基于DNA甲基化的宫颈癌基因治疗进展
2017-06-12唐倩倩郭剑锋华中科技大学同济医学院附属协和医院妇产科湖北武汉430022
周 萌,唐倩倩,刘 婷,郭剑锋 (华中科技大学同济医学院附属协和医院妇产科,湖北武汉430022)
基于DNA甲基化的宫颈癌基因治疗进展
周 萌,唐倩倩,刘 婷,郭剑锋 (华中科技大学同济医学院附属协和医院妇产科,湖北武汉430022)
宫颈癌是世界范围内严重威胁妇女健康的恶性肿瘤之一.研究表明伴随遗传学和表观遗传学改变的HPV感染,与宫颈癌的发生、发展以及恶变密不可分,而DNA甲基化正是这个复杂的癌变过程中很早发生,并且最频繁的一系列分子行为,其改变随着疾病进展而积累,目前已被认为是恶性宫颈癌的先兆,并被提议用于宫颈癌的早期监测、诊断和预后评估.本文主要讨论DNA甲基化对于临床上宫颈癌基因治疗的意义.
DNA甲基化;宫颈癌;基因治疗
0 前言
宫颈癌是世界范围内严重威胁妇女健康的恶性肿瘤之一,据GLOBOCAN统计,每年有近53万宫颈癌新发病例,超过26万患者因此失去了生命,其中85%以上来自发展中国家.在中国,由于宫颈筛查工作的不完善及女性对宫颈疾病的忽视,每年新增发病人数超过13万,占女性生殖系统恶性肿瘤发病率的73%~93%,更占据了约全球新发病例的1/4.值得注意的是,由于环境污染和生活中的不良卫生习惯,原本多发于50岁左右的女性宫颈癌,如今也“盯上”了年轻女性.分子流行病学研究已明确显示HPV感染与宫颈癌有着密切联系[1].
宫颈癌的发展是由正常上皮到低度鳞状上皮内病变(low-grade squamous intraepithelial leision,LSIL)、LSIL到高度鳞状上皮内病变(high-grade squamous intraepithelial leision,HSIL),再到宫颈原位癌(carcinoma in situ,CIS),最后形成转移癌.感染高危型HPV对于宫颈癌的来说是一个关键但不充分的条件[2-3].研究表明伴随遗传学和表观遗传学改变的HPV感染与宫颈癌的发生、发展及恶变密不可分,而DNA甲基化正是这个复杂的癌变过程中发生很早并且最频繁的一系列分子行为.DNA甲基化改变随着疾病进展而积累,目前已被认为是恶性宫颈癌的先兆,并被提议用于宫颈癌的早期监测、诊断和预后评估[4].
1 DNA甲基化
DNA甲基化是甲基基团在一系列DNA甲基转移酶的作用下转移至CpG二核苷酸胞嘧啶第五位点[5-7],在原核生物及真核生物,甚至病毒中都起着调控基因表达的重要作用[8],但有研究证明即使DNA不具备CpG位点,也能发生甲基化,只是程度会小得多[8-9].哺乳动物70%~80%的CpG胞嘧啶都有经过甲基化[10].在正常细胞中,DNA甲基化影响着基因表达调控、染色质激活/失活状态的控制、组织特异性表达以及基因印记[11].而在肿瘤细胞中,一方面,基因启动子区域的DNA超甲基化可以导致抑癌基因失活;另一方面,普遍的DNA低甲基化又会导致基因组不稳定性增加和细胞转化[12-13].可见,无论是DNA的超甲基化还是低甲基化都在宫颈癌发展过程中频繁发生,引起复杂的基因错误表达,包括致癌基因激活,抑癌基因失活,转座因子活动,印记丢失等,加剧了基因组的不稳定性和癌症发生[14].
2 宫颈癌和低甲基化
DNA的低甲基化是在包括癌症在内的许多疾病早期便存在并且频繁发生的重要基因激活机制.寄生序列、转座因子、致癌基因和原癌基因等被激活带来的甲基化导致了基因组不稳定性加剧和癌症的发生[15-16].在早期的研究中,通过与正常样本进行对照,Kim等[17]已证明宫颈癌和宫颈发育异常均与逐步发生的普遍DNA低甲基化有关.据报道,由于低甲基化所导致频繁发生的杂合性丢失与印记丢失也发生在宫颈癌中[18].Flowler等[19]的研究表明宫颈癌基因组的确与普遍的DNA低甲基化有关,而后者又与叶酸水平相关.大量的研究表明宿主基因组和HPV基因组在宫颈癌发生过程中都经历了低甲基化.Badal等[20]证明HPV基因组超甲基化可抑制瘤性转化,而低甲基化却能促进癌症发生.Missaoui等[21]的研究表明尽管癌前病变和正常人的甲基化水平差距甚微,但侵袭性宫颈癌样本却有明显的低甲基化.
3 宫颈癌与超甲基化
CpG岛和启动子区域的DNA超甲基化是基因沉默的重要机制,也是宫颈癌发生过程中的一类频繁并且早期出现的分子事件[22].在宫颈癌中,抑癌基因的失活与从低度鳞状上皮内病变到转移癌的每一步变化都紧密相连.过去几十年的表观遗传学研究已经证明DNA甲基化改变是宫颈癌的重要致病因素,能用于其早期监测、诊断、预后以及新治疗方法的发展[22].事实上已经证明超甲基化和基因沉默可干扰不受HPV感染影响的多条信号通路,涉及到细胞增殖、凋亡、细胞周期调控、DNA修复、细胞连接、血管再生、侵袭和转移[22].
4 宫颈癌与甲基化的临床应用
一些研究已经表明,基因的异常甲基化在宫颈癌发生的较早阶段就出现了,可用来作为早期检测的生物标记物.近来研究已明确鳞状细胞癌和腺癌中确定的甲基化模式,使之成为用于疾病分级和预后评估的合理选择[23].Thangavelu等[24]发现COL17A1启动子在乳腺癌中超甲基化,而在宫颈癌中低甲基化.COL17A1启动子的甲基化状态准确地预测了基因错误表达的方向和包括宫颈癌在内的五种上皮癌侵袭性的增加.这意味着COL17A1启动子甲基化的状态可用来预测患者结局,而且,针对COL17A1的表观遗传预示着能阻止患者癌灶转移的新方法.
4.1 甲基化的早期监测作用由于HPV可以被机体的免疫反应清除出体内,所以HPV感染并不都会导致宫颈癌,因此很有必要发展具有高度敏感性和特异性的选择性标记物,找出DNA甲基化特征将得到最佳临床效果.表观遗传改变被认为远早于遗传学改变,并在癌症的发生、进展及恶变过程中扮演了非常重要的角色[25].另外,异常的DNA甲基化早在低度鳞状上皮内病变时就有发生,因此可以单独或与现有监测方法联合用于宫颈癌早期诊断[22],该方法已被证实可以增加现有监测方法的敏感性和特异性.
与宫颈癌发生有关并且早期即发生DNA甲基化的例子有:CADM1、CACNA2D2、C13ORF18、DAPK1、MAI、MGMT、miR124-2、JAM3、PAX1、PCDHA4、PCDHA13、JAM3、RASSF1A、RAR-β2、SOX9、VIM[26-31].这些基因中某些基因的超甲基化可以在血、尿以及脱落细胞样本中检测到.DNA甲基化检测、HPV筛查及细胞学监测一起可以作为宫颈癌早期检查的有效方法.
4.2 甲基化的预后作用尽管目前宫颈癌的诊断是基于阴道镜、MRI及CT等多重检查手段的结果,但要预测药物治疗的敏感性却仍相当具有挑战性[32-33].一些学者认为异常的DNA甲基化可被有效运用于抗癌药物敏感性预测及预后评估.例如:Banno等[34]证明了CHFR基因超甲基化可作为预测紫杉醇在宫颈腺癌治疗敏感性的敏感性标记物.抗癌药物伊立替康(CRT-11)的敏感性是由Werner DNA解旋酶基因(WRN基因)的甲基化决定的;WRN基因被证明在人类宫颈鳞癌和腺癌细胞系中超甲基化并沉默,抑制WRN基因表达可以增加CRT-11的抗癌效果[35].宫颈癌 DNA甲基化调节基因中 APC1A、CHD1、CHD13、CACNA2D2、COX-2、DKK3、HPV-L1、LRIG1、MYOD1、RASSF1A、RASSF2、VIM有很明显的预后意义[29,36-44].除了甲基化调节基因,某些基因的异常表达在宫颈癌中也具有预后意义.例如:CD44v6、COX-2、CXCR7、EGFR、HIF-1α、MYC、survivin和XRCC1已被当作宫颈癌的主要治疗靶向,它们的高水平表达导致宫颈癌细胞对铂类药物反应不佳[45-46].尽管还未被结论性地证明,这些基因却很可能是通过DNA甲基化而得到调节.目前,针对HIF-1α的拓扑替康正处于宫颈癌治疗的第1和第2临床试验阶段[47-48].超甲基化基因在宫颈癌的预后总结于表1.
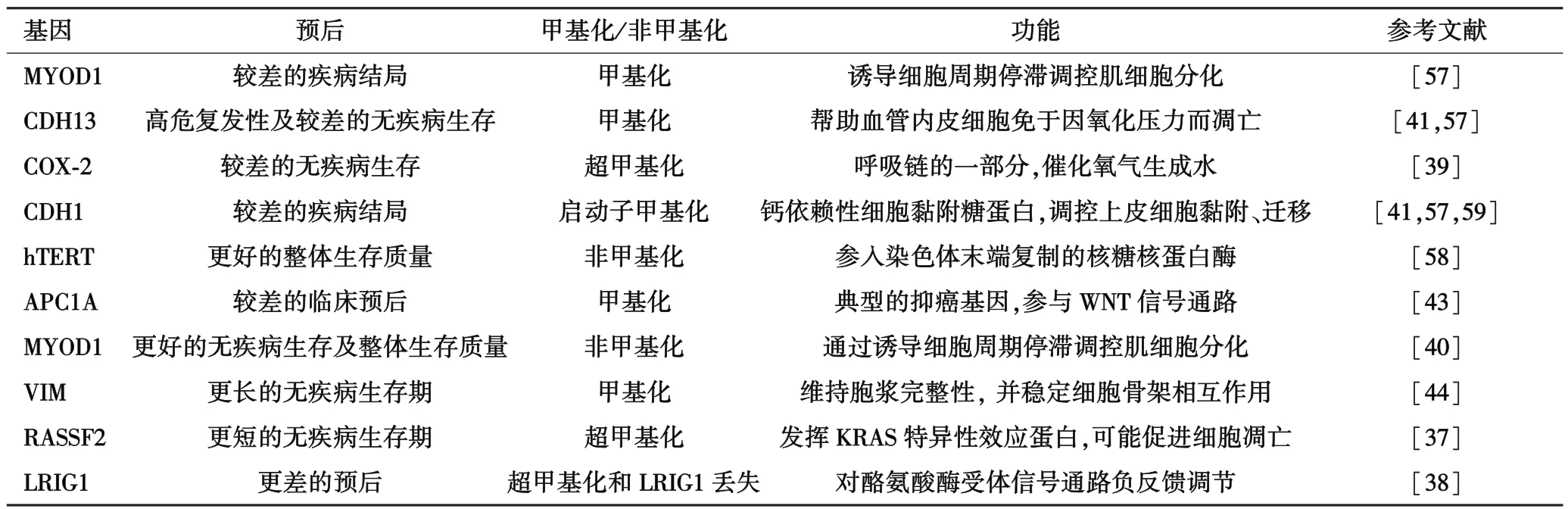
表1 超甲基化基因在宫颈癌的预后总结
4.3 甲基化与表观遗传治疗与遗传学改变不同,表观遗传改变的可逆性使得将它应用与疾病早期监测、诊断、疗效及预后评估成为可能.表观遗传的可逆性可用来恢复癌细胞对化疗药物的敏感性[49].目前,放化疗联合是宫颈癌治疗的标准方案,即在进行放疗时联用一种放射增敏剂——顺铂[50].目前用于表观遗传的药物分为两类:核苷类似物和非核苷类似物.①核苷类似物整合于DNA,并通过构成共价键封锁DNA甲基转移酶,现阶段正试验用于恶性血液病治疗[51].②非核苷类似物通过结合催化亚基封锁DNA甲基转移酶并限制其表达[52].一些研究表明在宫颈癌细胞系的治疗中通过启动子超甲基化可使沉默基因复活,Zambrano等[53]通过对4名患者管理肼苯哒嗪产生了APC和MGMT的去甲基化.ER,GSTP1,DAPK,RAR-β,FHIT以及p16INK4A这些基因中至少有一个发生去甲基化,程度如下:0 mg/d,40%;75 mg/d,52%;100 mg/d,43%;150 mg/d,32%.肼苯哒嗪剂量在50~100 mg/d之间的耐受性很好,达到明显的去甲基化效应以及在不改变普遍甲基化水平下的基因复活.Tanaka等[54]的研究则表明宫颈鳞状细胞癌对于SN38的耐药性可通过去甲基化药物治疗恢复敏感性.除此之外,去甲基化药物的细胞治疗也可使宫颈癌细胞对顺铂敏感[55-56].综上所述,表观遗传药物作为放疗增敏剂或化疗增敏剂具有巨大的潜力.
5 结论
不论是HPV还是宿主细胞基因组,在宫颈癌各个阶段都发生着大量表观遗传改变,包括普遍的低甲基化、关键肿瘤抑癌基因的超甲基化和组蛋白修饰.识别这些异常甲基化的基因可以生成非侵袭性生物标记物以用于早期监测、诊断、治疗方案的选择、评估疗效以及新治疗方法的探索.DNA甲基化标记物及甲基化程度千差万别,目前我们仍缺乏一个稳定的甲基化基因模版以应用于临床.因此,新的甲基化标记物需要被识别、监测、实践.一方面需要增加利用现有去甲基化药物的临床探索试验,借用甲基化谱分析识别应答因子及毒副作用.另一方面是要找出宫颈癌特异性的表观遗传驱动因子,然后对严格筛选后的患者行临床试验.这些标记物在目前宫颈癌监测和预后评估方面的应用很可能促进宫颈癌的个性化治疗及达到更好的临床结局.我们可以期待DNA去甲基化在未来的宫颈癌治疗中将占据一席之地.由于甲基化监测试验简单快速,稳定可靠,易于实现和理解,可以提供高度敏感和特异的信息.因此,我们需要后续的研究来阐明用于宫颈癌早期监测、诊断、预后评估及新治疗方法设计的标记物以更好地管理宫颈癌患者.对这些表观遗传改变的进一步研究将加深我们对宫颈癌的理解.另外,探索新的表观遗传改变标记物的实验正在进行中,这些将用于疾病监测.伴随DNA甲基化及组蛋白脱乙酰酶抑制剂,表观遗传的可逆性使得表观遗传治疗前景大好.
[1]zur Hausen H.Papillomaviruses causing cancer:evasion from host-cell control in early events in carcinogenesis[J].J Natl Cancer Inst,2000,92(9):690-698.
[2]Ho GY,Bierman R,Beardsley L,et al.Natural history of cervicovaginal papillomavirus infection in young women[J].N Engl J Med, 1998,338(7):423-428.
[3]Franco EL,Duarte-Franco E,Ferenczy A.Cervical cancer:epidemiology,prevention and the role of human papillomavirus infection[J].CMAJ,2001,164(7):1017-1025.
[4]Lai HC,Lin YW,Huang TH,et al.Identification of novel DNA methylation markers in cervical cancer[J].Int J Cancer,2008,123(1):161-167.
[5]Witte T,Plass C,Gerhauser C.Pan-cancer patterns of DNA methylation[J].Genome Med,2014,6(8):66.
[6]Auclair G,Weber M.Mechanisms of DNA methylation and demethylation in mammals[J].Biochimie,2012,94(11):2202-2211.
[7]Hermann A,Goyal R,Jeltsch A.The Dnmt1 DNA-(cytosine-C5)-methyltransferase methylates DNA processively with high preference for hemimethylated target sites[J].J Biol Chem,2004,279(46):48350-48359.
[8] Razin A,Riggs AD.DNA methylation and gene function[J].Science,1980,210(4470):604-610.
[9]Kozlenkov A,Roussos P,Timashpolsky A,et al.Differences in DNA methylation between human neuronal and glial cells are concentrated in enhancers and non-CpG sites[J].Nucleic Acids Res,2014,42(1):109-127.
[10]Jabbari K,Bernardi G.Cytosine methylation and CpG,TpG(CpA)and TpA frequencies[J].Gene,2004,333:143-149.
[11]Robertson KD.DNA methylation and human disease[J].Nat Rev Genet,2005,6(8):597-610.
[12]Chen RZ,Pettersson U,Beard C,et al.DNA hypomethylation leads to elevated mutation rates[J].Nature,1998,395(6697):89-93.
[13]Feinberg AP,Vogelstein B.Hypomethylation distinguishes genes of some human cancers from their normal counterparts[J].Nature,1983,301(5895):89-92.
[14]Chavez-Blanco A,Perez-Sanchez V,Gonzalez-Fierro A,et al.HER2 expression in cervical cancer as apotential therapeutic target[J].BMC Cancer,2004,4:59.
[15]Howard G,Eiges R,Gaudet F,et al.Activation and transposition of endogenous retroviral elements in hypomethylation induced tumors in mice[J].Oncogene,2008,27(3):404-408.
[16]Sigalotti L,Fratta E,Bidoli E,et al.Methylation levels of the“long interspersed nucleotide element-1”repetitive sequences predict survival of melanoma patients[J].J Transl Med,2011,9:78.
[17]Kim YI,Giuliano A,Hatch KD,et al.Global DNA hypomethylation increases progressively in cervical dysplasia and carcinoma[J].Cancer,1994,74(3):893-899.
[18]Douc-Rasy S,Barrois M,Fogel S,et al.High incidence of loss of heterozygosity and abnormal imprinting of H19 and IGF2 genes in invasive cervical carcinomas.Uncoupling of H19 and IGF2 expression and biallelic hypomethylation of H19[J].Oncogene,1996(2):423-430.
[19]Fowler BM,Giuliano AR,Piyathilake C,et al.Hypomethylation in cervical tissue:is there a correlation with folate status[J].Cancer Epidemiol Biomarkers Prev,1998,7(10):901-906.
[20]Badal V,Chuang LS,Tan EH,et al.CpG methylation of human papillomavirus type 16 DNA in cervical cancer cell lines and in clinical specimens:genomic hypomethylation correlates with carcinogenic progression[J].J Virol,2003,77(11):6227-6234.
[21]Missaoui N,Hmissa S,Dante R,et al.Global DNA methylation in precancerous and cancerous lesions of the uterine cervix[J].Asian Pac J Cancer Prev,2010,11(6):1741-1744.
[22]Yang HJ.Aberrant DNA methylation in cervical carcinogenesis[J].Chin J Cancer,2013,32(1):42-48.
[23]Lee EJ,McClelland M,Wang Y,et al.Distinct DNA methylation profiles between adenocarcinoma and squamous cell carcinoma of human uterine cervix[J].Oncol Res,2010,18(9):401-408.
[24]Thangavelu PU,Krenács T,Dray E,et al.In epithelial cancers,aberrant COL17A1 promoter methylation predicts its misexpression and increased invasion[J].Clin Epigenetics,2016,8:120.
[25]Jones PA,Baylin SB.The fundamental role of epigenetic events in cancer[J].Nat Rev Genet,2002,3(6):415-428.
[26]Wu JH,Liang XA,Wu YM,et al.Identification of DNA methylation of SOX9 in cervical cancer using methylated-CpG island recovery assay[J].Oncol Rep,2013,29(1):125-132.
[27]Eijsink JJ,Lendvai Á,Deregowski V,et al.A four-gene methylation marker panel as triage test in high-risk human papillomavirus positive patients[J].Int J Cancer,2012,130(8):1861-1869.
[28]Jung S,Yi L,Kim J,et al.The role of vimentin as a methylation biomarker for early diagnosis of cervical cancer[J].Mol Cells,2011,31(5):405-411.
[29]Mitra S,Mazumder indra D,Basu PS,et al.Alterations of RASSF1A in premalignant cervical lesions:clinical and prognostic significance[J].Mol Carcinog,2012,51(9):723-733.
[30]Yang N,Eijsink JJ,Lendvai A,et al.Methylation markers for CCNA1 and C13ORF18 are strongly associated with high-grade cervical intraepithelial neoplasia and cervical cancer in cervical scrapings[J].Cancer Epidemiol Biomarkers Prev,2009,18(11):3000-3007.
[31]仲肇基,杨佳欣,曹冬焱,等.子宫颈脱落细胞中DAPK1、RAR-β和MGMT基因启动子的甲基化水平及其临床意义[J].中华妇产科杂志,2012,47(3):196-200.
[32]Delgado G,Bundy B,Zaino R,et al.Prospective surgical-pathological study of disease-free interval in patients with stage IB squamous cell carcinoma of the cervix:a Gynecologic Oncology Group study[J].Gynecol Oncol,1990,38(3):352-357.
[33]Nicolet V,Carignan L,Bourdon F,et al.MR imaging of cervical carcinoma:a practical staging approach[J].Radiographics,2000,20(6):1539-1549.
[34]Banno K,Yanokura M,Kawaguchi M,et al.Epigenetic inactivation of the CHFR gene in cervical cancer contributes to sensitivity to taxanes[J].Int J Oncol,2007,31(4):713-720.
[35]Masuda K,Banno K,Yanokura M,et al.Association of epigenetic inactivation of the WRN gene with anticancer drug sensitivity in cervical cancer cells[J].Oncol Rep,2012,28(4):1146-1152.
[36]Oka N,Kajita M,Nishimura R,et al.L1 gene methylation in highrisk human papillomaviruses for the prognosis of cervical intraepithelial neoplasia[J].Int J Gynecol Cancer,2013,23(2):235-243.
[37] Guerrero-Setas D,Pérez-Janices N,Blanco-Fernandez L,et al.RASSF2 hypermethylation is present and related to shorter survival in squamous cervical cancer[J].Mod Pathol,2013,26(8):1111-1122.
[38]Lando M,Fjeldbo CS,Wilting SM,et al.Interplay between promoter methylation and chromosomal loss in gene silencing at 3p11-p14 in cervical cancer[J].Epigenetics,2015,10(10):970-980.
[39]Jo H,Kang S,Kim JW,et al.Hypermethylation of the COX-2 gene is a potential prognostic marker for cervical cancer[J].J Obstet Gynaecol Res,2007,33(3):236-241.
[40]Widschwendter A,Müller HM,Fiegl H,et al.DNA methylation in serum and tumors of cervical cancer patients[J].Clin Cancer Res,2004,10(2):565-571.
[41]Widschwendter A,Ivarsson L,Blassnig A,et al.CDH1 and CDH13 methylation in serum is an independent prognostic marker in cervical cancer patients[J].Int J Cancer,2004,109(2):163-166.
[42]Kang WS,Cho SB,Park JS,et al.Clinico-epigenetic combination including quantitative methylation value of DKK3 augments survival prediction of the patient with cervical cancer[J].J Cancer Res Clin Oncol,2013,139(1):97-106.
[43]Löf-öhlin ZM,Sorbe B,WINGREN S,et al.Hypermethylation of promoter regions of the APC1A and p16INK4a genes in relation to prognosis and tumor characteristics in cervical cancer patients[J].Int J Oncol,2011,39(3):683-688.
[44]Lee MK,Jeong EM,Kim JH,et al.Aberrant methylation of the VIM promoter in uterine cervical squamous cell carcinoma[J].Oncology,2014,86(5-6):359-368.
[45]Chung HH,Kim MK,Kim JW,et al.XRCC1 R399Q polymorphism is associated with response to platinum-based neoadjuvant chemotherapy in bulky cervical cancer[J].Gynecol Oncol,2006,103(3):1031-1037.
[46]Iida M,Banno K,Yanokura M,et al.Candidate biomarkers for cervical cancer treatment:Potential for clinical practice(Review)[J].Mol Clin Oncol,2014,2(5):647-655.
[47]Kummar S,Raffeld M,Juwara L,et al.Multihistology,target-driven pilot trial of oral topotecan as an inhibitor of hypoxia-inducible factor-1α in advanced solid tumors[J].Clin Cancer Res,2011,17(15):5123-5131.
[48]Rapisarda A,Shoemaker RH,Melillo G.Targeting topoisomerase I to inhibit hypoxia inducible factor 1[J].Cell Cycle,2004,3(2):172-175.
[49]Brown R,Curry E,Magnani L,et al.Poised epigenetic states and acquired drug resistance in cancer[J].Nat Rev Cancer,2014,14(11):747-753.
[50]Myrna C,Alicia GA,Lucely C,et al.Radiosensitizers in cervical cancer.Cisplatin and beyond[J].Radiat Oncol,2006(1):15.
[51]Egger G,Liang G,Aparicio A,et al.Epigenetics in human disease and prospects for epigenetic therapy[J].Nature,2004,429(6990):457-463.
[52]Sharma S,Kelly TK,Jones PA.Epigenetics in cancer[J].Carcinogenesis,2010,31(1):27-36.
[53]Zambrano P,Segura-pacheco B,Perez-cardenas E,et al.A phase I study of hydralazine to demethylate and reactivate the expression of tumor suppressor genes[J].BMC Cancer,2005,5:44.
[54] Tanaka T.Demethylation restores SN38 sensitivity in cells with acquired resistance to SN38 derived from human cervical squamous cancer cells[J].Oncol Rep,2012(27):1292-1298.
[55]Frost P,Abbruzzese JI,Hunt B,et al.Synergistic cytotoxicity using 2’-deoxy-5-azacytidine and cisplatin or 4-hydroperoxycyclophosphamide with human tumor calls[J].Cancer Res,1990,50(15):4572-4577.
[56]Sood S,Srinivasan R.Alterations in gene promoter methylation and transcript expression induced by cisplatin in comparison to 5-Azacytidine in HeLa and SiHa cervical cancer cell lines[J].Mol Cell Biochem,2015,404(1-2):181-191.
[57]Müller HM,Fiegl H,Widschwendter A,et al.Prognostic DNA methylation marker in serum of cancer patients[J].Ann N Y Acad Sci,2004,1022:44-49.
[58]Widschwendter A,Müller HM,Hubalek MM,et al.Methylation status and expression of human telomerase reverse transcriptase in ovarian and cervical cancer[J].Gynecol Oncol,2004,93(2):407-416.
[59]Chen CL,Liu SS,Ip SM,et al.E-cadherin expression is silenced by DNA methylation in cervical cancer cell lines and tumours[J].Eur J Cancer,2003,39(4):517-523.
R737.33
A
2095-6894(2017)05-70-04
2017-02-07;接受日期:2017-02-23
周 萌.E-mail:535911946@qq.com
郭剑锋.副主任医师,副教授.E-mail:jianfguo@outlook.com
