钬激光技术治疗后尿道瓣膜疾病的疗效观察
2017-09-02威力江赛买提帕洛克迪力木拉提迪亚尔地里木拉提阿衣丁西热亚孜旦王玉杰
李 佳 威力江·赛买提 帕洛克·迪力木拉提 迪亚尔·地里木拉提阿衣丁·西热亚孜旦 王玉杰
钬激光技术治疗后尿道瓣膜疾病的疗效观察
李 佳 威力江·赛买提 帕洛克·迪力木拉提 迪亚尔·地里木拉提阿衣丁·西热亚孜旦 王玉杰
目的探讨钬激光治疗后尿道瓣膜疾病的疗效,总结临床经验,推广钬激光在后尿道瓣膜疾病中的应用。 方法 29例后尿道瓣膜症患者,均为男性,行膀胱尿道造影、静脉尿路造影、经尿道输尿管镜检查诊断。均采用全麻,取膀胱截石位,运用钬激光电视监视下将后尿道瓣膜逐个点烧灼切除,再次检查后尿道,后尿道通畅,撤镜。挤压耻骨上膀胱体表处,见冲水样尿液从尿道流出,尿线较前明显增粗。术后给予抗炎、补液及对症处理。留置导尿管2 d~1周不等,并留置膀胱造瘘管。 结果
行钬激光后尿道瓣膜切除术,术中诊断后尿道瓣膜类型均为I型,手术几乎无出血,手术时间短,操作方便。术后随访3个月至2年,24例行经尿道膀胱输尿管镜钬激光手术治疗1次后,排尿费力症状缓解,延缓上尿路扩张损害。表现为:双肾积水改善,B超随访双肾及输尿管扩张情况均不同程度好转,残余尿均较小,术后半年随访尿流率,最大尿流率、平均尿流率均明显高于术前,排尿时间较术前明显缩短。5例症状无改善,行二次钬激光后尿道瓣膜切除术,术后尿流率在7~18 mL/s范围。本组病例术后尿动力学检查结果示:29例中,16例(占94.1%)存在不同程度膀胱功能损害,尿动力学检查表现为顺应性降低,逼尿肌不稳定(占37.9%),10例(占34.5%)残余尿增多。 结论 经尿道钬激光治疗后尿道瓣膜是一种安全、微创、有效治疗后尿道瓣膜的手段,值得推广。
尿道梗阻;激光手术;麻醉;治疗结果
后尿道瓣膜症是男童先天性下尿路梗阻的最常见病因,也是儿童终末期肾病的常见原因,早期发现并切除瓣膜可显著提高患儿生存率,也可以避免日后上尿路的手术修复。经尿道钬激光治疗尿道瓣膜是该病的主要治疗方法。本院2006年12月至2014年6月收治新生儿后尿道瓣膜患儿共29例,采用经尿道钬激光治疗并随访观察治疗效果,现报告如下。
资料与方法
一、一般资料
本研究29例后尿道瓣膜症患者,均为男性,平均年龄为4.7岁,其共同临床表现为排尿费力、尿不成线、尿滴沥等,手术前尿流率在1~9 mL/s范围。其中5例上尿路扩张积水,无膀胱输尿管反流,静脉尿路造影未见明显上尿路梗阻情况;10例单侧膀胱输尿管反流I-IV级;11例双侧膀胱输尿管反流IV-V级别;3例无上尿路积水,膀胱未见明显受损,无小梁小室形成。尿道瓣膜症诊断方法:行膀胱尿道造影、静脉尿路造影、经尿道输尿管镜检查、尿动力学检测。
二、治疗方法
所有患儿入院后均留置导尿管,同时给予抗感染和支持治疗。患儿肾功能好转,水电解质失衡纠正后进行手术治疗。术前平均住院时间9 d。造影检查仍不能明确诊断的患儿,尿道镜检查和手术同步进行。均采用全麻,取膀胱截石位。用手术采12F或8F小儿肾镜。经尿道口置入尿道。尿道内注入适量丁卡因胶浆。明确诊断并了解膀胱和输尿管开口情况。如诊断明确,确定瓣膜位置,厚度及与精阜关系。钬激光输出功率为10~15 W,能量1J,频率10~15 Hz,贴进瓣膜,电视监视下将后尿道瓣膜12点,对10点,2点,7点,5点,逐个点烧灼切除,最后是4点部位的残余瓣膜组织处理,所以残余的游离漂浮瓣膜组织无需处理,再次检查后尿道,后尿道通畅,撤镜。膀胱内注入0.9%氯化钠溶液适量,挤压耻骨上膀胱体表处,见冲水样尿液从尿道流出,尿线较前明显增粗。留置导尿管。术后给予抗炎、补液及对症处理。留置导尿管2 d至1周不等,并留置膀胱造瘘管。新生儿后尿道瓣膜往往较厚,肾镜进镜时阻力较大,即选择退镜至瓣膜远端,用钬激光将精卓及尿道12点处瓣膜切平,手术结束后按压膀胱,可见尿液流出通畅。
三、随访时间及内容
本研究所有患儿通过门诊随访,随访时间为3个月至2年。随访复查排泄期造影、泌尿系B超、尿动力学检测。
四、统计学处理
结 果
行钬激光后尿道瓣膜切除术,术中诊断后尿道瓣膜类型均为I型,手术几乎无出血,手术时间短,操作方便。术毕留置导尿,膀胱造瘘。3周后间断夹毕膀胱造瘘管,排尿通畅后,拔除膀胱造瘘管。随访3个月至2年,24例行经尿道膀胱输尿管镜钬激光手术治疗1次后,排尿费力症状缓解,延缓上尿路扩张损害。表现为:双肾积水改善,B超随访双肾及输尿管扩张情况均不同程度好转,残余尿均较小,术后半年随访尿流率,最大尿流率、平均尿流率均明显高于术前,排尿时间较术前明显缩短,见表1,差异经统计学分析有意义(P<0.05),5例症状无改善,行二次钬激光后尿道瓣膜切除术,术后尿流率在7~18 mL/s范围。本组术后尿动力学检查结果示:29例中,16例(占94.1%)存在不同程度膀胱功能损害,尿动力学检查表现为顺应性降低,逼尿肌不稳定(占37.9%),10例(占34.5%)残余尿增多。
表1 治疗前后尿流率检测结果比较(±s)Table 1 Comparison of urinary flow rate in patients before and after operation(±s)
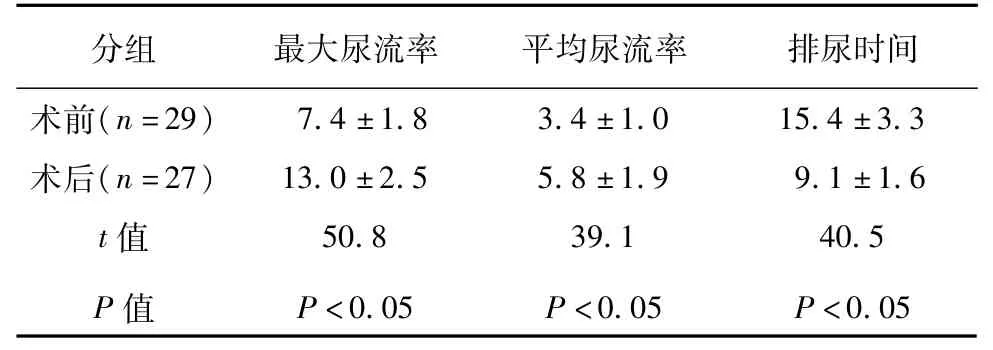
表1 治疗前后尿流率检测结果比较(±s)Table 1 Comparison of urinary flow rate in patients before and after operation(±s)
分组 最大尿流率 平均尿流率 排尿时间术前(n=2 9) 7.4 ± 1.8 3.4 ± 1.0 1 5.4 ± 3.3术后(n=2 7) 1 3.0 ± 2.5 5.8 ± 1.9 9.1 ± 1.6 t值 5 0.8 3 9.1 4 0.5 P值 P<0.0 5 P<0.0 5 P<0.0 5
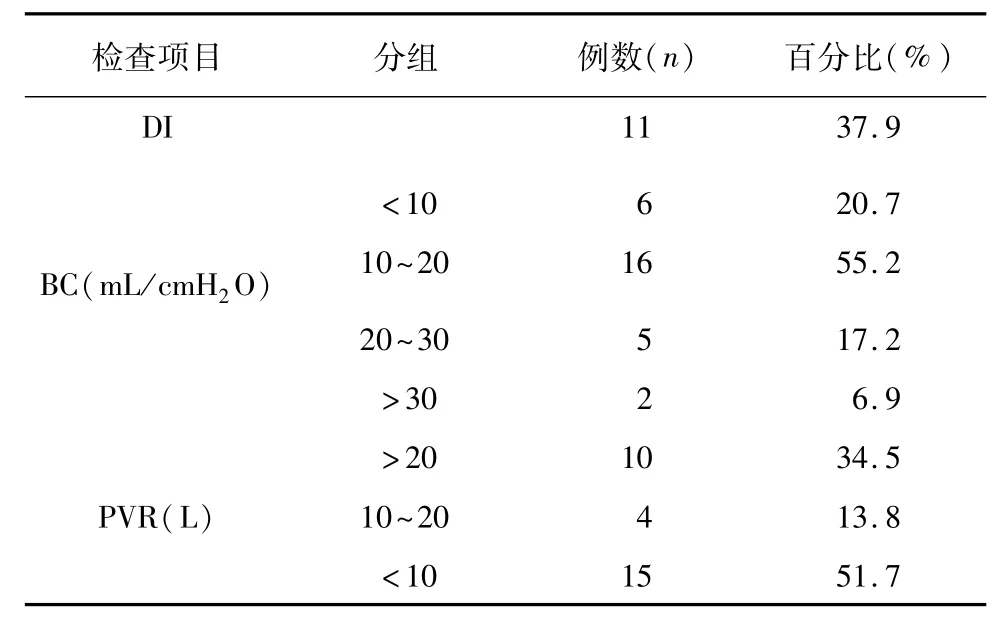
表2 术后尿动力学检查结果Table 2 Postoperative results of urodynamic examinations
讨 论
后尿道瓣膜可导致严重下尿路梗阻和继发性上尿路功能损害,未能及时治疗患儿在青春期前就会出现不可逆转的肾功能衰竭。随着国内超声技术的发展,约65%的后尿道梗阻可以通过产前超声检查发现,而且这一比例还在上升[1-2,12]。
后尿道瓣膜症患儿的临床表现与年龄和梗阻程度相关。新生儿患者的典型表现为双肾积水,膀胱扩张,后尿道扩张和膀胱壁增厚。患儿生后即出现排尿费力,尿滴沥和急性尿潴留。由于肾积水和膀胱输尿管反流导致的泌尿系感染和水电解质紊乱也较常见,排泄性膀胱尿道造影可以诊断,对于有明显下尿路梗阻症状以及产前检查发现双肾积水和输尿管扩张患儿均应施行。典型病例可发现后尿道扩张延长,造影剂中断或突然变细。由于新生儿不合作,针对部分VCUG仍不能明确诊断的患儿,应进一步行尿道镜检查[3-6]。
本组29例全部为YoungⅠ型。它占引起梗阻瓣膜的95%。是一对瓣膜象大三角帆样,起自精阜,远端走向前外侧瓣膜部尿道的近侧缘,双侧在中线汇合,仅留一孔隙,可逆行插入导尿管,但排尿时,瓣膜膨大突人膜部尿道,甚至可达球部尿道,导致梗阻。瓣膜组织结构为单一膜性组织。诸多研究者认为其属中肾管发育不正常,进入泄殖腔比正常位置靠前形成了后尿道瓣膜Ⅰ型。
术后尿动力结果提示,后尿道瓣膜患儿解除梗阻后膀胱功能损害仍然存在,尿动力学改变主要为顺应性、最大逼尿肌收缩压降低,逼尿肌不稳定发生率、残余尿量升高,需术后密切随访[7-10]。
激光的运用在小儿尿道疾病有明显的优势,钬激光是一种高能固体激光,近年来在腔内泌尿外科领域有了广泛的使用,钬激光切后尿道瓣膜有出血少,损伤临近组织少,具有精确切割、凝固止血、汽化组织的优势,国内外有个例报道钬激光治疗输尿管、尿道狭窄、瓣膜的案例,手术效果良好[13-16]。目前小儿后尿道瓣膜的最广泛的治疗是运用小儿电切镜电切治疗,治疗方法包括尿道扩张、经会阴瓣膜切除、冷刀内切开术及电切术等。尿道扩张仅适用于Ⅲ型,效果不佳,且极易复发;经会阴瓣膜切除术创伤大,并发症较多;冷刀内切开术相对安全,但不具备止血功能,切开瓣膜组织时出血对术野影响较大,操作存在一定的盲目性,易伤及海绵体,且无法切除瓣膜,复发率高;电切术可彻底切除瓣膜组织,是目前治疗该病的首选术式,但热损伤较大,易导致新的瘢痕形成,且患儿尿道内径小,儿童电切镜尚不普及,成人电切镜外鞘较粗(常用20 F以上),强行进入可能引起尿道黏膜损伤,造成远期全段尿道狭窄[11-14]。但因基层地区小儿电切镜较少,临床实现较为困难,钬激光相比电切镜治疗后尿道瓣膜优势是出血少视野清晰,操作方便,临床方便,钬激光较电切镜有较高尿道热损伤导致的尿道狭窄,因此术中需避免盲目暴力操作,建议视野清晰操作,本研究运用钬激光治疗小儿后尿道瓣膜治疗效果理想,并为增加术后尿道狭窄,尿失禁等并发症,可临床给予推广,为基层治疗小儿后尿道瓣膜给予更多方向。
经尿道钬激光治疗后尿道瓣膜是一种安全、微创、有效治疗后尿道瓣膜的手段,值得推广。患儿肾功能均可恢复到正常水平,但在部分患者肾积水和膀胱输尿管反流持续存在,治疗后膀胱功能损害仍然存在,需要密切随访和肾功能检查。
1 K.A.R.Hutton.Management of posterior urethral valves[J].Current Paediatrics,2004,14(7):568—575.DOI:10.1016/j.cupe.2004.07.013.
2 Sudarsanan B,Nasir AA,Puzhankara R,et al.Posterior urethral valves:a single center experience over 7 years[J].Pediatr Surg Int,2009,25(3):283—287.DOI:10.1007/s00383—009—2332—z.
3 Caione P,Nappo SG.Posterior urethral valves:long-term outcome[J].Pediatr Surg Int,2011,27(10):1027—1035. DOI:10.1007/s00383—011—2946—9.
4 黄澄如,张维平,孙宁,等.后尿道瓣膜症[J].中华小儿外科杂志,2005,26(1):30—33.DOI:10.3760/cma.j. issn.0253—3006.2005.01.008. Huang CR,ZhangWP,Sun N,etal.Posterior urethral valves in children:Analysis of158 cases[J].Chin JPediatr Surg,2005,26(1):30—33.DOI:10.3760/cma.j.issn.0253—3006.2005.01.008.
5 FarhatW,McLorie G,Capolicchio G,etal.Merguerian.Outcomes of primary valve ablation versus urinary tract diversion in patientswith posterior urethral valves[J].Urology.2000,Vol.56(No.4):653—657.DOI:10.1016/S0090—4295(00)00784—6.
6 梁海燕,张潍平,孙宁,等.小儿后尿道瓣膜切除后合并排尿异常的尿动力学研究[J].中华小儿外科杂志,2014(9):683—686.DOI:10.3760/cma.j.issn.0253—3006. 2014.09.011. Liao HY,Zhang WP,Sun N,et al.Effects of abnormalmicturition in boys with posterior urethral valves after valve ablation[J].Chin JPediatr Surg,2014(9):683—686.DOI:10.3760/cma.j.issn.0253—3006.2014.09.011.
7 苟丽,李泸平,樊玉霞,等.经内镜电灼术治疗小儿后尿道瓣膜症[J].中华小儿外科杂志,2011,32(7):527—529.DOI:10.3760/cma.j.issn.0253—3006.2011.07.013. Gou L,Li LP,Fan YX,et al.Clinical analysis of endoscopic fulguration of posterior urethral valve in children[J].Chin J Pediatr Surg,2011,32(7):527—529.DOI:10.3760/cma. j.issn.0253—3006.2011.07.013.
8 李源,文建国,王庆伟,等.瓣膜膀胱综合征尿动力学研究[J].中华小儿外科杂志,2005(4):192—194.DOI:10. 3760/cma.j.issn.0253—3006.2005.04.008. Li Y,Wen JG,Wang QW,et al.Urodynamics of valve bladder syndrome[J].Chin J Pediatr Surg,2005(4):192—194.DOI:10.3760/cma.j.issn.0253—3006.2005.04.008.
9 孙福涛,张文同,李爱武,等.钬激光在治疗小儿尿道狭窄中的应用[J].临床小儿外科杂志,2005,4(4):274—276. Li FT,ZhangWT,Li AW,et al.Application of holmium laser to treat the urethral stricture in children[J].JClin Ped Sur,2005,4(4):274—276.
10 胡岩,齐灿,李明磊,等.经尿道膀胱镜钬激光治疗小儿尿道瓣膜症[J].中国微创外科杂志,2016,16(8):716—719.DOI:10.3969/j.issn.1009—6604.2016.08.011. Hu Y,Qi C,Li ML,et al.Transurethral cystoscopic holmium laser in the treatment of pediatric urethral valve disease[J].Chin JMin Inv Surg,2016,16(8):716—719.DOI:10.39 69/j.issn.1009—6604.2016.08.011.
11 韩刚,张军勇,杨斌,等,经尿道输尿管镜下2μm激光汽化切除术治疗小儿后尿道瓣膜症[J].解放军医学院学报,2015,36(11):1096—1098.DOI:10.3969/j.issn. 2095—5227.2015.11.010. Han G,Zhang JY,Yang B,et al.Transurethral 2μm laser vaporesection for treatment of posterior urethral valves by ureteroscopy in pediatrics[J].Acad JChin PLA Med Sch,2015,36(11):1096—1098.DOI:10.3969/j.issn.2095—5227.2015.11.010.
12 王晓曼,贾立群,刘青林.超声在小儿后尿道瓣膜诊断中的应用[J].中国超声医学杂志,2014,30(10):927—930. Huang XM,Jia LQ,Liu QL.Utilizing ultrasound in the diagnosis of pediatric posterior urethral valve[J].2014,30(10):927—930.
13 王文举,范应中,李浩,等.小儿后尿道瓣膜的早期诊断与临床治疗分析[J].河南医学研究,2014,23(2):80—82.DOI:10.3969/j.issn.1004—437X2014.02.036. Wang WJ,Fan YZ,Li H,et al.Early diagnosis and clinical treatment of pediatric posterior urethral valves[J].Henan Medical Research,2014,23(2):80—82.DOI:10.3969/j. issn.1004—437X2014.02.036.
14 邱颖,谢向辉,孙宁,等.后尿道瓣膜切除术后尿动力学研究[J].临床小儿外科杂志,2010,9(5).330—333. DOI:10.3969/j.issn.1671—6353.2010.05.004. Qiu Y,Xie XH,Sun N,et al.Bladder dysfunction in boys with posterior urethral valves after valve ablation[J].Clin JPed Sur,2010,9(5).330—333.DOI:10.3969/j.issn. 1671—6353.2010.05.004.
Holm ium laser treatment of posterior urethral valve disease.
.Li Jia,Wilijia Caimaiti,Paruh Dilmurat,Diar Dilmurat,Aidin Xieryazidan,Wang Yujie.Department of Pediatric Surgery,First Affiliated Hospital,Xinjiang Medical University,Wulumuqi830054,China Corresponding author:Wang Yujie,Email:493879845@qq.com
ObjectiveTo explore the efficacy of holmium laser for posterior urethral valve disease. M ethods A total of 29 cases of posterior urethral valve disease were diagnosed by cystoscopy,intravenous urography and transurethral ureteroscopy.After general anesthesia,a position of lithotomy was adopted.Transurethral insertion of a 12F or 8F pediatric kidney endoscope was attempted.If the diagnosiswas definite,valve position,thickness and its relationship with caruncle was determined.Holmium laser was employed formonitoring posterior urethral valve.Posterior urethra was unobstructed and removed.After squeezing the surface of suprapubic bladder,water sample was visible,urine oozed out of urethra and urinary line became thicker than before.Indwelling catheter,anti-inflammation,fluid replacement and symptomatic treatment were performed postoperatively.The duration of indwelling catheter was 2 days to 1 week.Bladder fistula was reserved. Results After transurethral resection,the type of posterior urethral valve was Young I.Operation had minimal bleeding and a short operative duration.At week 3 after indwelling catheterization,urinary bladder fistula was removed.During the follow-up period of 3~24 months,24 patients underwent transurethral ureteroscopic holmium laser surgery once and their symptoms of micturition became alleviated and dilatation of upper urinary tractwas delayed.There was improvement of hydronephrosis.Ultrasonic follow-ups of double kidney and urethral dilatation improved to differentextents and residual urinewas lower after6months.Urine flow rate,maximal flow rate and average urinary flow rate were significantly higher than preoperative values and voiding time significantly shortened.No symptomatic improvement was found in 5 cases.Urethral resection was performedafter two sessions of holmium laser.The postoperative urinary flow ratewas7~18mL/s.The results of postoperative urodynamic examination indicated that16/29 cases(94.1%)had varying degrees of bladder dysfunction and lowered compliance of detrusor instability(37.9%).And 10 cases(34.5%)had increased residual urine.Conclusion Transurethral Holmium laser treatment is safe,mini-invasive and effective for posterior urethral valve disease.And its wider popularization is recommended.
Urethral Obstruction;Laser Surgery;Anesthesia;Treatment Outcome
2017—01—17)
(本文编辑:王爱莲 仇 君)
10. 3969/j.issn.1671—6353.2017.04.020.
10.3969/j.issn.1671—6353.2017.04.020
新疆医科大学第一附属医院小儿外科二病区 (新疆乌鲁木齐市,830054)
王玉杰,Email:493879845@qq.com
本文引用格式:李佳,威力江·赛买提,帕洛克·迪力木拉提,等.钬激光治疗后尿道瓣膜疾病的疗效评价[J].临床小儿外科杂志,2017,16(4):399—402.
Citing this article as:Li Jia,Wilijia Caimaiti,Paruh Dilmurat,Diar Dilmurat,etal.Holmium laser treatment of posterior urethral valve disease[J].J Clin Ped Sur,2017,16(4):399—402.DOI:10.3969/j.issn.1671—6353.2017.04. 020.
