锁定钢板联合可吸收软骨钉治疗MasonⅢ型桡骨头骨折
2017-09-11任东邢丹谋冯伟陈焱赵志明王欢肖志宏
任东 邢丹谋 冯伟 陈焱 赵志明 王欢 肖志宏
·论著·
锁定钢板联合可吸收软骨钉治疗MasonⅢ型桡骨头骨折
任东 邢丹谋 冯伟 陈焱 赵志明 王欢 肖志宏
目的评估采用解剖型锁定加压钢板联合可吸收软骨钉治疗MasonⅢ型桡骨头骨折的临床疗效。方法回顾性分析2010年1月至2015年1月武汉市普爱医院收治的MasonⅢ型桡骨头骨折患者19例,其中男7例,女12例;年龄16~58岁,平均38.1岁;左侧8例,右侧11例。其中2例合并肱骨小头软骨损伤,4例合并尺骨冠突骨折,1例合并同侧桡骨远端骨折。根据患者肘关节活动度、肌力、关节稳定性和疼痛情况,按照Broberg-Morrey肘关节评分标准评估。结果所有患者均获随访,随访时间为12~60个月,平均34个月。所有骨折均愈合,平均愈合时间12.4周。Broberg-Morrey评分为64~100分,平均88.4分;其中优6例,良11例,可2例,优良率为89.5%。结论采用解剖型锁定加压钢板联合可吸收软骨钉治疗MasonⅢ型桡骨头骨折,可在重建桡骨头的同时获得良好的关节功能和患者满意度。
桡骨头骨折; 锁定钢板; 可吸收植入物
桡骨头颈部骨折临床较为常见,约占肘部骨折的1/3至1/2,其中约1/3合并有肘部其他损伤,如合并尺骨冠突骨折、肘关节脱位等,则提示损伤更为复杂严重,常常影响到肘关节的稳定性。
复杂的桡骨头骨折的手术方法包括切开复位内固定、桡骨头切除和桡骨头假体置换,但目前对于最佳方式的选择一直存有争议。随着对桡骨头在维持肘关节稳定及传导前臂纵向负荷中重要作用的认识,单纯桡骨头切除已较少采用[1-2]。桡骨小头置换虽大多可获得满意的短期疗效,但亦可能发生关节僵硬、假体松动、肘外翻、骨性关节炎等晚期并发症[3],故仅在无法保留桡骨头时才考虑采用。
随着复位技术和内固定材料的进步,桡骨头颈解剖型锁定钢板和可吸收自身增强软骨钉的应用,使得部分以往认为无法修复的桡骨头得以保留。本文回顾性分析采用解剖型锁定钢板联合可吸收软骨钉治疗MasonⅢ型桡骨头骨折的患者资料,目的是评估解剖型锁定钢板联合可吸收软骨钉治疗MasonⅢ型桡骨头骨折的临床疗效,探讨此种方式的适应证。
资料与方法
一、一般资料
2010年1月至2015年1月武汉市普爱医院收治并采用解剖型锁定钢板(DePuy Synthes公司)联合可吸收软骨钉(成都迪康公司)内固定治疗的粉碎性桡骨头骨折患者19例,其中男7例,女12例;年龄16~58岁,平均38.1岁;左侧8例,右侧11例。致伤原因中:平地摔伤14例,高处坠落伤5例。其中2例合并肱骨小头骨软骨损伤,4例合并尺骨冠突骨折,1例合并同侧桡骨远端骨折。受伤至手术时间3~18 d。所有患者术前均行肘关节正侧位X线片及CT三维重建检查(图1)。

图1 患者男,28岁,术前X线片及CT诊断为左侧MasonⅢ型桡骨头骨折 图A为术前肘关节正侧位片; 图B为术前CT三维重建图像

图2 术中复位及固定情况 图A为桡骨头关节面复位后用可吸收软骨钉固定,克氏针临时固定桡骨颈;图B为解剖型锁定加压钢板固定桡骨颈
二、手术方法
手术在臂丛麻醉、气囊止血带下进行,采用肘外后侧Kocher切口,在肘肌和尺侧腕伸肌之间进入,切开环状韧带和部分旋后肌,暴露桡骨头颈部。显露过程中注意保持前臂旋前位,使桡神经远离术野以避免伤及。术中小心保留附着于骨片上的骨膜,先将碎裂的桡骨头盘状关节面复位,用2~3枚直径2.0 mm可吸收软骨钉固定,钉尾埋于关节面下(图2A)。再将颈部复位,用解剖型锁定钢板固定(图2B)。有多枚骨片游离的桡骨头骨折,可采用“on-table”技术[4],将骨块取出,在手术桌面上拼接,用可吸收软骨钉固定成完整的桡骨头,再用锁定钢板将其与颈部固定。对于合并Ⅱ型尺骨冠突骨折患者,可在显露桡骨头颈时,将桡骨近端向外侧脱位,即可显露尺骨冠突骨折端,先将其复位用微型螺钉或克氏针固定,再固定桡骨头骨折。手术可在一个切口内完成。对于合并肱骨小头软骨骨折患者,采用“线锚钉”方法固定[5-6],即在软骨缺损的两侧边缘预钻孔并导入缝线,将软骨片复位后收紧缝线并打结以固定软骨片。
三、术后处理
术后伤肢行功能位长臂石膏托固定,1周后去除石膏行支具保护下的肘关节屈伸及前臂旋转训练,训练以主动活动为主、被动活动为辅,禁止暴力扳拉。4周后拆除支具开始行抗阻力训练,12周后开始行负重练习。
术后第1天开始口服塞来昔布胶囊200 mg,2次/d,连服4周,镇痛同时可预防异位骨化的发生。
四、功能评价
根据患者肘关节活动度、肌力、关节稳定性和疼痛情况,按照Broberg-Morrey肘关节评分[7]标准进行评分,其中屈伸活动度27分,旋转活动度13分,肌力20分,稳定性5分,疼痛35分,满分100分,95~100分为优,80~94分为良,60~79分为可,60分以下为差。
结 果
本组19例患者切口均一期愈合,无一发生感染及内固定失效。2例术后出现桡神经损伤症状,术后4周内完全恢复,考虑为术中牵拉所致。
术后随访12~60个月,平均34个月,骨折均获得骨性愈合,愈合时间8~20周,平均12.4周,未发现有桡骨头缺血坏死。
患者肘关节屈伸活动度80~140°(平均 120.8°), 旋 转 活 动 度60~150°( 平 均112.4°)。所有患者未出现关节不稳定。遗留肘部疼痛者6例,其中轻度4例,中度2例;肘部或腕部轻度无力者5例,其余患者肌力正常。Broberg-Morrey评分为64~100分,平均88.4分;其中优7例,良13例,可3例,优良率为86.9%。
3例患者术后于肘前侧及外侧出现异位骨化(图3),2例功能为良,1例为可,分别于术后1~2年取内固定同时行异位骨切除和关节松解(图4),第2次术后3个月评分为优(图5)。1例患者因骨折线累及“安全区”,术中为求更好固定效果,将钢板部分放置于安全区内侧,术后随访前臂旋后50°,旋前10°,功能为可,但因其肩关节外展可代偿部分前臂旋前动作,患者并未感觉不便。1例合并同侧桡骨远端骨折患者,术后早期因惧痛拒绝行功能训练,术后6个月时功能为可。

图3 内固定术后23个月,可见肘前异位骨化

图4 术后23个月,行内固定取出及异位骨化切除
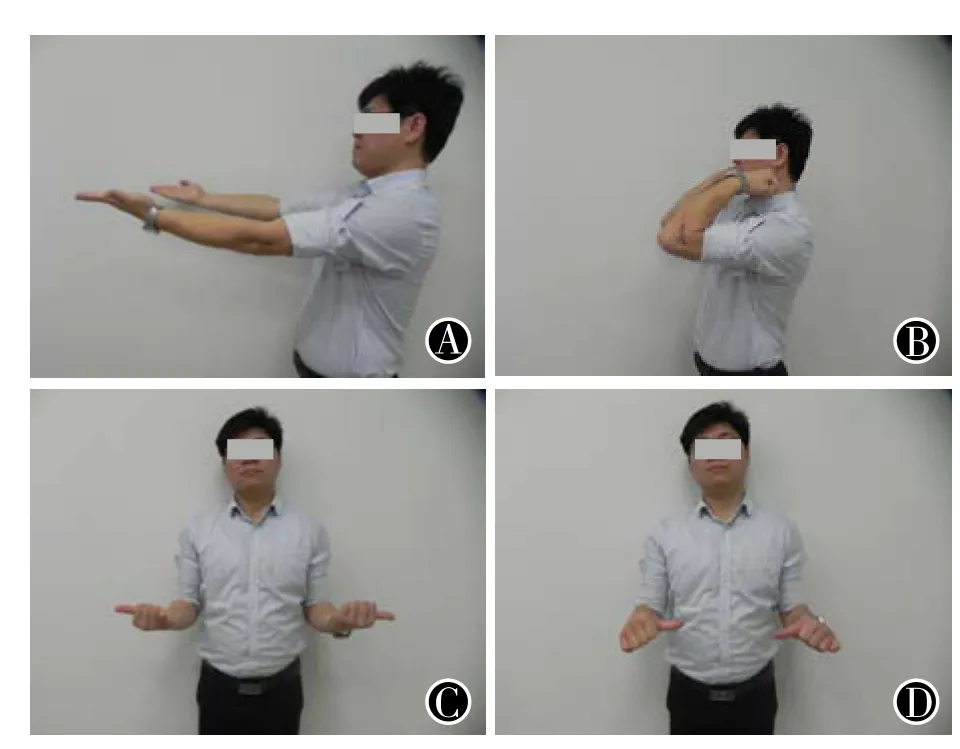
图5 第2次术后18个月,左肘功能情况 图A为伸肘;图B为屈肘;图C为旋后;图D为旋前
讨 论
桡骨头骨折的治疗目的是重建桡骨头的解剖结构,恢复肘关节的外侧稳定性。对于MasonⅠ、Ⅱ型骨折的治疗,学界观点基本一致,即根据骨折移位情况决定行保守治疗或内固定术[8],但对MasonⅢ、Ⅳ型骨折的治疗,目前仍存争议。因较多桡骨小头切除后发生的肘关节外翻不稳定,桡骨上移及继发性下尺桡关节脱位,肘、腕部疼痛无力等并发症,现已很少推荐采用。人工假体置换因手术操作简单,中、短期疗效好,现已得到较广泛应用,但尚缺乏长期随访的资料,且仍有部分患者出现假体松动、关节僵硬、骨性关节炎等并发症。桡骨头骨折大部分发生于青壮年(本组患者平均年龄38.1岁),部分患者观念上不愿接受假体置换。
以往由于内固定材料的限制,很多MasonⅢ型桡骨头骨折内固定效果不尽人意,部分学者认为内固定手术效果差于假体置换[9-10]。但随着解剖型锁定钢板和微型可吸收钉的应用,使得大部分曾经认为不可重建的桡骨头骨折得以保留。可吸收钉初始强度、弹性模量与皮质骨相当,可满足桡骨头骨折块的固定要求,且无需担心普通微型螺钉退钉的风险。桡骨头颈解剖型锁定加压钢板在固定原理上与其他锁定加压钢板类似,钢板与螺钉之间的角稳定性可降低骨折复位丢失的风险,钢板桡骨头部的3枚锁定钉孔设计为分散型,以增加对骨块的把持力,减少术后松动的发生;同时该型接骨板进行了预塑形,外形与桡骨头颈的正常解剖结构一致,有助于骨折复位;且钢板边角部位做了低切迹处理,可减少旋转活动时对环状韧带的刺激。部分患者若术后发生异位骨化影响关节功能,可在骨折愈合后内固定取出的同时行关节松解和异位骨切除,本组3例发生异位骨化患者在第2次术后关节功能得到进一步改善。
解剖型锁定加压钢板使用过程中需注意尽量将钢板置于桡骨头的安全区内,即前臂中立位时,桡骨茎突和Liser结节之间所对应的区域[11]。但对部分严重粉碎的骨折为使其达到更稳定的固定,钢板无法完全放置于安全区时,可将其置于桡骨头前内侧,如术后可能会影响前臂旋前,肩关节外展可部分代偿之。本组病例中有1例发生这种情况,术后前臂旋前活动受限,但患者自觉功能障碍并不明显。
对MasonⅢ型桡骨头骨折采用解剖型锁定加压钢板联合可吸收软骨钉治疗可在重建桡骨头的同时获得良好的关节功能和患者满意度,提供了一种有益的治疗选择,值得临床推广。
[1]Ikeda M, Sugiyama K, Kang C, et al. Comminuted fractures of the radial head. Comparison of resection and internal fixation[J]. J Bone Joint Surg Am, 2005, 87(1): 76-84.
[2]危蕾, 邢丹谋, 何文平, 等. 不同手术方法治疗MasonⅢ, Ⅳ型桡骨头骨折的疗效分析[J]. 中华创伤骨科杂志, 2010,12(6):530-533.
[3]Stuffmann E, Baratz ME. Radial head implant arthroplasty[J].J Hand Surg Am, 2009, 34(4): 745-754.
[4]Businger A, Ruedi TP, Sommer C. On-table reconstruction of comminuted fractures of the radial head[J]. Injury, 2010, 41(6): 583-588.
[5]邢丹谋, 勘武生, 任东, 等. 可吸收自身增强软骨钉治疗桡骨小头骨折[J]. 中华骨科杂志, 2013, 33(1):50-54.
[6]任东, 邢丹谋, 冯伟, 等. 桡骨头骨折伴肱骨小头软骨损伤的治疗[J]. 中华手外科杂志, 2014, 30(5):375-377.
[7]Broberg MA, Morrey BF.Resultsof delayed excision of the radial head after fracture[J]. J Bone Joint Surg Am, 1986, 68(5): 669-674.
[8]郝有亮, 周方, 侯国进. 桡骨头骨折的治疗研究进展[J/CD]. 中华肩肘外科电子杂志, 2016, 4(3):186-190.
[9]Ring D. Displaced, unstable fractures of the radial head: fixation vs. replacement--what is the evidence?[J]. Injury, 2008, 39(12): 1329-1337.
[10]范存义, 姜佩珠, 蔡培华, 等. 内固定与假体置换治疗MasonⅢ型桡骨头骨折的比较研究[J]. 中华创伤骨科杂志,2006, 8(12):1105-1108.
[11]Caputo AE, Mazzocca AD, Santoro VM. The nonarticulating portion of the radial head: Anatomic and clinical correlations for internal fixation[J]. J Hand Surg Am, 1998, 23(6):1082-1090.
Anatomical LCP combined with absorbable cartilage tack in treatment of MasonⅢradial head fractures
Ren Dong, Xing Danmou, Feng Wei, Chen Yan, Zhao Zhiming, Wang Huan, Xiao Zhihong. Department of Hand Surgery, Wuhan Puai Hospital, Wuhan 430033, China
Xing Danmou,Email:13986058526@163.com
BackgroundThe radial head fracture is a common elbow fracture in clinic,accounting for approximately 1/3 to 1/2 of all elbow fractures. Furthermore, about 1/3 of radial head fractures were companied by other elbow injuries such as coronoid process fracture,elbow joint dislocation, etc. These complications suggest more severe and complex damages that often affect the stability of elbow joint. Surgical treatments for complex radial head fractures include open reduction and internal fixation, radial head resection, and radial head prosthesis replacement. However, the choice of the best method remains controversial. With the understanding of the important role radial head plays in maintaining the stability of elbow joint and the longitudinal load of forearm, the simple radial head resection has been seldomly used.The short-term effect of radial head replacement is satisfactory in most cases. However, later complications such as joint stiffness, prosthetic loosening, valgus elbow joint, osteoarthritis,etc. may occur as well. Thus, it is only used when the radial head cannot be preserved.With the development of reduction techniques and internal fixation materials and the application of radial head neck anatomical locking plates and absorbable self-enhancing cartilage tacks, some of the radial head that was used to be regarded as irreparable is preserved.In this study, the data of anatomical locking plate combined with absorbable cartilage tack in the treatment of Mason type III radial head fractures were analyzed to assess the clinical curative effect and to explore its indications.Methods(1)General data.From January 2010 to January 2015,19 patients (7 males and 12 females) with comminuted radial head fractures were treated with anatomic locking plate (DePuySynthes company) and absorbable cartilage tack (Chengdu DUCAM company).The age ranged from 16 to 58 years with an average of 38.1 years. 8 cases had the left side affected, and 11 cases had the right side affected. Causes of injury: 14 cases of flat fall and 5 cases of high fall. The complications included 2 cases of combined injury of humeral cartilage, 4 cases of combined fracture of ulna coronoid process and 1 case of combined fracture of ipsilateral distal radius. The time of injury to surgery ranged from 3 to 18 days. All patients were examined by X-ray and CT three-dimensional reconstruction of elbow joint.(2)Operative methods.The operation was performed under brachial plexus block and pneumatic tourniquets. A posterior lateral Kocher incision was made between anconeus and cubitalis posterior, and the annular ligament and part of musculi supinator were cut open to expose radial head and neck. Attention was paid to maintain the pronation of forearm in order to keep the radial nerve away from the surgical field, which helped to prevent injury. The periosteum attached to bone was carefully retained intraoperatively. The fractured articular disc of radial head was reduced and fixed with 2-3 absorbable cartilage tacks of 2.0 mm in diameter, and the tail was buried under the articular surface. Then, the neck was reduced and fixed with the anatomical locking plate. The “On-table”technique could be used for the radial head fracture with dissociation of several fragments. The fracture fragments were taken out and stitched into a complete radial head on the surgical table followed by fixation with absorbable cartilage screws.Later, the stitched complex and neck were fixed with the locking plate. For patients with the type II fracture of ulna coronoid process, the proximal radius was dislocated laterally during the exposure of radial head to expose the fracture end of ulnar coronoid process. The fracture was reduced and fixed firstly with micro screws or Kirschner wires, and then the radial head fracture was fixed. For patients with the fracture of capitelum cartilage of humerus, the “suture anchor” method was adopted for fixation. To be specific, both sides of the cartilage defect edge were pre-drilled and penetrated with sutures.After being reduced, the cartilage slices were fixed by the tightening and knotting of sutures. (3)Postoperative treatment. The injured limb was fixed with long arm plaster cast after the operation.As the plaster was removed 1 week after the surgery, the flexion and extension training of elbow joint and the rotation training of forearm were carried out. The training was mainly based on active activities and supplemented by passive activities. Violent pulling was forbidden. The brace was removed 4 weeks after the operation, and the resistance training was initiated. The weightbearing exercise began 12 weeks later.On the first day after the operation, oral Celecoxib of 200 mg was taken twice per day for 4 weeks, which could help with analgesia and prevent heterotopic ossification simultaneously.(4)Functional evaluation. The conditions of elbow mobility, muscle strength, joint stability and pain were scored based on the Broberg-Morrey functional scoring criteria. The total score is 100 points, including 27 points for flexion and extension, 13 points for rotation mobility, 20 points for muscle strength, 5 points for stability and 35 points for pain. 95-100 points were considered as excellent; 80-94 points were considered as good; 60-79 points were considered as moderate; 60 points below were considered as poor.ResultsThe incision of 19 cases of this group obtained primary healing without any infection or interal fixator failure. Two cases had the symptom of radial nerve injury and recovered completely within 4 weeks. The injury was considered to be caused by intraoperative traction. The patients were followed up for 12-60 months with an average of 34 months. All fractures were healed by 8-20 weeks with an average of 12.4 weeks. No radial head necrosis was found. The flexion and extension mobility of elbow joint ranged from 80 to 140° (120.8°on average), and the rotation mobility ranged from 60 to 150° (112.4°on average). No joint instability occurred in patients. Six cases had residual pain of elbow, including 4 cases of mild pain and 2 cases of moderate pain. Five cases had mild weakness of elbow or wrist, and the rest of patients had normal muscle strength. The patients had an average Broberg-Morrey score of 88.4 points (64-100 points), which included 7 cases of excellent, 13 cases of good and 3 cases of moderate. The good and excellent rate was 86.9%. 3 patients had heterotopic ossification in the anterior and lateral elbow, including 2 cases of goodand 1 case of moderate. The removal of internal fixation and procedures of ectopic bone resection and arthrolysis were preformed respectively 1-2 years after the initial operation. The score was excellent 3 months after the second operation. Since the “security zone” was affected by the fracture line in 1 patient, the plate was partially placed on the medial side for better fixation effect. During the postsurgical follow-up, the function was good with 50° of pronation and 10° of supination. However, the patient felt no inconvenience as shoulder abduction could compensate for part of forearm pronation.ConclusionThe treatment of Mason type III radial head fracture using anatomical locking compression plate combined with absorbable cartilage tack achieves good joint function, patient satisfaction and radial head reconstruction. Thus, this strategy provides a beneficial treatment option and is worth of clinical promotion.
Radial head fracture; Locking plate; Absorbable implant
2017-02-02)
(本文编辑:胡桂英;英文编辑:陈建海、张晓萌、张立佳)
10.3877/cma.j.issn.2095-5790.2017.02.006
430033 武汉市普爱医院手外科
邢丹谋,Email:13986058526@163.com
任东,邢丹谋,冯伟,等.锁定钢板联合可吸收软骨钉治疗MasonⅢ型桡骨头骨折[J/CD]..中华肩肘外科电子杂志 ,2017,5(2):108-112.