自发性颅内出血死亡的多因素回归分析
2017-10-17蔡根平王文浩刘长春
蔡根平,王文浩,胡 康,刘长春,林 洪,张 源
自发性颅内出血死亡的多因素回归分析
蔡根平,王文浩,胡 康,刘长春,林 洪,张 源
目的探讨自发性颅内出血(spontaneous intracerebral hemorrhage, SIH)患者30 d内死亡的危险因素。方法回顾性分析2012-01至2016-01医院收治的SIH患者324例。30 d内死亡82例,为死亡组,其余242例存活患者为存活组,统计分析两组患者入院时主要临床特征。单因素和多因素logistic回归分析显示格拉斯哥昏迷评分降低、糖尿病、小脑出血、出血量增加和脑室出血等死亡的危险因素。结果与存活组比较,死亡组年龄显著偏大[(54.38±12.47)岁vs(51.73±11.94)岁,P=0.028];高血压病显著增加(68.29%vs55.79%,P=0.047),;糖尿病显著增加(46.34%vs27.69%,P=0.002);吸烟率显著增加(35.37%vs21.07%,P=0.009);小脑出血率显著增高(20.73%vs8.68%,P=0.003);脑室出血率显著增高(74.39%vs54.96%,P=0.002);手术率显著降低(20.73%vs37.19%,P=0.006);出血量显著增多[(110.98±36.96)mlvs(77.04±31.81)ml,t=4.922,P=0.000];格拉斯哥昏迷评分显著降低(7.52±2.70vs9.54±2.06,t=4.207,P=0.000)。结论格拉斯哥昏迷评分降低、糖尿病、小脑出血、出血量增加和脑室出血是SIH患者30 d内死亡的危险因素。
自发性颅内出血;死亡;危险因素;多因素回归分析
自发性颅内出血(spontaneous intracerebral hemorrhage, SIH)是一种致死性疾病,30 d内病死率可高达25%[1-3]。近年来,随着高血压、高血脂和糖尿病等慢性病发生率不断增高,SIH的发病率呈上升趋势[4, 5]。80%的SIH为原发性,主要由慢性高血压、颅内动脉瘤导致。出血的部位、出血量、年龄和其他合并症等均可导致SIH不同的临床预后[6]。格拉斯哥昏迷评分、脑出血分级量表等诸多病情严重度评分,在预测患者临床预后方面具有一定的临床意义[7]。然而,不同年龄和合并症等患者,即使格拉斯哥昏迷评分相同,其临床预后可不同。SIH患者发病后30 d内是死亡的高峰期,占病死率的70%以上[8]。因此,分析SIH患者30 d内死亡的危险因素具有十分重要的临床意义。本研究回顾性分析2012-01至2016-01解放军175医院收治的SIH患者324例,对其中82例30 d内死亡患者的相关数据进行总结分析,旨在探讨格拉斯哥昏迷评分降低、糖尿病、小脑出血、出血量增加和脑室出血是SIH患者30 d内死亡的危险因素。
1 对象与方法
1.1 对象 收集我院2012-01至2016-01收治的SIH患者,纳入标准:(1)通过磁共振或CT诊断为SIH;(2)入院距发病时间小于12 h;(3)年龄18~75岁。排除标准:(1)入院时脑干反射消失;(2)肿瘤、创伤、动静脉畸形导致的颅内出血;(3)临床病历资料不全;(4)不配合治疗;(5)住院期间转院;(6)放弃治疗。研究期间,根据纳入标准和排除标准,共收集SIH 324例,其中82例为30 d内死亡,总病死率为25.31%,根据死亡情况,将患者分为死亡组(n=82)和存活组(n=242)。本研究通过我院伦理委员会批准,患者及家属签署知情同意书。
1.2 方法 收集入院后完善相关检验检查,包括年龄、性别、格拉斯哥昏迷评分、高血压、糖尿病、高脂血症、吸烟、嗜酒、出血部位、出血量、脑室出血、蛛网膜下腔出血、手术治疗和30 d内病死率等。格拉斯哥昏迷评分:根据睁眼反应、语言反应和肢体运动对患者进行评分,总分为0~15分,得分越低,昏迷程度越重。分析死亡组患者与存活组患者临床特征差异,同时分析自发性颅内出血患者30 d内死亡的危险因素。
1.3 统计学处理 采用SPSS22.0统计软件进行分析,其中计量资料符合正态分布使用独立样本t检验;计数资料采用χ2检验;危险因素使用单因素logistic和多因素logistic回归分析;P<0.05为差异有统计学意义。
2 结 果
2.1 一般情况 与存活组患者比较,死亡组年龄较大,高血压病、糖尿病、小脑出血、脑室出血率发生率显著增加,差异有统计学意义(表1);手术率显著降低(20.73%vs37.19%,P=0.006)。
表1两组自发性颅内出血患者一般情况比较

(n;%)
2.2 格拉斯哥昏迷评分和出血量比较 死亡组出血量显著多于对照组,差异有统计学意义[(110.98±36.96)mlvs(77.04±31.81)ml,t=4.922,P=0.000];格拉斯哥昏迷评分显著低于对照组(7.52±2.70vs9.54±2.06,t=4.207,P=0.000)。
2.3 危险因素单因素和多因素logistic回归分析 格拉斯哥昏迷评分降低、糖尿病、小脑出血、出血量增加和脑室出血是SIH患者30 d内死亡的危险因素(P<0.05,表2)。
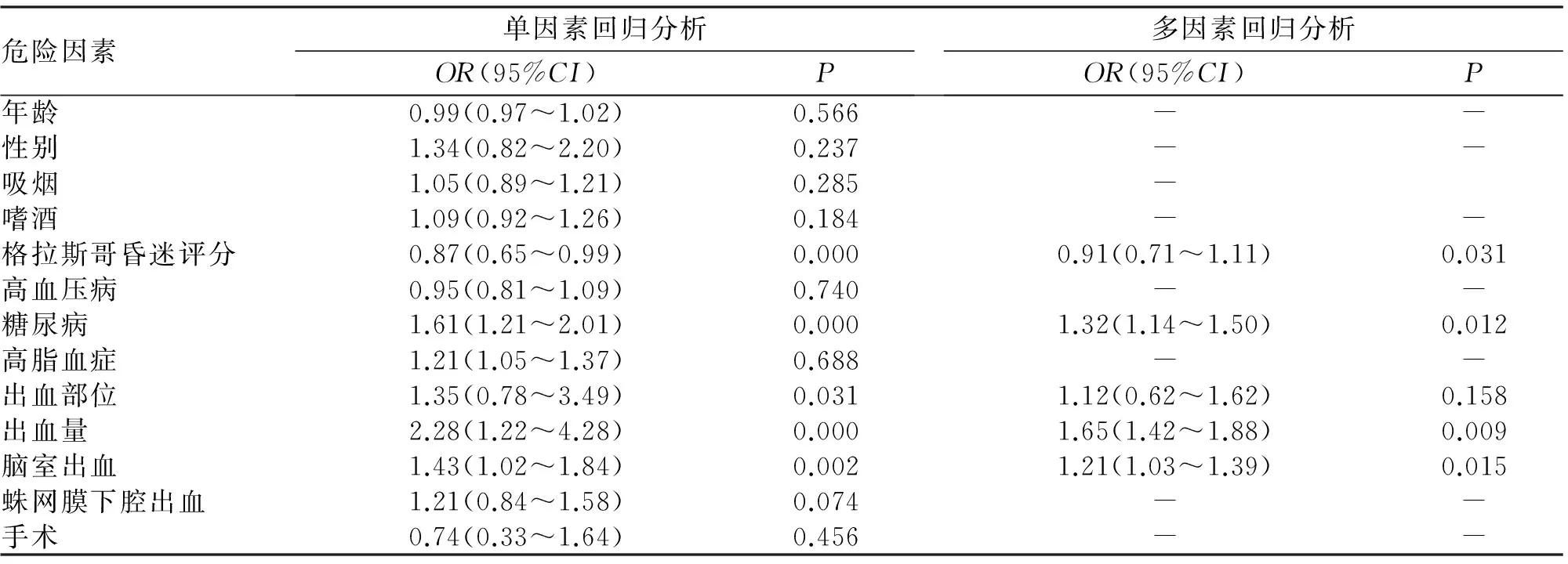
表2 82例自发性颅内出血患者30 d内死亡的危险因素分析
3 讨 论
高血压、高血脂和糖尿病等慢性病可导致发生SIH[9]。由于我国高血压人群基数较大,因此SIH合并高血压病较常见。长期慢性高血压可导致患者脑动脉粥样硬化,导致动脉瘤形成,其中豆纹动脉、桥脑、大脑白质和小脑动脉瘤较为常见,因此出血部位常出血于基底节、脑小叶、小脑和脑干等部位,严重时可合并脑室出血和蛛网膜下腔出血等,具有病情严重、病死率高、好发于中老年的特点。SIH在发病30 d内病死率较高,虽然国内外学者对此进行了深入研究,但其临床病死率仍高居不下[10, 11]。为早期识别重症患者, Bakhshayesh等[12]纳入98例SIH,其研究结果表明年龄、合并长期慢性糖尿病、NIHSS评分增加、出血量增加和周围水肿是SIH死亡的危险因素。Stein等[11]研究发现,脑室出血和脑积水分级可以较好地预测SIH患者的临床预后。本研究显示,与存活者比较,死亡患者年龄、高血压病、糖尿病、吸烟率、小脑出血率、脑室出血率和出血量显著增加,手术率和格拉斯哥昏迷评分显著降低。单因素和多因素logistic回归分析显示格拉斯哥昏迷评分降低、糖尿病、小脑出血、出血量增加和脑室出血是SIH患者30 d内死亡的危险因素。临床上对于格拉斯哥昏迷评分降低、合并糖尿病、小脑出血、脑室出血和大量出血的患者应加强监护,或许有助于降低SIH患者整体病死率。格拉斯哥昏迷评分根据睁眼、语言反应和肢体运动三个大类对颅内病变的患者进行评分,总分为15分,得分降低与颅内病变患者预后不良显著相关,表现为得分越低,病死率越高[13, 14]。因此被临床医师广泛应用,且格拉斯哥昏迷评分系统较为简便,本研究显示其在预测SIH中具有较好的价值。小脑和脑室是颅内重要部位,大量出血导致的占位性病变可导致患者发生脑疝等,进而导致死亡[15]。长期糖尿病与SIH患者颅内动脉粥样硬化有关,合并高血压病可对患者形成双重打击,另外,合并糖尿病的SIH患者感染风险更高,尤其是术后,这可能是糖尿病导致SIH患者预后不良的因素。
综上所述,本研究通过回顾性分析表明,格拉斯哥昏迷评分降低、糖尿病、小脑出血、出血量增加和脑室出血是SIH患者30 d内死亡的危险因素,但仍存在收集病例较少的问题,下一步需加大样本,对临床诊治进行更深入地研究。
[1] Safatli D A, Gunther A, Schlattmann P,etal. Predictors of 30-day mortality in patients with spontaneous primary intracerebral hemorrhage[J]. Surg Neurol Int,2016,7(Suppl 18):S510-517.
[2] Stein M, Hamann G F, Misselwitz B,etal. In-Hospital mortality and complication rates in surgically and conservatively treated patients with spontaneous intracerebral hemorrhage in central europe: a population-based study[J]. World Neurosurg,2016,88(42):306-310.
[3] Ziai W C, Siddiqui A A, Ullman N,etal. Early therapy intensity level (TIL) predicts mortality in spontaneous intracerebral hemorrhage[J]. Neurocrit Care,2015,23(2):188-197.
[4] Liu J, Wang D, Lei C,etal. Etiology, clinical characteristics and prognosis of spontaneous intracerebral hemorrhage in children: a prospective cohort study in China[J]. J Neurol Sci,2015,358(1-2):367-370.
[5] Hemphill J C, Greenberg S M, Anderson C S,etal. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American heart association/American stroke association[J]. Stroke,2015,46(7):2032-2060.
[6] Ferrete A M, Egea J J, Vilches A A,etal. Predictors of mortality and poor functional outcome in severe spontaneous intracerebral hemorrhage: a prospective observational study[J]. Med Intensiva,2015,39(7):422-432.
[7] Wang Q, Lin S, Dong W,etal. Characteristics of etiological diagnostic workup across the past 10 years in patients with spontaneous intracerebral hemorrhage in a large general hospital[J]. Dev Neurorehabil,2016,19(1):10-16.
[8] Gregson B A, Broderick J P, Auer L M,etal. Individual patient data subgroup meta-analysis of surgery for spontaneous supratentorial intracerebral hemorrhage[J]. Stroke,2012,43(6):1496-1504.
[9] 翟卫东,钟建卫,王 涛,等. 高血压脑出血并发大面积脑梗死的危险因素分析[J]. 武警医学,2014,25(5):497-499.
[10] Chan C L, Ting H W, Huang H T. The incidence, hospital expenditure, and, 30 day and 1 year mortality rates of spontaneous intracerebral hemorrhage in Taiwan[J]. J Clin Neurosci,2014,21(1):91-94.
[11] Stein M, Luecke M, Preuss M,etal. The prediction of 30-day mortality and functional outcome in spontaneous intracerebral hemorrhage with secondary ventricular hemorrhage: a score comparison[J]. Acta Neurochir Suppl,2011,112(3):9-11.
[12] Bakhshayesh B, Hosseininezhad M, Seyed Saadat S M,etal. Predicting in-hospital mortality in Iranian patients with spontaneous intracerebral hemorrhage[J]. Iran J Neurol,2014,13(4):231-236.
[13] 王小刚,高 丁,李 涛,等. 院前应用格拉斯哥昏迷分级评分评估颅脑损伤患者与预后的相关性分析[J]. 中国临床医生杂志,2015, 8(1):36-39.
[14] 锁建军. 格拉斯哥昏迷评分和血液流变学变化对外伤继发大面积脑梗死的评估价值[J]. 中国实用神经疾病杂志,2016,19(17):97-98.
[15] Fu J, Chen W J, Wu G Y,etal. Whole-brain 320-detector row dynamic volume CT perfusion detected crossed cerebellar diaschisis after spontaneous intracerebral hemorrhage[J]. Neuroradiology,2015,57(2):179-187.
(2016-12-10收稿 2017-04-11修回)
(责任编辑 郭 青)
Multi-factorregressionanalysisof30-daymortalityinpatientswithspontaneousintracranialhemorrhage
CAI Genping, WANG Wenhao, HU Kang, LIU Changchun, LIN Hong, and ZHANG Yuan.
Department of Neurosurgery, No.175 Hospital of PLA,Zhangzhou 363000, China
ObjectiveTo explore the risk factors of 30-day mortality in patients with spontaneous intracranial hemorrhage (SIH).MethodsThree hundred and twenty-four patients with SIH admitted to our hospital between January 2012 and January 2016 were retrospectively studied. Eight-two patients who died within 30 days were assigned to a death group, while another 242 survivors were assigned to a survival group. The main clinical features of both groups were observed. Univariate and multivariate logistic regression analysis was used to study such risk factors for death as a decrease of Glasgow coma score, diabetes, cerebellar hemorrhage, an increased amount of hemorrhage and intraventricular hemorrhage.ResultsWhen compared with the survival group, patients in the death group had significantly older ages (54.38±12.47vs51.73±11.94,P=0.028), a higher rate of hypertension (68.29%vs55.79%,P=0.047),diabetes (46.34%vs27.69%,P=0.002)and of smoking (35.37%vs21.07%,P=0.009). The rate of cerebellar hemorrhage increased apparently (20.73%vs8.68%,P=0.003), the rate of intraventricular hemorrhage increased significantly (74.39%vs54.96%,P=0.002), the surgical rate decreased (20.73%vs37.19%,P=0.006), the amount of bleeding increased apparently [(110.98±36.96)mlvs(77.04±31.81)ml,t=4.922,P=0.000] and the Glasgow coma score decreased significantly (7.52±2.70vs9.54±2.06,t=4.207,P=0.000).ConclusionsA decrease in Glasgow coma scale, diabetes, cerebellar hemorrhage, an increased amount of hemorrhage and cerebral ventricular hemorrhage are risk factors for 30-day mortality in patients with SIH.
spontaneous intracranial hemorrhage; death; risk factors; multiple regression analysis
R651.1
蔡根平,本科学历,医师。
363000 漳州,解放军第一七五医院神经外科
王文浩,E-mail:1360500900@163.com
