肱骨头骨折块体积与治疗方法的相关性研究
2017-09-11沈施耘王栋梁张炯豪何继业彭建平张家红
沈施耘王栋梁张炯豪何继业彭建平张家红
·论著·
肱骨头骨折块体积与治疗方法的相关性研究
沈施耘1王栋梁2张炯豪3何继业2彭建平2张家红2
目的探讨肱骨头骨折块性质与手术方法、预后之间的相关性,并获得支持手术方法选择的相关参数。方法自2013年1月至2015年12月上海交通大学医学院附属新华医院骨科连续收治的49例肱骨近端四部分骨折患者,最终44例获得随访,其中男21例,女23例,年龄范围:58~89岁,平均(78.09±2.52)岁,其中32例行切开复位内固定术(open reduction and internal fixation,ORIF),12例行半肩关节置换术(hemi-arthroplasty,HA)。术前均行肩关节三维CT重建,分别测量出肱骨头骨折块体积与肱骨头的体积,所得的加权比值拟代表肱骨头骨折块的性质。患者术后功能的评价采用美国肩与肘协会评分系统(American shoulder and elbow surgeons'form,ASES)评分,随访时间12~58个月,平均(29.26±2.58)个月。结果行ORIF的32例患者,术后ASES评分40.0~85.0分,平均(66.78±4.51)分,优良率为68.7%(22例);行HA的12例患者,术后ASES评分18.0~88.0分,平均(61.83±12.34)分,优良率为41.6%(5例)。对肱骨头骨折块性质与肩关节功能的相关性分析显示,ORIF后,两者间存在线性关系(P<0.01),而HA后两者间无明显相关性。结论肱骨头骨折块体积比>54.46%的四部分骨折,ORIF较HA功能恢复更佳。肱骨头骨折块体积比 <54.46%的四部分骨折,尤其是当患者年龄较大伴骨质疏松时,HA预后较好。
肱骨近端粉碎性骨折; 手术方法; 预后; 半肩关节置换术; 锁定钢板
肱骨近端骨折在全身骨折中约占5%[1],其中80%的患者通过非手术治疗可获得较为满意的结果[2]。但对于不稳定的骨折,保守治疗可能导致严重的畸形和肩关节功能障碍[3],具体的手术方式较多,但都具有一定的并发症发生率,其中切开复位内固定术(open reduction internal fixation,ORIF)和半肩关节置换术(hemiarthroplasty,HA)是有效而常用的方法。
目前临床被广泛使用的锁定钢板能较好地固定松质骨骨折块[4],多数患者获得了良好的功能恢复。但对于复杂的肱骨近端骨折,总体治疗效果仍不甚理想[5]。HA一般用于骨质差或粉碎程度严重的老年患者。虽然有报道认为HA术后患者功能的恢复并不十分理想[6],且ORIF相对HA术后短期并发症更少,术后功能更好[7-8]。但也有报道显示HA相较ORIF能获得更好的肩关节活动度[9],而肩袖的完整程度往往起到了重要的作用[10]。
本研究拟探讨通过影像资料来测量肱骨头骨折块体积,评估其与手术方法选择及其预后之间的相关性,并获得支持手术方法选择的相关参数。
资料与方法
一、 一般资料
自2013年1月至2015年12月本院连续收治符合筛选标准的49例肱骨近端四部分骨折患者,5例失联,其中2例拒绝接受随访,3例因与本次手术无关的原因死亡。其余44例中,男21例,女23例,年龄:58~89岁,平均(78.09±2.52)岁。其中32例患者接受ORIF,12例患者接受HA。手术均由2名有丰富肩关节手术经验的副主任以上医师完成。患者于术前常规行患侧肱骨近端正侧位X线片以及肩关节三维重建CT,术后仅复查肩关节X线正侧位片。患者随访时间12~58个月,平均(29.26±2.58)个月。
二、纳入及排除标准
纳入标准:①急性、闭合性肱骨近端粉碎性骨折(根据Neer分类系统四部分骨折);②患者年龄超过18岁;③患者无神经功能损伤。
排除标准:①病理性骨折和开放性骨折;②合并有其他四肢骨折的患者;③肱骨头骨折块关节面不完整。
三、测量与计算方法
1.测量与计算:数据的测量均采用Unisight(3.0)软件进行,为避免个体差异对试验结果的影响,实际测得的肱骨头骨折块体积均加权以消除此差异,所得的加权比值R代表肱骨头骨折块的体积。
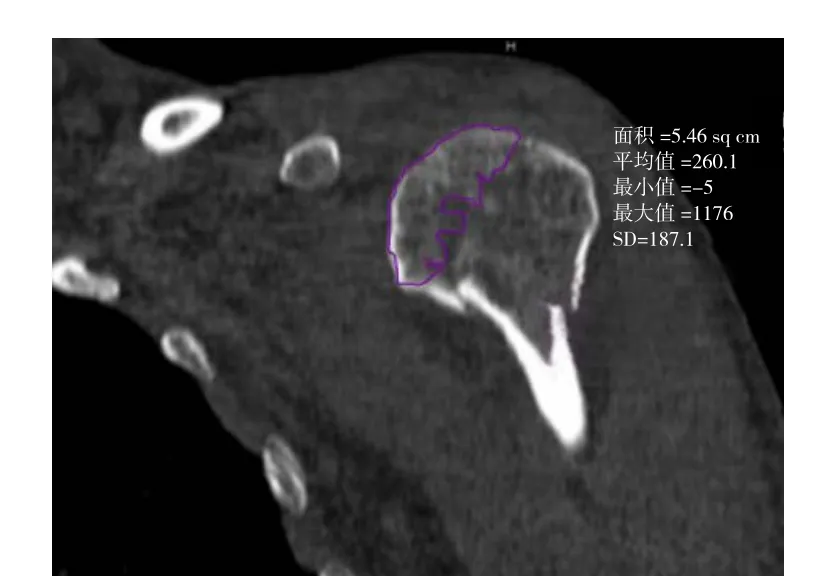
图1 肱骨头骨折块在一个层面上面积的测量
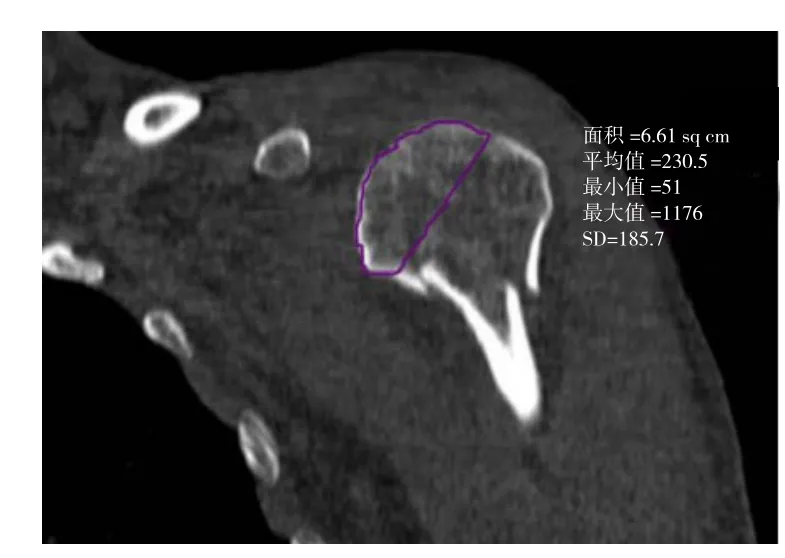
图2 肱骨头标准体积在一个层面上面积的测量
2.体积Vm的测量及加权值R的计算:在三维CT重建图像上(图1~2)选取骨折块截面,软件自动测量选取范围面积Sm,分别测量出肱骨头骨折块各断面面积后,使用微积分法计算出骨折块体积Vm。同时,在各个扫描断面上连接肱骨头关节面两侧边界点以及关节面,用同样的方法计算出完整肱骨头的体积V。

Vm:肱骨头骨折块体积;Sm:骨折块截面面积;V:肱骨头体积;S:肱骨头截面积;H:CT层厚;n:扫描层数。
四、手术方法及术后康复练习
1.ORIF(PHILOS®):均采用全身麻醉,沙滩椅位,标准胸大肌三角肌入路,并使用缝线技术加强固定。术后用前臂吊带悬吊,术后第1天即开始手腕关节和肘关节的主动活动;术后第2天拔除引流管后开始耸肩和钟摆样运动;术后3周增加患肢的被动活动,包括前屈、后伸运动,内收、内旋运动,外展、外旋运动;术后6周X线复查发现明显骨痂形成后可开始肩关节周围肌肉的力量和顺应性锻炼。
2.HA(ZIMMER®):手术体位及入路同ORIF,按照ZIMMER®放置标准操作,术后将肩关节放置于外展45°,旋转中立位,术后即开始患肢肌肉的等长收缩;术后第2天拔除引流管后开始耸肩活动和渐进钟摆样运动;术后3周开始行被动前屈、后伸、内旋、外旋及外展活动(同ORIF组);术后6周行X线检查,发现有结节间骨痂形成后,开始肩关节渐进性主动锻炼,并逐步增加肩关节的活动度;术后12周开始行肩关节牵拉和抗阻力训练,并逐渐增加肩关节周围肌肉群的协调性和顺应性。
五、评价指标
功能评估根据美国肩与肘协会评分系统(American shoulder and elbow surgeons'form,ASES)评分,它由两部分组成:患者的疼痛感觉(50%)和日常功能活动(50%)。满分为100分,0~54分为差,55~69分为中,70~84分为良,85~100分为优。
结 果
一、AESE评分结果
32例行ORIF的患者,ASES评分40.0~85.0分,平均(66.78±4.51)分;12例行HA的患者,术后ASES评分18.0~88.0分,平均(61.83±12.34)分,其中1例(8.3%)为优、4例(33.3%)良好、4例(33.3%)中等、3例(25.0%)较差。
二、统计学分析结果
1. ORIF后患者相关数据的统计学分析:将肱骨头骨折块体积加权值R与肩关节术后ASES评分进行正态检验,P>0.01,表明符合二元正态分布,故可作线性相关与线性回归。使用SAS软件(V9.4)分析发现,加权后肱骨头骨折块的体积与术后ASES评分存在线性关系,P <0.01,可见肱骨头骨折块体积与ORIF肩关节的功能评分间存在线性关系,随后求得线性回归方程 :y=34.60+0.50x,R2=0.82,P <0.01(方程 1)。
2. HA后患者相关数据的统计学分析:将肱骨头骨折块体积加权值与肩关节功能进行正态性检验,P>0.01,表明符合二元正态分布,故可作线性相关与线性回归。使用SAS软件(V9.4)作线性相关分析,肱骨头骨折块体积与术后ASES评分相关性P=0.032,即肱骨头骨折块性质与HA后肩关节的功能之间不存在线性关系,故不可作线性回归分析;但因体积与术后ASES评分符合二元正态分布,故可采用均数61.83±12.35代表其平均值。
三、并发症
ORIF组未发现有内固定失败、神经损伤或深部感染的患者,患者由于锁定钢板位置偏高出现了肩峰下撞击1例,肱骨头缺血性坏死1例,螺钉松动1例,骨折延迟愈合2例(其中1例接受手术,1例最终愈合);HA组未出现假体周围骨折、异位骨化、神经损伤或深部组织感染,出现人工假体关节松动1例,未行翻修手术。
讨 论
手术治疗肱骨近端粉碎性骨折是复杂而具有挑战性的,ORIF和HA是较为成熟而常用的术式。虽经多年的临床实践,手术方法的选择依然存在争议[11],ORIF和HA各具优点的同时,也都存在相当比率的并发症发生率[12]。
锁定钢板的使用克服了许多传统钢板的不足,发散的螺钉对疏松的骨质有更大的把持力,尽可能降低复位丢失的几率。稳定的固定后,患者能早期进行功能锻炼,降低术后关节粘连的发生率,改善了肩关节活动度,从而获得理想的肩关节功能。多位学者的临床试验也都证明,肱骨近端骨折行锁定钢板内固定后可获得比较理想的功能预后[13-16]。
HA较适合骨折粉碎程度严重或存在明显骨质疏松的患者[6],这样的患者往往复位较为困难或内固定后稳定性较差。Popescu等[17]的研究认为大多数患者行HA后,其肩关节功能和活动范围不佳。Bastian等[6]的研究显示,肱骨近端粉碎性骨折术后的功能恢复,HA略差于ORIF,这种差异可能是由于不同的年龄和性别所致。虽然对术后功能的恢复存在争议[18-20],但HA对患者疼痛的缓解却是得到广泛认可的。
尽管已有许多学者对肱骨近端骨折手术方法选择做了相关研究,但肱骨头骨折块的体积与手术方法选择是否有相关性尚未见报道。
随着肱骨头骨折块体积的增加,患者ORIF后ASES功能评分均随之上升,并且经SAS软件计算统计,它们之间存在线性关系,而在HA后的患者中,没有得到存在相关性的依据。
12例行HA的患者,术后ASES评分平均值为(61.83±12.35)分,代入方程1,当y=61.83时,x=54.46,即统计学上,当肱骨头骨块体积大于54.46%时,ORIF会有大于61.83的评分,此时ORIF后肩关节功能较HA后好。故可以认为,这些患者建议选择ORIF,反之则建议选择HA。
行ORIF的患者,若骨折粉碎较严重,特别对于高龄骨质明显疏松患者,易致骨折复位丢失。Spross等[21]报道 PHILOS®钢板难以固定 Neer 4型骨折,他认为钢板不能提供长期的稳定性,容易导致骨折内翻移位。而本研究显示,在四部分骨折患者中,当肱骨头骨折块体积比大于54.46%时,锁定钢板多能提供足够的稳定性,即便出现骨折内翻移位,其肩关节功能仍较HA后为好。
行HA的患者,除假体放置位置外,肩袖的质量对于HA后的功能康复也至关重要[10]。高龄患者接受HA后,尽管能显著缓解疼痛,但功能结果往往并不令人满意。Wild等[22]报道ORIF相对HA,有更为理想的手术效果,并认为如果HA的术后功能不佳,往往与旋转肩袖的完整性、高龄、大小结节的难以解剖复位、软组织过度剥离、假体位置不佳等因素有关。研究结果显示四部分骨折患者肱骨头骨块折体积比小于54.46%时,HA后肩关节功能可优于ORIF。目前,反肩关节置换术在国外大量开展,其手术效果也得到了广泛的肯定,但由于价格昂贵,国内的应用受到了限制,如HA后关节功能差,特别是伴有肩袖功能障碍时,反肩关节置换术可能是唯一的挽救方法[23]。
从术后的并发症上可以看到有1例患者出现肩峰下撞击,这可能是由于钢板放置的位置偏高引起的。1例肱骨头缺血性坏死的患者其肱骨头骨折块的体积较小,而肱骨头血供破坏较为严重,该患者术前肱骨头骨折块完全脱位,应高度怀疑肱骨头血供严重破坏,需进一步考虑HA。1例钢板松动与过早的开始肩关节负荷有关,对这类患者应加强术后随访,增加其顺应性。钢板松动还可能与术中反复调整螺钉位置有关,螺钉位置调整后,原螺钉孔处的骨质强度明显降低。1例假体松动考虑与患者未按要求行康复训练有关。
本研究尚存不足,一是部分患者失访(失访5例);二是行HA的患者总例数仅12例,病例数较少。本研究显示肱骨头骨折块的性质与术后肩关节功能无线性关系,但随着例数的增加不排除存在相关性的可能,此时可取两直线的交点,作为手术方法选择的临界点。研究本身的不足在于它是一个回顾性的研究,所以缺乏随机对照性,一些粉碎严重的肱骨近端骨折或者老年骨质明显疏松的患者多采用了HA而没有行ORIF,相对而言,行ORIF的患者骨折粉碎程度较轻,可能导致ORIF后的功能较实际更好,而HA后的功能较实际更差。
综上所述:①肱骨头骨折块体积比>54.46%的四部分骨折,ORIF较HA功能恢复更佳;②肱骨头骨折块体积比 <54.46%的四部分骨折,尤其是当患者年龄较大伴骨质疏松时,HA预后较好;③本研究拟为肱骨近端粉碎性骨折手术方法的选择提供理论依据。
[1]Palvanen M, Kannus P, Niemi S, et al. Update in the epidemiology of proximal humeral fractures[J]. Clin Orthop Relat Res,2006, 442: 87-92.
[2]Tamimi I, Montesa G, Collado F, et al. Displaced proximal humeral fractures: when is surgery necessary?[J]. Injury,2015, 46(10): 1921-1929.
[3]Hessmann M, Baumgaertel F, Gehling H, et al. Plate fixation of proximal humeral fractures with indirect reduction: surgical technique and results utilizing three shoulder scores[J].Injury, 1999, 30(7): 453-462.
[4]Björkenheim JM, Pajarinen J, Savolainen V. Internal fixation of proximal humeral fractures with a locking compression plate: a retrospective evaluation of 72 patients followed for a minimum of 1 year[J]. Acta Orthop Scand, 2004, 75(6): 741-745.
[5]Parmaksizoğlu AS, Sökücü S, Ozkaya U, et al. Locking plate fixation of three- and four-part proximal humeral fractures [J].Acta Orthop Traumatol Turc, 2010, 44(2): 97-104.
[6]Bastian JD, Hertel R. Osteosynthesis and hemiarthroplasty of fractures of the proximal humerus: Outcomes in a consecutive case series[J]. J Shoulder Elbow Surg, 2009, 18(2): 216-219.
[7]Cvetanovich GL, Chalmers PN, Verma NN, et al. Open reduction internal fixation has fewer short-term complications than shoulder arthroplasty for proximal humeral fractures[J].J Shoulder Elbow Surg, 2016, 25(4): 624-631.
[8]Dai J, Chai Y, Wang C, et al. Meta-analysis comparing locking plate fixation with hemiarthroplasty for complex proximal humeral fractures[J]. Eur J Orthop Surg Traumatol, 2014, 24(3): 305-313.
[9]Cai M, Tao K, Yang C, et al. Internal fixation versus shoulder hemiarthroplasty for displaced 4-part proximal humeral fractures in elderly patients[J]. Orthopedics, 2012, 35(9):e1340-e1346.
[10]Hashiguchi H, Iwashita S, Ohkubo A, et al. The outcome of hemiarthroplasty for proximal humeral fractures is dependent on the status of the rotator cuff [J]. Int Orthop, 2015, 39(6):1115-1119.
[11]Price MC, Horn PL, Latshaw JC. Proximal humerus fractures[J]. Orthop Nurs, 2013, 32(5): 251-258.
[12]Königshausen M, Kübler L, Godry H, et al. Clinical outcome and complications using a polyaxial locking plate in the treatment of displaced proximal humerus fractures. A reliable system?[J]. Injury, 2012, 43(2): 223-231.
[13]Erasmo R, Guerra G, Guerra L. Fractures and fracturedislocations of the proximal humerus: A retrospective analysis of 82 cases treated with the Philos(®) locking plate[J].Injury, 2014, 45(6): S43-S48.
[14]Sun JC, Li YL, Ning GZ, et al. Treatment of three-and four-part proximal humeral fractures with locking proximal humerus plate[J]. Eur J Orthop Surg Traumatol, 2013, 23(6): 699-704.
[15]Panchal K, Jeong JJ, Park SE, et al. Clinical and radiological outcomes of unstable proximal humeral fractures treated with a locking plate and fibular strut allograft[J]. Int Orthop, 2016,40(3): 569-577.
[16]Matejcić A, Vidović D, Ivica M, et al. Internal fixation with locking plate of 3- and 4-part proximal humeral fractures in elderly patients: complications and functional outcome[J].Acta Clin Croat, 2013, 52(1): 17-22.
[17]Popescu D, Fernandez-Valencia JA, Rios MA, et al. Internal fixation of proximal humerus fractures using the T2-proximal humeral nail[J]. Arch Orthop Trauma Surg, 2009, 129(9):1239-1244.
[18]Agarwal S, Rana A, Sharma RK. Functional outcome after primary hemiarthroplasty in three or four part proximal humerus fracture: A short term followup[J]. Indian J Orthop, 2016, 50(6): 590-594.
[19]Leblanc JE, Macdermid JC, Faber KJ, et al. Outcomes after hemiarthroplasty for proximal humerus fracture are significantly affected by hand dominance [J]. J Orthop Trauma, 2015, 29(8): 379-383.
[20]Cuff DJ, Pupello DR, Santoni BG. Partial rotator cuff repair and biceps tenotomy for the treatment of patients with massive cuff tears and retained overhead elevation: midterm outcomes with a minimum 5 years of follow-up[J]. J Shoulder Elbow Surg,2016, 25(11): 1803-1809.
[21]Spross C, Platz A, Erschbamer MA, et al. Surgical treatment of neer group VI proximal humeral fractures retrospective comparison of PHILOS (R) and hemiarthroplasty[J]. Clin Orthop Relat Res, 2012, 470(7): 2035-2042.
[22]Wild JR, Demers A, French R, et al. Functional outcomes for surgically treated 3- and 4-part proximal humerus fractures [J].Orthopedics, 2011, 34(10): e629-e633.
[23]Szerlip BW, Morris BJ, Edwards TB. Reverse shoulder arthroplasty for trauma: when, where, and how[J]. Instr Course Lect, 2016, 65: 171-179.
Study on the correlation between fragment volume and treatment methods of humeral head fractures
Shen Shiyun1, Wang Dongliang2, Zhang Jionghao3, He Jiye2, Peng Jianping2, Zhang Jiahong2.1Shanghai Jiao Tong University School of Medicine, Shanghai 200025,China;2Department of Orthopaedic Surgery, Xinhua Hospital, Shanghai Jiaotong University School of Medicine,Shanghai 200092, China;3Department of Orthopaedic Surgery, Jing'an District Centre Hospital of Shanghai, Shanghai 200040, China
Wang Dongliang, Email: wang02-73@126.com
BackgroundProximal humerus fractures account for approximately 5% of all fractures, and 80% of them can achieve satisfactory results with nonoperative methods. However, the conservative treatment for unstable fractures may lead to severe deformity and shoulder dysfunction. There are multiple specific surgical methods, but complications usually happen. The open reduction and internal fixation (ORIF)and hemiarthroplasty(HA)are two effective strategies that are commonly used.Currently, the widely used locking plate can well stabilize the cancellous bone fragment in clinic, and most of the patients achieve good functional recovery. However, the overall treatment outcome is still not satisfactory for complex proximal humeral fractures. HA is generally used in elderly patients with poor bone quality or severe comminution. Although previous reports showed unsatisfactory functional recovery of patients after HA and fewer short-term complication and better function of ORIF compared to HA, somereport showed that HA achieves better shoulder mobility than ORIF does. More importantly, the integrity of rotator cuff often plays an important role. In this study, the fragment volume of humeral head was measured based on imaging data in order to obtain the parameters that support the selection of surgical methods and to access the correlation in between.Methods(1) General information. From January 2013 to December 2015, 49 patients with comminuted proximal humeral fractures were treated in our hospital. Among them, 5 cases lost contact; 2 cases refused to be followed up; 3 cases died because of reasons unrelated to this operation. 21 males and 23 females comprised the other 44 treated cases, and the ages ranged from 58 to 89 (78.09±2.52) years. Within the treated group, 32 cases
ORIF, and 12 cases received HA. All operations were performed by two associate chief physicians who had sufficient experiences in the shoulder joint surgery. Before the operation, all patients took the routine X-ray film of proximal humerus in anteroposterior lateral views and 3D reconstruction CT. Only the X-ray film of anteroposterior lateral views were taken postoperatively. Patients were followed up for 12-58 (29.26±2.58) months. (2)Inclusive and exclusive criteria. Inclusion criteria:① acute and closed comminuted proximal humeral fractures(according to Neer classification of 4 parts fractures);② over 18 years old;③ no neurological impairment.Exclusive criteria: ① pathological or open fractures;② combined fractures of other limbs;③ incomplete articular surface of humeral head fragments.(3) Methods.① Measurement and calculation: The data were measured with the Unisight 3.0 software. In order to avoid the impact of individual differences on the test result, the actual measurement of humeral head fracture volume was weighted. The weighted ratio R represented the volume of humeral head. ② Calculations of volume Vm and weighted R: The fragment section was selected on 3D reconstruction images, and the corresponding selected area Sm was automatically calculated. The cross - sectional area of humeral head fragment was measured respectively to calculate the fragment volume using calculus. Meanwhile, the articular surface of the humeral head and its boundary points were connected on each scanning section, and the volume V of entire humeral head was calculated using the same strategy. R=Vm/V*100%. Vm= Sm1H+Sm2H+Sm3H+Sm4H+…+SmnH=H∑sm1smn. V=S1H+S2H+S3H+S4H+…+SnH=H∑s1sn. Vm: volume of humeral head fragment;Sm: sectional area of fracture fragment; V: volume of humeral head; S: sectional area of humeral head; H:thickness of CT layer; n: number of scanning layer. (4) Operative methods and postoperative rehabilitation exercises.① ORIF(PHILOS®):All patients were applied with general anesthesia and put in beach chair position. The standard deltopectoral approach was taken, and the suture technique was used to strengthen fixation. The affected arm was suspended postoperatively using forearm sling. The wrist and elbow joint were allowed with active movements starting from the first day after operation; the shrug and pendular exercises were allowed starting from the second day after operation (after the removal of drainage tube) ; the passive movements were introduced 3 weeks after operation, including anteflexion, extension,adduction, abduction, internal rotation and external rotation; the strength and compliance exercises around shoulder muscles started once the obvious callus formation was found under fluoroscopy 6 weeks after operation.② HA (ZIMMER®):The operation position and approach were same as those of ORIF, which were operated based on the ZIMMER®. After the operation, the shoulder joint was placed in rotating neutral position with 45°of abduction. The isometric muscle contraction of affected limb began right after surgery;the shrug and pendular exercises were allowed starting from the second day after operation (after the removal of drainage tube) ; passive anteflexion, extension, adduction, abduction, internal rotation and external rotation were introduced 3 weeks after operation (the same as ORIF group); the gradual active exercises with increasing shoulder joint mobility began once the callus formation between nodules were found under fluoroscopy 6 weeks after operation; the shoulder traction and resistance training were started 12 weeks after surgery, and the coordination and compliance of muscle groups around the shoulder were enhanced gradually.(5) Functional evaluation. The functional evaluation was based on the ASES score,which consisted of two components: the patient's pain perception (50%) and the daily functional activity(50%). The total score was 100 points with 0-55 points for bad, 55-69 points for middle, 70-84 points for good and 85-100 points for excellent.Results(1)AESE scoring results. ① For 32 patients with the treatment of ORIF, the ASES score ranged from 40.0 to 85.0(66.78±4.51)points , and the excellent andgood rate was 68.7%(22 cases); For 12 patients with the treatment of HA, the postoperative ASES score ranged from 18.0 to 88.0(61.83±12.34), and the excellent and good rate was 41.6%(5 cases).(2)Statistical analysis.① Statistical analysis of relevant data of patients after ORIF: The weighted value R of humeral head fragment volume and post-operative ASES scores were analyzed using normal test.P>0.01 suggested the fitness for bivariate normal distribution, which indicated the viability of conducting linear correlation analysis. The analysis with SAS software (V9.4) showed that the weighted volume of humeral head fragment and postoperative ASES scores were in a linear relationship withP<0.01. Furthermore,there was a linear relationship between the humeral head fragment volume and ORIF shoulder joint function scores. The regression equation: y = 34.60 + 0.50 x, R2= 0.82,P<0.01. ② Statistical analysis of relevant data of patients after HA: The weighted value R of humeral head fragment volume and post-operative ASES scores were analyzed using normal test.P>0.01 suggested the fitness for bivariate normal distribution,which indicated the viability of conducting linear correlation analysis. The analysis with SAS software(V9.4) showed the correlation of the weighted volume of humeral head fragment and postoperative ASES scores to beP=0.032 (P>0.01), which meant that there was no liner correlation between humeral head bone quality and shoulder joint function after HA. Thus, it was impossible to conduct linear regression analysis; As the volume and postoperative ASES scores fitted bivariate normal distribution, the average value could be expressed as 61.83±12.35. (3) Complications. No fixation failure, nerve injury or deep infection was found in the ORIF group. Subacromial impingement occurred in one patient due to high position of locking plate. There were 1 case of ischemic necrosis of humeral head, 1 case of screw loosening and 2 cases of delayed union (one received surgery and the other obtained bone union); no periprosthetic fracture, heterotopic ossification, nerve injury or deep tissue infection was found in patients of HA group.One patient had artificial prosthesis loosening and did not receive revision surgery. Conclusion The purpose of this study is to provide a theoretical basis for the selection of surgical methods of proximal humerus comminuted fractures. If the volume ratio of fragment>54.46% for the four-part proximal humeral fracture, good clinical results could be achieved by ORIF. Otherwise, HA would be an ideal treatment for the older patient with osteoporosis.
Comminuted proximal humeral fracture; Surgical methods; Prognosis;Hemiarthroplasty; Locking plate
2017-03-20)
(本文编辑:胡桂英;英文编辑:陈建海、张晓萌、张立佳)
10.3877/cma.j.issn.2095-5790.2017.02.003
上海市科学技术委员会(13DZ1940704)
工作单位: 200025 上海交通大学医学院1;200092 上海交通大学医学院附属新华医院骨科2;200040 上海市静安区中心医院骨科3
王栋梁,Email:wang02_73@126.com
沈施耘,王栋梁,张炯豪,等. 肱骨头骨折块体积与治疗方法的相关性研究[J/CD].中华肩肘外科电子杂志,2017,5(2):90-95.