiteratures about volumetric changes in the upper airway after orthodontic- bimaxillary surgery for the treatment of skeletal class III malocclusion were searched from the database: Cochrane library, Embase, PubMed, Web of Science, Wangfang, China Science and Technology Journal Database(VIP), Chinese Biomedical Medicine Database(CBM) and China National Knowledge Infrastructure(CNKI). All the literatures were evaluated by Newcastle-Ottawa Scale(NOS) and analyzed by RevMan 5.3.Results9 studies with 204 cases about volumetric changes in the upper airway after orthodontic-bimaxillary surgery for the treatment of skeletal III malocclusion were included. Meta-analysis showed that after treatment there was no statistical difference about the nasopharyngeal volume change and the total volume change(P>0.05); there was statistically significant difference about oropharyngeal volume change(P<0.05).ConclusionIt might be better to consider orthodontic-bimaxillary surgery for skeletal class III malocclusion with certain risk factors about OSAHS, but there was still a risk of airway narrow after orthodontic-bimaxillary surgery for skeletal class III malocclusion.
SkeletalclassIIImalocclusion;Orthodontictreatment;Orthoganthicsurgery;Airway;Meta-analysis
重庆市卫生局重点项目(编号: 2009-1-32)
401147, 重庆医科大学口腔医院正畸科, 口腔疾病与生物医学重庆市重点实验室
王豫蓉 E-mail: 1920779581@qq.com
783.5
A
10.3969/j.issn.1001-3733.2017.04.010
(收稿: 2017-01-25 修回: 2017-06-14)
