三种药物对全身麻醉外科手术后恶心呕吐的预防作用
2017-08-24阿拉木斯任德辰
阿拉木斯,任德辰
·临床医学·
·论著·
三种药物对全身麻醉外科手术后恶心呕吐的预防作用
阿拉木斯,任德辰
目的 评估和比较昂丹司琼、格拉司琼和雷莫司琼对全身麻醉下进行的外科手术后的恶心呕吐(postoperative nausea and vomiting, PONV)的预防作用。方法 90例被确诊为美国麻醉师协会(ASA)分级为I和II级患者,年龄20~65岁,预定在全身麻醉下进行外科手术。经患者知情同意,并签署知情同意书后,将全部患者分成3组,每组30例。昂丹司琼组:昂丹司琼0.1 mg/kg,格拉司琼组:格拉司琼40 μg/kg,雷莫司琼组:雷莫司琼0.3 mg,用5 ml生理盐水稀释药物后在麻醉前5 min通过静脉给药。在术后的第1个24 h,记录所发生的恶心、呕吐和干呕等症状情况。如没有发生恶心、呕吐、干呕和使用紧急止吐药则为完全发挥药效,以此评估药物的作用。用单因素方差分析和卡方检验对获得的数据进行观察。结果 术后0~3 h期间,所有实验组之间没有明显区别(P>0.05);在术后3~24 h期间,雷莫司琼和昂丹司琼有明显的区别,昂丹司琼组70%的患者无恶心、呕吐和干呕,雷莫司琼组93%的患者无恶心、呕吐和干呕,2组比较差异有统计学意义(P<0.05)。然而,在同样的时期格拉司琼和雷莫司琼之间没有区别(P>0.05)。结论 术后0~3 h内,所有的研究药物对预防恶心、呕吐和干呕的作用没有明显的区别。在术后3~24 h阶段,格拉司琼和雷莫司琼与昂丹司琼相比能更好的预防PONV。
全身麻醉;外科手术;恶心呕吐; 昂丹司琼;格拉司琼;雷莫司琼
外科手术后的恶心呕吐(postoperative nausea and vomiting, PONV)是施行全身麻醉的外科手术中最有危险性的副作用。PONV导致伤口裂开、出血、误吸、电解质紊乱、延长出院时间和减少患者的安全性等并发症。导致PONV发生的因素较多,包括患者、手术和麻醉相关因素。患者相关的因素有年龄、体质量、性别、术前存在的疾病、术后恶心、呕吐、干呕病史和吸烟史。有趣的是,不吸烟者发生PONV的倾向性是吸烟者的2倍[1]。预防PONV的药物有很多种,包括传统止吐药,如胃复安(多巴胺受体拮抗剂);最近引进的止吐药,如昂丹司琼、格拉司琼和雷莫司琼(5-羟色胺受体阻断剂)。探索这些药物在接受全身麻醉患者中预防PONV的潜力及其临床效果是本实验的目的。因此,可以通过实验评估比较昂丹司琼、格拉司琼和雷莫司琼在实施全身麻醉的外科手术后预防PONV的作用。
1 资料与方法
1.1 研究对象 本试验选择90例被确诊为美国麻醉师协会(ASA)分级I级和II级,年龄20~65岁,预定施行全身麻醉进行外科手术的患者。实验排除标准为:有晕动症病史,曾经发生术后恶心呕吐史,前庭病变,体质量指数(body mass index, BMI)>30和围术期24 h内使用过止吐药的患者。经医院伦理委员会的允许并通过书面形式告知患者。经患者知情同意,并签署知情同意书后,将全部患者分为3组,每组平均30人。
1.2 方法 所有的药物均用5 ml的生理盐水稀释后通过静脉给药,昂丹司琼0.1 mg/kg(昂丹司琼组)、格拉司琼40 μg/kg(格拉司琼组)和雷莫司琼0.3 mg(雷莫司琼组)。实验药物由单人准备,要求其不知道实验药物的使用情况。患者在术前建立好静脉通道后,进入手术室并且连接监护仪,在麻醉诱导前5 min对每个患者注射5 ml的实验药物。所有患者通过标准的麻醉诱导,使用曲马多(0.5 mg/kg)、丙泊酚(2 mg/kg)、罗库溴铵(0.6 mg/kg)进行气管插管。保持氧流量2 L/min,麻醉维持使用0.5%~2.0%的七氟醚和瑞芬太尼[0.25~2.0 μg/(kg·h)]根据手术进程和肌松情况追加罗库溴铵。术前监测包括持续的心电图、血压、心率、呼吸频率、血氧饱和度等生命体征。在手术结束时所有患者静脉注射新斯的明50 μg/kg拮抗残余的神经肌肉阻滞作用。在患者恢复自主呼吸后拔出气管导管,并送往恢复室。由同一实验者记录患者术后的恶心、呕吐和干呕的发生情况。紧急止吐药为从静脉注射0.2 mg/kg的胃复安。恶心的定义为令人不愉快的感觉联合呕吐的冲动。干呕是腹部肌肉不自主的有节律的收缩,但没有胃内容物排出。没有发生恶心、呕吐、干呕和不使用紧急止吐药则称为完全发挥药效。结果制作成表使用单因素方差分析或者使用卡方检验进行统计学分析。
2 结果
在昂丹司琼、格拉司琼和雷莫司琼3组患者中,年龄、体质量指数和麻醉时间没明显区别(P>0.05)。术后的0~3 h内,3组的PONV发生率差异无统计学意义(P>0.05)。见表1。昂丹司琼组:恶心13.3%,呕吐13.3%;格拉司琼组:恶心10%,呕吐13.3%;雷莫司琼组:恶心3.3%,呕吐6.7%。在昂丹司琼、格拉司琼和雷莫司琼3组中需要紧急止吐药患者的百分比分别为13.3%、13.3%和3.3%,而在术后3~24 h内分别为23.3%、10.0%和6.7%(表2)。术后0~3 h期间,3组之间药物对于预防恶心、呕吐、干呕和紧急止吐药的使用结果比较差异无统计学意义(P>0.05)。虽然无统计学意义,但在雷莫司琼组中仅有3.3%的患者使用了紧急止吐药。在术后的3~24 h期间,雷莫司琼与格拉司琼相比和昂丹司琼与格拉司琼相比,对于预防恶心、呕吐、干呕和紧急止吐药的使用结果比较差异无统计学意义(P>0.05)。然而,在术后的3~24 h期间,昂丹司琼与雷莫司琼的使用结果相比差异有统计学意义(P<0.05)(表3)。
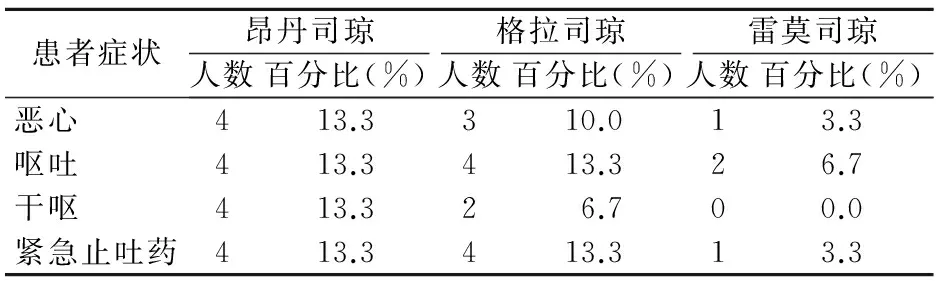
表1 昂丹司琼组、格拉司琼组和雷莫司琼组术后0~3 h发生恶心呕吐的情况(每组n=30)
3 讨论
PONV的病因是多因素的,与患者自身、外科手术和麻醉有着多种相关因素。患者相关的因素包括年龄、体质量、性别、存在的疾病、曾经有恶心呕吐病史、焦虑和吸烟。高发生率的外科手术如斜视手术、中耳手术,而使用阿片类药物,氯胺酮和新斯的明等药物也增加PONV的发生率。患者活动、血容量不足和过早的进行交流都可能增加患者发生PONV的风险。口服0.5 mg阿普唑仑保证晚上有好的睡眠,丙泊酚快速诱导麻醉和静脉注射75 mg双氢灭痛有助于减缓术前的焦虑和术后疼痛。本实验中药物使用的剂量是基于之前发表的文献。3组药物都是选择性的5-羟色胺-3受体拮抗剂对治疗患者的PONV是有效的[2]。5-羟色胺-3受体拮抗剂被视为预防化疗和放疗引起的呕吐的金标准。众所周知,在相同的有效剂量下5-羟色胺-3拮抗剂具有更明显的临床止吐作用和安全性。发现昂丹司琼、格拉司琼和雷莫司琼这3种药物明显减少术后3 h内的PONV发生率。然而,在术后3~24 h期间,昂丹司琼组和雷莫司琼组之间出现明显的不同。2010年Choi等[3]报道了相似的结果,证明在术后的6~24 h期间,雷莫司琼预防PONV的效果优于昂丹司琼。这一发现与Hahm等的研究一致[4]。在术后24 h期间,昂丹司琼和格拉司琼之间没有明显的区别,有些实验同样支持这一观点[5-7]。本研究未能在昂丹司琼组和格拉司琼组之间发现区别,可能与仅仅限制在24 h有关。总之,预防性的使用昂丹司琼、格拉司琼和雷莫司琼都能减少术后3 h内恶心和呕吐的发生率。然而,在术后的24 h内,雷莫司琼能够更有效地预防PONV的发生。
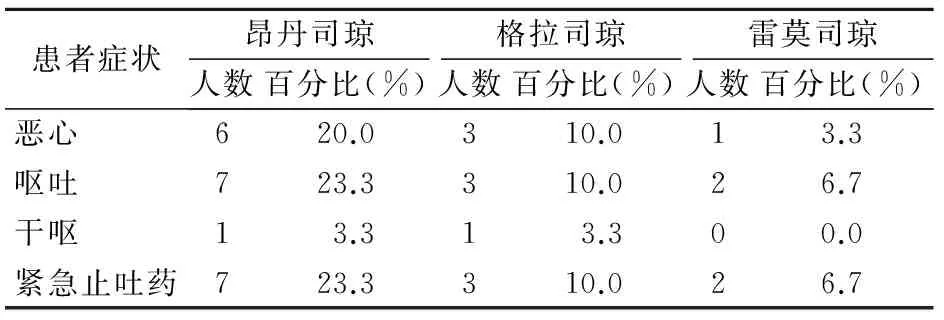
表2 昂丹司琼组、格拉司琼组和雷莫司琼组术后3~24 h发生恶心呕吐的情况(每组n=30)
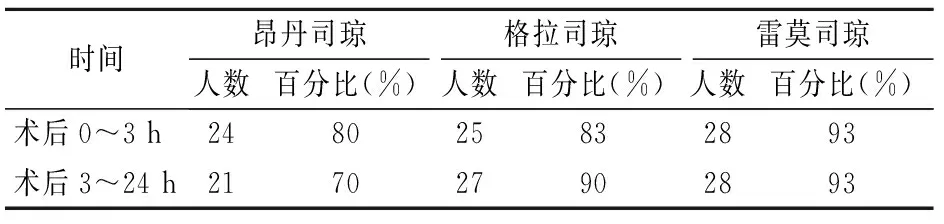
表3 术后昂丹司琼组、格拉司琼组和雷莫司琼组无恶心、呕吐和干呕的情况(每组n=30)
[1] Apfel CC, Stoecklein K, Lipfert P. PONV: a problem of inhalational anaesthesia[J]. Best Pract Res Clin Anaesthesiol, 2005, 19(3): 485-500. DOI:10.1016/j.bpa.2005.03.001.
[2] Kim SI, Kim SC, Baek YH, et al. Comparison of ramosetron with ondansetron for prevention of postoperative nausea and vomiting in patients undergoing gynaecological surgery[J]. British J Anaesth, 2009(4): 549-553. DOI:10.1093/bja/aep209.
[3] Choi YS, Shim JK, Yoon DH, et al. Effect of ramosetron on patient-controlled analgesia related nausea and vomiting after spine surgery in highly susceptible patients: comparison with ondansetron[J]. Spine, 2008, 33(17): E602-E606. DOI:10.1097/BRS.0b013e31817c6bde.
[4] Hahm TS, Ko JS, Choi SJ, et al. Comparison of the prophylactic anti-emetic efficacy of ramosetron and ondansetron in patients at high-risk for postoperative nausea and vomiting after total knee replacement[J]. Anaesthesia, 2010, 65(5): 500-504. DOI:10.1111/j.1365-2044.2010.06310.x.
[5] Fujii Y, Tanaka H, Ito M. Ramosetron compared with granisetron for the prevention of vomiting following strabismus surgery in children[J]. Br J Ophthalmol, 2001, 85(6): 670-672. DOI:10.1136/bjo.85.6.670.
[6] Schwartzberg L, Barbour SY, Morrow GR, et al. Pooled analysis of phase III clinical studies of palonosetron versus ondansetron, dolasetron, and granisetron in the prevention of chemotherapy-induced nausea and vomiting (CINV)[J]. Support Care Cancer, 2014, 22(2): 469-477. DOI:10.1007/s00520-013-1999-9.
[7] Lee WS, Lee KB, Lim S, et al. Comparison of palonosetron, granisetron, and ramosetron for the prevention of postoperative nausea and vomiting after laparoscopic gynecologic surgery: a prospective randomized trial[J]. BMC Anesthesiology, 2015, 15(1): 121-125. DOI:10.1186/s12871-015-0102-0.
(本文编辑:林永丽)
Protective effects of the 3 drugs on postsurgical nausea and vomiting under general anesthesia
Alamus,RenDechen
(HospitalofOnshoreServiceDepartmentofNavalVessels,Dalian161041,China)
Objective To evaluate and compare the preventive effects of ondansetron, granisetron and ramosetron on postsurgical nausea and vomiting under general anesthesia.Methods Ninety patients of ASA grade I and II with an age range of 20-65 years were scheduled for surgery under general anesthesia. With the knowledge and consent of the patients and following the signing of the letter of agreement, the patients were divided into 3 groups, each consisting of 30. The patients
the following drugs intravenously. The ondansetron group received 0.1 mg/kg ondansetron, the granisetron group was given granisetron at a dose of 40 μg/kg, and the ramosetron group had 0.3 mg ramosetron, which was diluted with 5 ml physiological saline and transfused intravenously 5 minute before surgery. Episodes of nausea, vomiting and retching were recorded in the first 24 hours after surgery. If there were no nausea, retching or vomiting or if acute antiemetic drug was used, it showed that the drugs had produced certain effect upon which the drugs were evaluated. Observation results were assessed and analyzed by using analysis of variance (ANOVA) and chi-square test.Results Within 0-3 hours after surgery, no statistical significance could be noted in all the study groups (P>0.05). Within the period of 3-24 hours, significant differences could be shown, when comparisons were made between the ramosetron group and the ondansetron group. Seventy per cent of the patients in the ondansetron group had no nausea and vomiting or retching, while 93% of the patients in the ramosetron group had no nausea and vomiting or retching. Statistical significance could be noted, when comparisons were made between them (P<0.05). However, during the period, no significant statistical differences could be seen between the granisetron and the ramosetron groups (P>0.05).Conclusion Within 0-3 hours after surgery, all the study drugs were not significantly different in the prevention of nausea, retching and vomiting. However, both ramosetron and granisatron were superior to ondansetron in the prevention of PONV within the period of 3-24 hours after surgery.
General anesthesia; Surgery; Nausea and vomiting; Ondansetron; Granisetron; Ramosetron
161041 辽宁 大连,解放军92538部队卫生处
任德辰,电子信箱:rendecheng1988927@163.com
R975.4
A
10.3969/j.issn.1009-0754.2017.04.021
2016-05-31)