胰腺黏液性囊性肿瘤的临床病理特点及良恶性影响因素分析
2017-08-30侯丽艳贾如江王秀超兰春根尹清臣
侯丽艳, 贾如江, 王秀超, 兰春根, 尹清臣
(1 邯郸市中心医院, 河北 邯郸 056102; 2 天津医科大学附属肿瘤医院, 天津 300060)
论著/胰腺疾病
胰腺黏液性囊性肿瘤的临床病理特点及良恶性影响因素分析
侯丽艳1, 贾如江1, 王秀超2, 兰春根2, 尹清臣1
(1 邯郸市中心医院, 河北 邯郸 056102; 2 天津医科大学附属肿瘤医院, 天津 300060)
目的 探讨胰腺黏液性囊性肿瘤(MCN)的临床病理特点并分析其良恶性的影响因素。方法 回顾性分析2013年1月-2015年12月天津市肿瘤医院和邯郸市中心医院收治的经术后病理证实的43例胰腺MCN患者的临床资料,根据病理诊断结果分为良性组(包括黏液性囊腺瘤及胰腺MCN伴低/中级别异型增生)和恶性组(包括MCN伴高级别异型增生及MCN伴浸润癌)。总结2组患者的临床病理特点和影像学特征,分析胰腺MCN发生恶变的相关危险因素。计量资料组间比较采用独立样本t检验,计数资料组间比较采用χ2检验,多因素分析采用logistic回归分析。结果 43例患者中男14例,女29例,年龄22~81岁,中位年龄58.53岁。有临床症状的患者30例(69.8%)。肿瘤最大直径4.8 cm(1.2~16 cm)。肿瘤位于胰头部18例(41.9%),胰颈3例(7.0%),体尾部20例(46.5%),2例(4.6%)为多发。2组患者在年龄、肿瘤性质、肿瘤部位、质地、肿瘤标志物、囊壁不均质强化、伴有实性成分不均质强化、囊壁厚度>0.2 cm上差异均有统计学意义(P值均<0.05)。多因素logistic回归分析显示年龄、肿瘤标志物升高是恶性胰腺MCN的独立预测因素(P值均<0.05)。结论 年龄、肿瘤性质、肿瘤部位、质地、肿瘤标志物升高、囊壁不均质强化、伴有实性成分不均质强化、囊壁厚度>0.2 cm为恶性胰腺MCN的重要特点,其中年龄、肿瘤标志物升高为恶性胰腺MCN的独立危险因素。
胰腺疾病; 肿瘤, 囊性, 黏液性和浆液性; 病理状态, 体征和症状; 危险因素
胰腺黏液性囊性肿瘤(mucinous cystic neoplasm,MCN)是一类少见的胰腺外分泌囊性肿瘤。病理形态上由高柱状、产生黏液的上皮细胞构成囊壁,上皮细胞层下的卵巢样间质为胰腺MCN特征表现,是诊断MCN的必要条件[1]。随着医学诊疗技术的发展,胰腺囊性肿瘤诊断率较过去明显增高[2-3]。不同表型的胰腺MCN生物学行为及远期预后存在显著差异,现有研究关于胰腺MCN恶变的临床病理特征及影像学表现报道不一[4-5],而MCN的临床诊治策略则需要根据其生物学特征进行严格区分。因此,本研究通过回顾近3年收治的胰腺MCN患者的临床诊治资料,分析胰腺MCN的临床病理特点并对良恶性因素进行统计分析,以提高对恶性胰腺MCN的临床和影像学特征的认识,进而提高其诊治水平。
1 资料与方法
1.1 研究对象 回顾性分析2013年1月-2015年12月天津市肿瘤医院和邯郸市中心医院收治的经手术治疗的胰腺MCN患者43例。纳入标准:经手术治疗,病理诊断明确且具有完整的随访资料。收集患者的年龄、性别、主诉、有无黄疸、肿瘤部位、大小、肿瘤性质(实性、囊实性、囊性)、质地(质硬、质中、质软)、肿瘤标志物,影像学资料以及术后病理资料等。
1.2 临床病理及影像学特征比较 术后病理按照世界卫生组织消化系肿瘤分级标准(2010版)[1]进行病理诊断。根据病理诊断结果分为良性组(包括黏液性囊腺瘤及MCN伴低/中级别异型增生)和恶性组(包括MCN伴高级别异型增生及MCN伴浸润癌)。比较2组患者的基本临床资料、病理特征差异和影像学特征差异,影像学表现包括囊壁厚度、囊壁不均质强化、实性成分强化、有无分隔、有无壁内结节、囊壁或实性成分有钙化、胰管扩张、胆管扩张。
2 结果
2.1 一般资料 共收集43例患者,其中女29例(67.4%),男14例(32.6%)。年龄22~81岁,中位年龄58.53岁。有临床症状的患者30例(69.8%),主要症状为腹痛、腹胀、腹部不适、腰背部疼痛、黄疸、消瘦。肿瘤最大直径4.8 cm(1.2~16 cm)。肿瘤位于胰头部18例(41.9%),胰颈3例(7.0%),体尾部20例(46.5%),2例(4.6%)为头颈体多发肿瘤。术后病理类型包括MCN伴低/中级别异型增生28例,MCN伴高级别异型增生6例,MCN伴浸润癌9例。根据病理诊断结果分为良性组(包括MCN伴低/中级别异型增生)28例(65.1%),恶性组(包括MCN伴高等级别异型增生及MCN伴浸润癌)15例(34.9%)。恶性组包括局部癌变4例,侵及胰腺被膜及周围脂肪软组织8例,侵犯周围肠壁2例,侵犯胃壁1例。癌变为乳头状囊腺癌6例、中分化腺癌1例、中低分化腺癌1例、高分化腺癌1例、黏液腺癌1例、导管腺癌1例。
2.2 临床病理特征比较 结果显示,在性别、有无临床症状、肿瘤最大直径等方面的差异无统计学意义,而在年龄、肿瘤性质、肿瘤部位、质地、肿瘤标志物是否增高等方面的差异均有统计学意义(P值均<0.05)(表1)。
2.3 影像学检查结果 CT检查30例次,磁共振/磁共振胰胆管造影检查11例次,超声内镜检查4例次。良性组28例,影像学检查诊断为囊腺瘤4例,囊腺瘤/囊腺癌1例,囊腺瘤/实性假乳头状瘤1例,囊腺瘤/导管内乳头状黏液瘤(intraductal papillary mucinous neoplasm,IPMN)1例,囊腺癌1例,IPMN 2例,囊(实)性肿物18例。恶性组15例,影像学检查诊断为囊腺癌4例,胰腺癌3例,恶性囊实性肿物2例,IPMN 2例,囊(实)性肿物4例。胰腺MCN的主要影像学表现为囊壁明显,囊壁厚度>0.2 cm有21例(图1),囊壁不均质强化19例(图2),实性成分强化21例(图3),有分隔17例(图4),有壁内结节15例(图5),囊壁或实性成分有钙化17例(图6),胰管扩张14例,胆管扩张13例。2组患者影像学特征比较显示在囊壁厚度、囊壁不均质强化、实性成分强化上的差异有统计学意义(P值均<0.05)(表1)。
2.4 多因素分析 多因素logistic回归结果显示,年龄、肿瘤标志物升高是恶性胰腺MCN的独立预测因素(表2)。
3 讨论
目前认为,MCN具有潜在恶性,经由一个腺瘤逐步恶变为浸润癌的过程,从可根治的非浸润性癌发展为浸润性癌可能需要5~10年时间。在癌前病变阶段完整切除即可,恶变局限在原位癌和浸润癌阶段的手术治疗需要RO切除和淋巴结清扫[6],5年生存率高,预后较好[7]。恶性胰腺MCN术前诊断困难,临床症状特点结合影像学表现可能会提高诊断率。超声内镜结合细针穿刺可提高术前诊断率[8],但是该检为有创性,且可造成恶性肿瘤的播散,需要一定的技术设备,目前在我国难以大范围开展。因此,如何依据临床病理特点及影像学表现提高恶性MCN的诊断尤为重要。

表1 2组患者临床病理和影像学特征比较

图1 囊壁厚度>0.2 cm

图2 囊壁不均质强化

图3 实性成分强化

图4 囊内分隔

图5 壁内结节

图6 囊壁、实性成分钙化
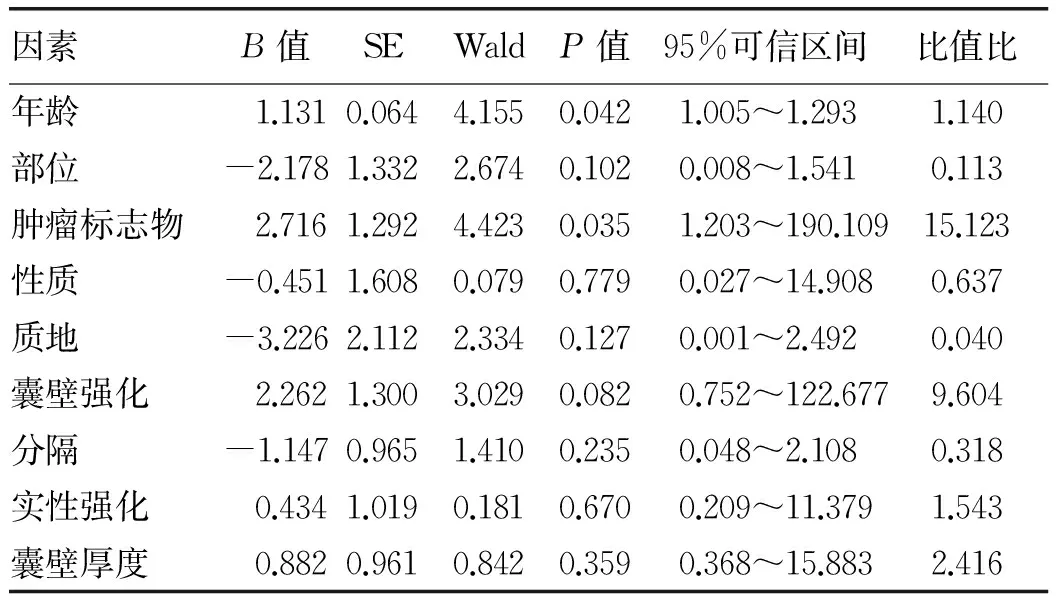
因素B值SEWaldP值95%可信区间比值比年龄1.1310.0644.1550.0421.005~1.2931.140部位-2.1781.3322.6740.1020.008~1.5410.113肿瘤标志物2.7161.2924.4230.0351.203~190.10915.123性质-0.4511.6080.0790.7790.027~14.9080.637质地-3.2262.1122.3340.1270.001~2.4920.040囊壁强化2.2621.3003.0290.0820.752~122.6779.604分隔-1.1470.9651.4100.2350.048~2.1080.318实性强化0.4341.0190.1810.6700.209~11.3791.543囊壁厚度0.8820.9610.8420.3590.368~15.8832.416
本组女性患者占67.4%,中位年龄58.53岁,肿瘤多位于体尾部46.5%,其次是胰头部41.9%和胰颈7.0%,少数为多部位。有临床症状者占69.8%,主要症状为腹痛、腹胀、腹部不适、腰背部疼痛、黄疸、消瘦。肿瘤最大径1.2~16 cm。共收治胰腺囊性肿瘤包括浆液性囊性肿瘤、MCN、实性假乳头状瘤、IPMN共182例,其中胰腺MCN 43例,约占囊性肿物的23.6%,较国内孙金山等[9]的报道结果明显升高,分析可能与收集病例的年代及地域差别有关。恶性组占MCN的34.9%,且本资料中男性患者占32.6%,肿瘤位于胰头部41.9%,比例均高于Han等[10]的报道结果,考虑与恶性病例升高有关。
国内严力等[11]报道在胰腺MCN良恶性的诊断过程中,囊壁厚度以及是否伴实性成分可作为重要的鉴别因素,与本研究结果一致,囊壁厚度、囊壁不均质强化、实性成分不均质强化在良性组和恶性组间差异均有统计学意义。多数研究[12]显示年龄是独立的预测因素,考虑与囊腺瘤逐步恶变的过程有关,即随着年龄的增大恶性患者明显增多。本研究还显示实性成分的增多、肿瘤质地变硬也是恶性MCN的预测因素。多因素logistic回归显示只有年龄、肿瘤标志物升高是恶性MCN的独立预测因素。
MCN具有恶变潜能,对于术前明确诊断的MCN患者均建议手术治疗[13],MCN预后良好,具体手术方式应根据肿瘤位置、大小、与周围邻近组织关系、术中冰冻病理决定。大多数MCN微浸润癌患者通过手术治愈[14],我国的胰腺囊性肿瘤的比例与西方国家不同,恰当的术前鉴别诊断仍具有挑战性[15]。本研究病例总体数较小,需要进一步大宗病例研究来证实这一结论。
[1] Editorial Board of Chinese Journal of Pancreatology. Consensus on pancreatic cystic neoplasm in China (draft in 2013, Shanghai)[J]. Chin J Pancreatol, 2013, 13(2): 79-90. (in Chinese) 中华胰腺病杂志编辑委员会. 我国胰腺囊性肿瘤共识意见(草案2013, 上海)[J]. 中华胰腺病杂志, 2013, 13(2): 79-90.[2] BUERKE B, DOMAGK D, HEINDEL W, et al. Diagnostic and radiological management of cystic pancreatic lesions: Important features for radiologists[J]. Clin Radiol, 2012, 67(8): 727-737.
[3] LI L, SUN B, ZHANG GQ, et al. Risk factors analysis of benign and malignant pancreatic cystic neoplasm and prognosis[J]. Chin J Dig Surg, 2016, 15(6): 562-566. (in Chinese) 李乐, 孙备, 张广权, 等. 影响胰腺囊性肿瘤良恶性及预后的危险因素分析[J]. 中华消化外科杂志, 2016, 15(6): 562-566.[4] JANG KT, PARK SM, BASTURK O, et al. Clinicopathologic characteristics of 29 invasive carcinomas arising in 178 pancreatic mucinous cystic neoplasms with ovarian-type stroma: implications for management and prognosis[J]. Am J Surg Pathol, 2015, 39(2): 179-187.
[5] CRIPPA S, SALVIA R, WARSHAW AL, et al. Mucinous cystic neoplasm of the pancreas is not an aggressive entity[J]. Ann Surg, 2008, 247(4): 571-579.
[6] TANAKA M, FERNNDEZ-DEL CASTILLO C, ADSAY V, et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas[J]. Pancreatology, 2012, 12(3): 183-197.
[7] LEWIS GH, WANG H, BELLIZZI AM, et al. Prognosis of minimally invasive carcinoma arising in mucinous cystic neoplasms of the pancreas[J]. Am J Surg Pathol, 2013, 37(4): 601-605.
[8] YOON WJ, BRUGGE WR. The safety of endoscopic ultrasound-guided fine-needle aspiration of pancreatic cystic lesions[J]. Endosc Ultrasound, 2015, 4(4): 289-292.
[9] SUN JS, ZHANG YZ, ZHOU YY, et al. Mucinous cystic neoplasm of the pancreas: clinical features of 125 patients[J]. Chin J Pancreatol, 2014,14(5): 321-325. (in Chinese) 孙金山, 张永镇, 周益胰, 等. 腺黏液性囊性肿瘤125例临床特征分析[J].中华胰腺病杂志, 2014, 14(5): 321-325.
[10] HAN KW, HA R, KIM KK, et al. Surgical management and results for cystic neoplasms of pancreas[J]. Korean J Hepatobiliary Pancreat Surg, 2013, 17(3): 118-125.
[11] YAN L, CHEN YL, ZHANG WZ, et al. Clinicopathological and CT features of mucinous cystic neoplasms of the pancreas[J]. Chin J Oncol, 2014, 36(6): 446-450. (in Chinese) 严力, 陈永亮, 张文智, 等. 胰腺黏液性囊性肿瘤的临床病理特点和CT影像学特征[J].中华肿瘤杂志, 2014, 36(6): 446-450.
[12] LI XD, LIU YJ, ZHU LW, et al. Clinical correlative factors of malignant cystic pancreatic tumors[J]. Chin J Dig Surg, 2012, 11(4): 343-345. (in Chinese) 李晓丹, 刘毓键, 朱理玮, 等. 恶性胰腺囊性肿瘤的临床相关因素分析[J]. 中华消化外科杂志, 2012, 11(4): 343-345.
[13] ZHANG JL, GE CL. Clinical features of pancreatic cystic neoplasms and its therapeutic strategy[J]. J Clin Hepatol, 2016, 32(5): 860-863. (in Chinese) 张家利, 葛春林. 胰腺囊性肿瘤的临床特点及治疗策略[J]. 临床肝胆病杂志, 2016, 32(5): 860-863.
[14] LEWIS GH, WANG H, BELLIZZI AM, et al. Prognosis of minimally invasive carcinoma arising in mucinous cystic neoplasms of the pancreas[J]. Am J Surg Pathol, 2013, 37(4): 601-605.
[15] BAI X, YE L, ZHANG Q, et al. Surgical resection and outcome of pancreatic cystic neoplasms in China: analysis of a 16-year experience from a single high-volume academic institution[J]. World J Surg Oncol, 2014, 12(5): 228-232.
引证本文:HOU LY, JIA RJ, WANG XC, et al. Clinicopathological features of pancreatic mucinous cystic neoplasm and influencing factors for its malignancy[J]. J Clin Hepatol, 2017, 33(8): 1514-1517. (in Chinese) 侯丽艳, 贾如江, 王秀超, 等. 胰腺黏液性囊性肿瘤的临床病理特点及良恶性影响因素分析[J]. 临床肝胆病杂志, 2017, 33(8): 1514-1517.
(本文编辑:王 莹)
Clinicopathological features of pancreatic mucinous cystic neoplasm and influencing factors for its malignancy
HOULiyan,JIARujiang,WANGXiuchao,etal.
(HandanCentralHospital,Handan,Hebei056102,China)
Objective To investigate the clinicopathological features of pancreatic mucinous cystic neoplasm (MCN) and influencing factors for benign and malignant MCN. Methods A retrospective analysis was performed for the clinical data of 43 patients with pathologically confirmed pancreatic MCN who were treated from January 2013 to December 2015, and according to the results of pathological diagnosis, the patients were divided into benign group (mucinous cystadenoma and pancreatic MCN with low/middle-grade dysplasia) and malignant group (MCN with high-grade dysplasia and MCN with invasive carcinoma). The clinicopathological features and radiological features were summarized, and the risk factors for malignant transformation of pancreatic MCN were analyzed. The independent samplest-test was used for comparison of continuous data between groups, the chi-square test was used for comparison of categorical data between groups, and a multivariate logistic regression analysis was used to identify risk factors. Results There were 14 male and 29 female patients aged 22-81 years (median 58.53 years). Of all patients, 30 (69.8%) had clinical symptoms. The maximum tumor diameter was 4.8 cm (range 1.2-16 cm). Of all patients, 18 (41.9%) had MCN in the head of the pancreas, 3 (7.0%) had MCN in the neck of the pancreas, 20 (46.5%) had MCN in the body and tail of the pancreas, and 2 (4.6%) had multiple MCNs. There were significant differences between the two groups in age, tumor nature, tumor location, texture, tumor markers, heterogeneous enhancement of the cyst wall, heterogeneous enhancement of solid components, and cyst wall thickness >0.2 cm(allP<0.05). The multivariate logistic regression analysis showed that age and increased tumor markers were independent predictive factors for malignant pancreatic MCN (bothP<0.05). Conclusion Age, tumor nature, tumor location, texture, increased tumor markers, heterogeneous enhancement of the cyst wall, heterogeneous enhancement of solid components, and cyst wall thickness >0.2 cm are important features of malignant pancreatic MCN, and age and increased tumor markers are risk factors for malignant pancreatic MCN.
pancreatic diseases; neoplasms, cystic, mucinous, and serous; pathological conditions, signs and symptoms; risk factors
10.3969/j.issn.1001-5256.2017.08.021
2017-01-05;
2017-01-26。
侯丽艳(1971- ),女,副主任医师,主要从事重症医学的基础与临床研究,特别是重症胰腺疾病的临床研究。
贾如江,电子信箱:jiarujiang@126.com。
R735.9
A
1001-5256(2017)08-1514-04