交锁髓内钉与锁定钢板治疗肱骨近端骨折的临床对比研究
2017-09-11周启荣曹烈虎翁蔚宗陈晓张军汪林王尧苏佳灿
周启荣 曹烈虎 翁蔚宗 陈晓 张军 汪林 王尧 苏佳灿
·论著·
交锁髓内钉与锁定钢板治疗肱骨近端骨折的临床对比研究
周启荣 曹烈虎 翁蔚宗 陈晓 张军 汪林 王尧 苏佳灿
目的探讨交锁髓内钉与锁定钢板治疗肱骨近端骨折的疗效对比。方法将2015年5月至10月第二军医大学附属长海医院创伤骨科收治的51例肱骨近端骨折患者按手术方式分为髓内钉组(n=25)及锁定钢板组(n=26)。记录患者平均手术时间、术中出血量、住院时间、骨折愈合时间、术后并发症的发生情况,采用肩关节Neer评分法和美国肩与肘协会评分系统(American shoulder elbow surgeons'form,ASES)综合评估肩关节功能。结果髓内钉组患者各项手术指标显著优于锁定钢板组(P<0.05)。髓内钉组术后并发症发生率为4.00%,锁定钢板组术后并发症发生率为23.08%,髓内钉组术后并发症发生率低于锁定钢板组。两组患者术后5个月肩关节功能优良率分别为96.00%、88.46%,髓内钉组肩关节功能优良率明显高于锁定钢板组(P<0.05)。结论交锁髓内钉用于治疗肱骨近端骨折,能缩短手术时间、住院时间,减少出血量,在固定骨折稳定性方面与锁定钢板固定相比并没有明显的差异,在手术并发症方面也较锁定钢板固定更具优势,值得临床推广。
肱骨近端骨折; 交锁髓内钉; 锁定钢板
肱骨近端骨折占四肢骨折的5%[1],肱骨近端骨折的发生率每年在105~342/10 000人。在通常情况下,非移位骨折通常采取保守治疗,移位骨折采取手术治疗。在骨质疏松的老年人中,由于致伤能量低,通常导致稳定或微移位的骨折,大多数患者通过保守治疗能够获得肩关节功能的恢复,只有大约20%的患者需要手术治疗。一般认为,头干位移大于50%的干部直径、内翻或外翻角比正常头干倾斜角大20°以上的骨折需考虑手术治疗。手术治疗方法包括经骨缝合固定术、经皮克氏针固定术、带锁髓内钉固定术、钢板螺钉固定术[2]。髓内钉内固定术和锁定钢板内固定术是临床应用较多的手术方法,髓内钉一般适用于移位较小的涉及干骺端或骨干的三、四部分骨折,切开复位钢板内固定术的适应证是包含大小结节或肱骨头移位的二、三、四部分骨折,一般认为切开固定能使骨折块获得更好的解剖复位,但手术并发症的发生率更高。髓内钉创伤小,但固定的稳定性不如锁定钢板。手术方式的选择仍存在较大争议,有研究显示在治疗肱骨近端二部分骨折时,髓内钉明显优于钢板,且并发症的发生率更低[2]。但另有多中心研究显示,两种固定方式经长期随访后,在治疗效果和并发症方面并无明显区别,髓内钉固定术导致医源性肩袖损伤需要肩关节镜治疗的比率更高[3-4]。
所以在肱骨近端骨折的治疗中,仍缺少明确的指南或证据来指导临床治疗,作为一种相对常见的骨折类型,关于其治疗的随机对照研究却很少。一部分原因是由于肱骨近端骨折类型多变,治疗方法多样,使临床随机对照研究很难实施,且各个研究间常缺乏统一的标准和准则,使相互间结果对比异常困难[4-5]。为了给临床治疗肱骨近端骨折提供一定的参考,针对以上问题,本院对2015年5月至10月收治的51例肱骨近端骨折的患者分别进行了锁定钢板内固定和髓内钉固定,并对这两种固定方式进行研究和对比,现将治疗结果报道如下。
资料与方法
一、一般资料
选择2015年5月至10月收治的51例肱骨近端骨折患者进行研究,患者骨折类型按肱骨近端骨折Neer分型分为二部分骨折30例,三部分骨折21例。按手术方式分为髓内钉组和锁定钢板组。髓内钉组患者共25例,其中男12例,女13例;年龄35~67岁,平均(46.46±5.78)岁;锁定钢板组患者共26例,其中男15例,女11例;年龄30~65岁,平均(43.45±6.34)岁。两组患者在年龄、性别及骨折分型上差异无统计学意义(P>0.05)。手术均由接受过专业肩肘外科训练的副主任医师配合主治医师完成。
二、纳入及排除标准
1.纳入标准:(1)年龄大于18岁,无严重合并症;(2)符合Neer骨折分型的二、三部分骨折;(3)无明显血管、神经损伤;(4)在入院后1~4 d接受手术,术后无严重并发症。
2.排除标准:(1)年龄小于18岁;(2)严重的血管神经损伤;(3)严重多发伤;(4)术后出现严重并发症。
三、治疗方法
1.髓内钉组:采用臂丛麻醉或全身麻醉,在肩峰前外侧面做斜行切口,在三角肌的前、中1/3交界处沿肌纤维走形劈开三角肌,保护腋神经,劈开三角肌不能超过肩峰远端5 cm,顺纤维切开肩袖。在扩髓时使用全层缝合保护肩袖免受损害。牵拉复位后,透视下插入导针至适当位置,连续扩髓后,将髓内钉插入骨髓腔,确保钉尾埋入肱骨头的关节面,利用外装设备从前侧拧入近端、远端锁钉。直视下全层缝合修复肩袖。透视确认复位情况和螺钉的位置及长度。术后行早期肩关节功能锻炼。
2.锁定钢板组:采用臂丛麻醉或全身麻醉,胸三角入路暴露近端肱骨,剥离三角肌暴露骨折部位,复位后克氏针临时固定,透视复位确定复位情况后,钢板置于大结节上,临时用克氏针固定,透视确定钢板位置正确,先拧入锁定钉固定肱骨头,1~2枚固定肱骨干,透视确定螺钉在软骨下位置和复位质量,确认复位后,透视下拧入固定螺钉。术后行早期肩关节功能锻炼。
四、评价标准
分别记录两组患者手术指标,包括平均手术时间、术中出血量、住院时间、骨折愈合时间、随访术后并发症的发生情况。
采用美国肩与肘协会评分系统(American shoulder elbow surgeons'form,ASES)综合评估肩关节功能。优:复位满意,骨折无畸形愈合,肩关节外展及肘关节屈伸运动无受限,正常臂力,上肢功能恢复,无疼痛;良:复位满意,骨折无畸形愈合,肩关节主动上举大于140°,正常臂力,肩周偶有轻微疼痛或成角;一般:复位基本满意,关节主动上举大于100°,活动时有疼痛,基本正常臂力;差:复位较差,骨折端移位大于1 cm,成角畸形大于30°,骨折愈合困难,骨不连,内固定松动、断裂,患者疼痛明显而持久,肩肘关节功能活动明显受限。
五、统计学分析
应用SPSS17.0软件进行统计学分析,计量资料采用 x-±s表示,组间比较采用t检验,计数资料采用卡方检验,P <0.05为差异有统计学意义。
结 果
一、手术指标比较
两组患者的平均手术时间、术中出血量、住院时间及骨折愈合时间见表1。髓内钉组患者各项手术指标显著优于锁定钢板组(P <0.05)。
二、术后并发症发生情况比较
术后对两组患者进行随访,随访时间为术后5个月,髓内钉组术后并发症发生率为4.00%,锁定钢板组术后并发症发生率为23.08%,髓内钉组术后并发症发生率低于锁定钢板组,见表2。
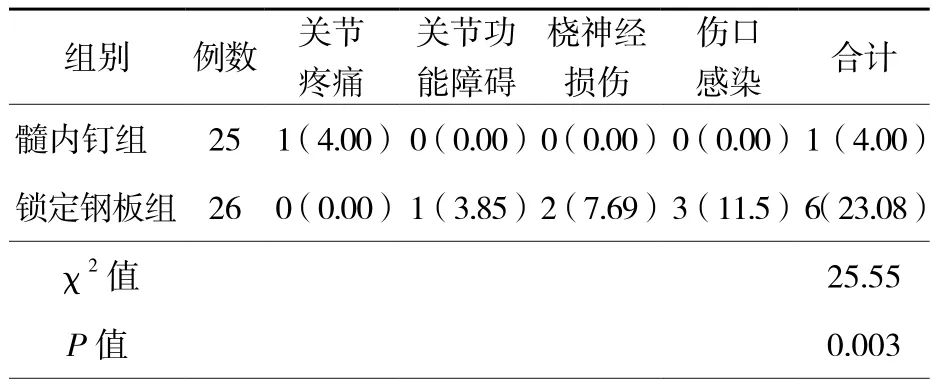
表2 两组患者术后并发症的比较[例(%)]
三、肩关节功能恢复情况比较
两组术后5个月肩关节功能优良率分别为96.00%、88.46%,髓内钉组肩关节功能优良率明显高于锁定钢板组(P <0.05),见表3。
四、影像学观察对比
如图1,从影响学图片中可以看出,髓内钉和锁定钢板对肱骨近端骨折都能进行良好的固定,术后3个月时观察,两种固定方式都实现了良好的愈合。
表1 两组患者手术指标比较(± s)
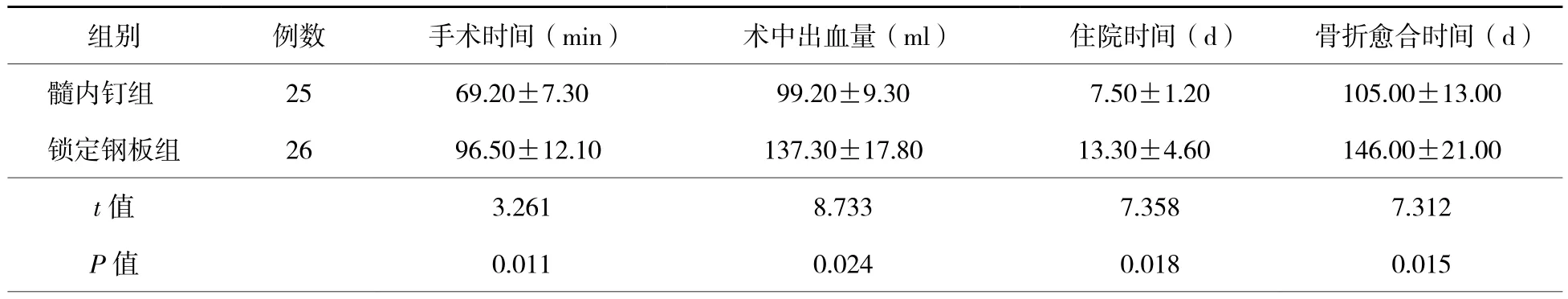
表1 两组患者手术指标比较(± s)
组别 例数 手术时间(min) 术中出血量(ml) 住院时间(d) 骨折愈合时间(d)髓内钉组 25 69.20±7.30 99.20±9.30 7.50±1.20 105.00±13.00锁定钢板组 26 96.50±12.10 137.30±17.80 13.30±4.60 146.00±21.00t值 3.261 8.733 7.358 7.312P值 0.011 0.024 0.018 0.015
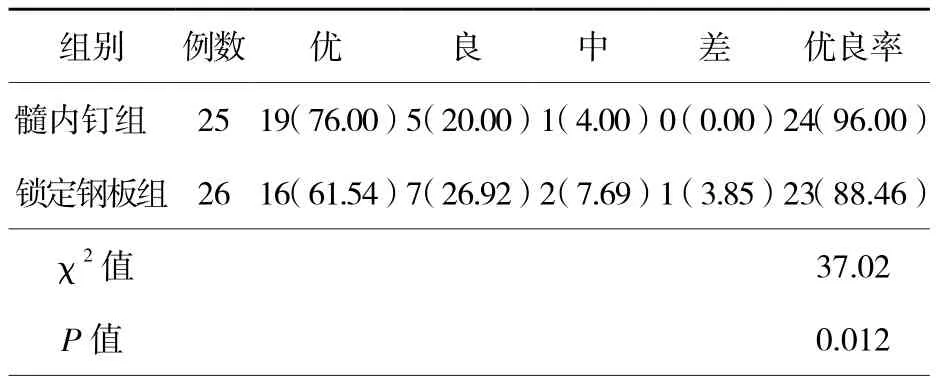
表3 两组患者肩关节功能恢复情况比较[例(%)]

图1 两组患者术前及术后3个月愈合情况对比 图A为髓内钉固定术前;图B为髓内钉固定术后;图C为锁定钢板固定术前;图D为锁定钢板固定术后
讨 论
肱骨近端骨折手术治疗的方法众多,因而要选择恰当的手术治疗方法往往比较困难,临床根据各种情况,应用较多的是切开复位锁定钢板内固定和交锁髓内钉固定,两种固定方法都各有优缺点。切开复位锁定钢板内固定可更好地对骨折块进行操作,因此各种类型的肱骨近端骨折都可用锁定钢板进行固定,由于肱骨头固定较差而导致畸形愈合或不愈合等并发症较多,此外,广泛的软组织剥离增加了肱骨头坏死的可能,并导致肩关节疼痛及功能受限。一个多中心研究显示,在12个月的观察期内,155例患者中,有52例发生了并发症,其中28例是由于拙劣的手术技术造成的[6]。另一项包含154例患者的回顾性分析中描述并发症发生率为48.8%,其中包含了13.8%的正畸率[7]。在本研究中,锁定钢板固定较髓内钉固定出现了更多的并发症,由于放置钢板需更多的暴露和剥离,更长的切口,所以在神经损伤和切口感染方面钢板较髓内钉有更高的发生率。
在固定的稳定性方面仍存在争议,Kitson等[8]进行的尸体研究发现,髓内钉较钢板在外翻、前屈和后伸三个方面稳定性更好;而Sanders[9]学者根据自己的研究结果认为,钢板在外翻负荷下更加坚强,其他的负荷矢量上则无区别。在本研究中,全部病例在5个月的随访观察中,均未出现内固定失效的情况,进一步的固定效果仍需更长时间的观察。
在手术操作过程中肩袖损伤是髓内钉固定时容易出现的问题,会导致术后的肩关节疼痛,影响治疗效果,但髓内钉术后产生的肩关节疼痛比钢板固定严重仍存争议[9]。朱等学者发现,在治疗肱骨近端二部分骨折时,髓内钉在固定骨折方面能提供与钢板相同的稳定性,3年的随访发现,两种固定方式术后的疼痛、肩关节运动并无明显不同,钢板固定术中的失血量更多,髓内钉的术后并发症发生率也更低[10-11]。另一个纳入152例患者的配对多中心研究中,对二、三、四部分骨折的病例分别进行顺行和侧滑稳定的近端交锁髓内钉固定和钢板固定,经过1年的随访后,发现二者的功能评分相同,稳定交锁髓内钉固定术与钢板固定术相比具有相同的并发症发生率,且髓内钉固定术导致医源性肩袖损伤需要肩关节镜治疗的比率更高[12]。在本研究中,髓内钉固定组有1例出现早期肩关节疼痛,随着随访的时间延长,疼痛消失,且两组在肩关节功能评分方面并没有明显的差异。中期回顾中还未发现畸形愈合的病例,证明两种固定方式在固定的稳定性方面并无明显差异,但是髓内钉固定在手术时间、出血量、住院时间方面都具有明显的优势,手术过程中,锁定钉从前侧打入,可避免损伤桡神经,术中所需透视的次数也明显减少,进一步减少手术时间,降低了手术风险。但同时Lundy等[13]学者研究发现,髓内钉置钉点不正确,骨折累及置钉点或延伸至外侧干骺端的复杂骨折,都会影响髓内钉固定的效果。所以,髓内钉固定手术应由经验丰富的外科医师完成,才能真正体现髓内钉治疗的优势,特别是肱骨近端骨折在老年人中发病率最高。在已经步入老龄化社会的中国,如何对此类骨折进行治疗将成为一个重大的社会问题。随着老年骨折患者数量增加和手术技术的改进,更多的微移位骨折选择采取手术治疗,所以对老年患者来说,手术时间的长短、手术创伤、术后并发症将成为手术方式选择的重要方面。
本研究中患者数量少,为回顾性研究,在一定程度上缺少说服力,且为中期随访,更进一步的结果还需进一步随访观察。
综上所述,交锁髓内钉用于治疗肱骨近端骨折,能缩短手术时间、住院时间,减少出血量,在固定骨折稳定性方面与锁定钢板固定相比并没有明显的差异,在手术并发症方面较锁定钢板固定更具优势,特别是在老年骨折的手术处理固定上,将有更广阔的应用,值得临床推广。
[1]Dimai HP, Svedbom A, Fahrleitner-Pammer A, et al. Epidemiology of proximal humeral fractures in Austria between 1989 and 2008[J]. Osteoporos Int, 2013, 24(9): 2413-2421.
[2]Murray IR, Amin AK, White TO, et al. Proximal humeral fractures: current concepts in classification, treatment and outcomes[J]. J Bone Joint Surg Br, 2011, 93(1): 1-11.
[3]Gregory TM, Vandenbussche E, Augereau B. Surgical treatment of three and four-part proximal humeral fractures[J]. Orthop Traumatol Surg Res, 2013, 99(1 Suppl): S197-S207.
[4]Konrad G, Bayer J, Hepp P, et al. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Surgical technique[J]. J Bone Joint Surg Am, 2010, 92(Suppl 1): 85-95.
[5]Burkhart KJ, Dietz SO, Bastian L, et al. The treatment of proximal humeral fracture in adults [J]. Dtsch Arztebl Int,2013, 110(35/36): 591-597.
[6]Horn J, Gueorguiev B, Brianza S, et al. Biomechanical evaluation of two-part surgical neck fractures of the humerus fixed by an angular stable locked intramedullary nail [J]. J Orthop Trauma, 2011, 25(7): 406-413.
[7]Gradl G, Dietze A, Kaeaeb M, et al. Is locking nailing of humeral head fractures superior to locking plate fixation?[J].Clin Orthop Relat Res, 2009, 467(11): 2986-2993.
[8]Kitson J, Booth G, Day R. A biomechanical comparison of locking plate and locking nail implants used for fractures of the proximal humerus [J]. J Shoulder Elbow Surg, 2007, 16(3):362-366.
[9]Sanders R. Re: Percutaneous humeral plating of fractures of the proximal humerus: results of a prospective multicenter clinical trial [J]. J Orthop Trauma, 2010, 24(1): 59.
[10]Maier D, Jaeger M, Izadpanah K, et al. Proximal humeral fracture treatment in adults[J]. J Bone Joint Surg Am, 2014,96(3): 251-261.
[11]Sproul RC, Iyengar JJ, Devcic Z, et al. A systematic review of locking plate fixation of proximal humerus fractures [J].Injury, 2011, 42(4): 408-413.
[12]Zhu Y, Lu Y, Shen J, et al. Locking intramedullary nails and locking plates in the treatment of two-part proximal humeral surgical neck fractures: a prospective randomized trial with a minimum of three years of follow-up[J]. J Bone Joint Surg Am, 2011, 93(2): 159-168.
[13]Lundy DW, Agel J, Marsh JL,et al. Musculoskeletal function assessment outcomes scores over time for tibial plafond (OTA/AO 43) and proximal humeral (OTA/AO 11) fractures: a pilot project[J]. J Orthop Trauma, 2015, 29(2): 60-64.
A clinical research of interlocking intramedullary nail and locking plate in the treatment of proximal humerus fractures
Zhou Qirong, Cao Liehu, Weng Weizong, Chen Xiao, Zhang Jun, Wang Lin,Wang Yao, Su Jiacan. Department of Orthopaedic Surgery, Changhai Hospital, Second Military Medical University, Shanghai 200433, China
Su Jiacan, Email:drsujiacan@163.com
BackgroundProximal humerus fracture accounts for 5% of limb fractures, and the incidence affects 105-342/10 000 people per year. While non-displaced fractures are usually treated conservatively, displaced fractures are treated by surgery. As elderly patients with osteoporosis usually suffer from low energy injury that causes stable or slightly displaced fractures,most of them can obtain the recovery of shoulder joint function with conservative treatment with only about 20% of patients required for surgery. It is generally accepted that surgical treatment should be considered if the displacement of head and shaft is over 50% of shaft diameter, or the angle of varus or valgus is 20° greater than the normal head-shaft angle. Operative treatment methods include transosseous suture fixation, Kirschner wire fixation, intramedullary nail fixation and locking plate fixation. Intramedullary nail fixation and locking plate fixation are more applicable clinically.Intramedullary nailing is indicated for minimally displaced Part-3 and Part-4 fractures that involve humeral metaphyseal or shaft, while open reduction and interal plate fixation is indicated for Part-2,Part-3 and Part-4 fractures that involve greater and lesser tuberosity or humeral head. It is widely accepted that better anatomic reduction can be obtained by open fixation, but the rate of operative complications is higher. Intramedullary nailing is less traumatic, but its fixation stability is inferior to that of locking plate. Thus, the choice of operative methods is still controversial. Studies have shown that intramedullary nailing is superior to plate and has lower complication rate. However,another multicenter study shows that there is no significant difference in curative effect and the incidence of complications between two methods after long-term follow-ups. Intramedullary nail fixation leads to a higher rate of iatrogenic rotator cuff injury which requires further arthroscopic treatment.Therefore, there is still not enough clear guideline or evidence to guide the clinical treatment of proximal humeral fractures. As a relatively common type of fracture, it is seldomly studied by any randomized controlled study. Since the treatment method varies from multiple fracture types, it is difficult to carry out studies. Furthermore, there is no unified standard or guideline for the comparison of results among groups in various studies. In order to provide certain reference for the clinical treatment of proximal humeral fractures, 51 patients were treated with locking plate or intramedullary nail respectively from May to October in 2015 for study and comparison of these two fixation methods.Methods(1)General Information.From May 2015 to October, 51 patients with proximal humeral fractures were treated. According to the Neer classification, 30 cases of Part-2 fracture and 31 cases of Part-3 fracture were included. Patients were divided into two groups based on operative methods. 25 cases belonged to the intramedullary nailing group, including 12 males and 13 females; the age ranged from 35 to 67 years with an average of (46.46±5.78) years. 26 cases belonged to the locking plate group, including 15 males and 11 females; the age ranged from 30 to 65 years with an average of (43.45±6.34) years.There was no statistical difference in age, gender and fracture classification between two groups (P>0.05). The operation was performed by the deputy chief physician trained for professional shoulder and elbow surgery with the cooperation of the attending physician.(2)Inclusive and exclusive criteria.Inclusion criteria: ①age over 18 years without server complication;②Part-2 or Part-3 fracture based on Neer classification; ③ no obvious neurovascular injury; ④ operation performed 1-4 days after admission and no serious postoperative complications.Exclusion criteria:①age less than 18 years;② severe neurovascular injuries; ③ severe multiple injuries; ④ severe postoperative complications.(3)Treatment methods.Intramedullary nail group: after brachial plexus block or general anesthesia, an oblique incision was made on the anterolateral side of acromion. With the protection of axillary nerve, the deltoid muscle was split along muscle fibers at the 1/3 junction of anterior and middle parts of deltoid muscle. The splitting of deltoid muscle should not exceed the distal of acromion for more than 5 cm, and the rotator cuff was cut open along fibers. Full thickness suture was used to protect rotator cuff from damage during medullar cavity reaming. After traction reduction, the guide pin was inserted into the appropriate position of marrow cavity. After continuous reaming, the intramedullary nail was screwed in until the tail has been embedded under the articular surface of humeral head. Then, the proximal and distal locking screws were inserted from the front side with the help of external equipment. The rotator cuff was repaired with full-thickness suture under direct vision. Fluoroscopy was used to confirmed reduction and the position and length of screws. Early shoulder joint function exercises were performed postoperatively. Locking plate group:after brachial plexus block or general anesthesia, the proximal humerus was exposed through deltopectoral approach. The fracture ends were made visible by stripping deltoid muscle, and reduction was temporarily fixed with Kirschner wires. After the reduction condition was confirmed by fluoroscopy, the plate was placed on greater tuberosity and temporarily fixed with Kirschner wires. As the plate position was confirmed properly by fluoroscopy, locking screws were inserted into humeral head for fixation. Afterward, 1-2 screws were for humeral shaft fixation. The position of screws in articular cartilage and the quality of reduction were confirmed under fluoroscopy. In the end, the fixation screws were inserted under fluoroscopy. Early shoulder joint function exercises were performed after surgery. (4)Evaluation criteria.The operation indexes of two groups were recorded, including average operation duration, intraoperative blood loss, hospitalization time,fracture healing time and postoperative complications.American shoulder and elbow surgeons' form(ASES) was used for shoulder joint function evaluation. Excellent : satisfactory reduction, no fracture malunion, no restriction of shoulder abduction and elbow flexion and extension , normal armwrestle, full recovery of upper limb function , no pain; Good: satisfactory reduction, no fracture malunion,>140° of active shoulder elevation , normal arm wrestle, mild pain or slight angulation around shoulder ;Poor: poor reduction,>1 cm of fracture displacement ,>30° of angular deformity , difficulty of fracture healing , nonunion, loosening and breakage of internal fixator, obvious and lasting pain, obviously limited shoulder and elbow movements.(5)Statistical analysis.The SPSS 17.0 software was used for statistical analysis, and the measurement data was expressed as . The t test was used between the groups, and the chi square test was used for enumeration data. The difference was statistically significant ifP<0.05.Results(1)Comparison of operative indexes.The mean operation time, intraoperative blood loss, hospitalization and fracture healing time for the intramedullary nail group were significantly better than those for the locking plate group (P<0.05). (2)Comparison of postoperative complications.The two groups were followed up for 5 months after surgery. The postoperative complication rate of intramedullary nail group was 4.00%, which was lower than that of locking plate group (23.08%). (3) Comparison of shoulder function recovery.The good and excellent rates of shoulder function for two groups 5 months after operation were 96% and 88.46% respectively, and the excellent and good rate of shoulder function for intramedullary nail group was significantly higher than that for locking plate group (P<0.05).(4)Contrast of imaging observation.As what can be seen from images, proximal humeral fractures can be well fixed with both intramedullary nail and locking plate. After 3 months of observation, two fixation methods have both achieved good healing.ConclusionsInterlocking intramedullary nail for the treatment of proximal humeral fractures can shorten the time of operation and hospitalization and reduce blood loss. There is no obvious difference between two strategies in fixing fracture stability.In terms of surgical complications, the interlocking intramedullary nail has more advantages compared to locking plates. Especially in the treatment of senile fracture fixation, the interlocking intramedullary nail has broader applications and is worth of clinical promotion.
Proximal humeral fracture; Intramedullary nail; Locking plate
2016-10-13)
(本文编辑:胡桂英;英文编辑:陈建海、张晓萌、张立佳)
10.3877/cma.j.issn.2095-5790.2017.02.002
国家自然国际合作基金(8141101156);上海市科委生物医药专项(154119500600)
200433 上海,第二军医大学附属长海医院创伤骨科
苏佳灿,Email:drsujiacan@163.com
周启荣,曹烈虎,翁蔚宗,等.交锁髓内钉与锁定钢板治疗肱骨近端骨折的临床对比研究[J/CD].中华肩肘外科电子杂志,2017,5(2):84-89.