Ⅲ级睡眠呼吸监测设备在住院心血管疾病患者中监测的准确性评价
2017-06-05王玲章佳伟黄碧霞王锐罗建方陈纪言
王玲,章佳伟,黄碧霞,王锐,罗建方,陈纪言
Ⅲ级睡眠呼吸监测设备在住院心血管疾病患者中监测的准确性评价
王玲,章佳伟*,黄碧霞,王锐,罗建方,陈纪言
目的:评价Ⅲ级便携式睡眠呼吸监测设备(PM)在住院心血管疾病(CVD)患者中对睡眠呼吸暂停(SA)监测的准确性及应用价值。
方法:入选101例住院CVD患者,分别应用Ⅱ级多导睡眠呼吸监测设备(PSG)与Ⅲ级PM进行睡眠呼吸监测,比较两种监测设备的睡眠呼吸暂停低通气指数(AHI)结果。将AHI(单位:次/h)分为正常(AHI<5)、轻度(5≤AHI<15)、中度(15≤AHI<30)、重度(AHI≥30)4等级,计算Kendall相关系数、Kappa值,进行配对卡方检验。
结果:Ⅱ级PSG的AHI为(18.0±16.6)次/h,Ⅲ级PM的AHI为(18.6±17.4)次/h,差异无统计学意义(P>0.05)。AHI正常、轻度、中度、重度4等级,Kendall相关系数为0.701,P<0.01,呈强相关关系。一致性检验Kappa值为0.493,P<0.01,呈中等强度一致性。Ⅱ级PSG与Ⅲ级PM均以AHI≥15 次/h为诊断界值时一致性检验,Kappa值为0.679,P<0.05,呈高度一致性。以Ⅱ级PSG为标准作受试者工作特征(ROC)曲线分析,以AHI≥15 次/h为诊断界值时,Ⅲ级PM曲线下面积(AUC)为0.918,敏感度为80.4%,特异度为87.3%。Ⅲ级PM最佳诊断点为AHI=15.70次/h,此时约登指数最大,为0.695。
结论:对于住院CVD患者监测SA严重程度,Ⅲ级PM与Ⅱ级PSG相比,使用AHI≥15 次/h为诊断标准时一致性良好,具有较高的准确性。AHI=15.70 次/h为Ⅲ级PM诊断中重度SA的最佳截点。
睡眠呼吸暂停综合征;心血管疾病;睡眠呼吸监测
(Chinese Circulation Journal, 2017,32:485.)
睡眠呼吸暂停(SA)与各种心血管疾病(CVD)发病和预后高度相关[1,2],及时识别CVD患者的SA合并情况并给予治疗有利于改善患者症状[3,4]。研究表明80%的SA患者被漏诊[5]。睡眠呼吸监测是诊断SA的重要手段。睡眠呼吸监测分为四个等级:I级多导睡眠呼吸监测设备(PSG), Ⅱ级PSG,Ⅲ级便携式睡眠呼吸监测设备(PM),Ⅳ级单或双生物参数持续记录[6],Ⅰ级、Ⅱ级可诊断SA,Ⅲ级、Ⅳ级可筛查诊断SA[7]。CVD患者多存在睡眠维持困难,应选择对睡眠影响小的监测方式[8],使用PSG费用较高、操作复杂并且佩戴可能给患者睡眠造成负担,可接受性较差[9],难以满足住院CVD患者临床诊断的需要,Ⅲ级PM具有经济、易操作、对睡眠影响小、可开展随访等特点。本研究拟优化住院CVD患者SA的诊断模式,评价住院CVD患者应用Ⅲ级PM诊断SA的准确性。
1 资料与方法
研究对象:选取2015-06到2016-02在广东省人民医院心内科住院患者135例,年龄18~75岁,均签署知情同意书并获伦理委员会批准。最终101例完成Ⅱ级PSG和Ⅲ级PM睡眠呼吸监测,男性89例,女性12例,年龄(52±13)岁,体重指数(26.5±3.8) kg/m2。排除标准:拒绝完成监测,电极脱落,实际睡眠时间<2 h。采用自身前后对照设计,随机安排每例患者Ⅱ级和Ⅲ级两种监测设备的佩戴顺序,监测间隔时间为1~7天。
睡眠呼吸监测设备:Ⅱ级PSG采用倍德公司生产的Ⅱ级设备Compumedics Somté V2,参数包括:脑电、颏肌电、眼电、心电图、口鼻气流、胸腹呼吸运动、脉搏氧饱和度,采用设备配套的Profusion PSG4软件判读睡眠呼吸暂停低通气指数(AHI)。Ⅲ级PM采用飞利浦公司生产的Ⅲ级设备Alice PDx,参数包括:口鼻气流、胸腹呼吸运动、脉搏氧饱和度、脉率,采用配套的飞利浦Sleepware软件判读AHI。
判读标准:根据美国睡眠医学会(AASM)2.1版判读手册规则判读AHI[9],将AHI(单位:次/h)分为正常(AHI<5)、轻度(5 ≤AHI<15)、中度(15≤AHI<30)、重度(AHI≥30)4等级。AHI≥15 次/h为中重度SA诊断标准。不判读呼吸努力相关性觉醒(RERA)。
统计学方法:采用SPSS 19.0统计学软件分析结果。正态分布计量资料采用均数±标准差表示,用配对t检验进行比较。以两种监测仪测量所得AHI为连续型变量,进行配对t检验、Pearson相关分析,绘制Bland-Altman图评价所得AHI的一致性。按AHI 4等级资料,计算Kendall相关系数、Kappa值,进行配对卡方检验。以AHI≥15 次/h为诊断标准,计算两种监测仪AHI一致性Kappa值,作配对卡方检验。以Ⅱ级PSG所得AHI≥15次/h为界值,作受试者工作特征(ROC)曲线,分析计算Ⅲ级PM诊断的敏感度、特异度、阳性似然比、阴性似然比。P<0.05为差异有统计学意义。
2 结果
2.1 101例患者两种设备主要监测指标比较(表1)
101例患者两种设备监测AHI、最低脉氧及中重度SA比例,差异均无统计学意义(P均>0.05)。总记录时间Ⅱ级PSG高于Ⅲ级PM(P<0.05)。
表1 101例患者两种设备主要监测指标比较
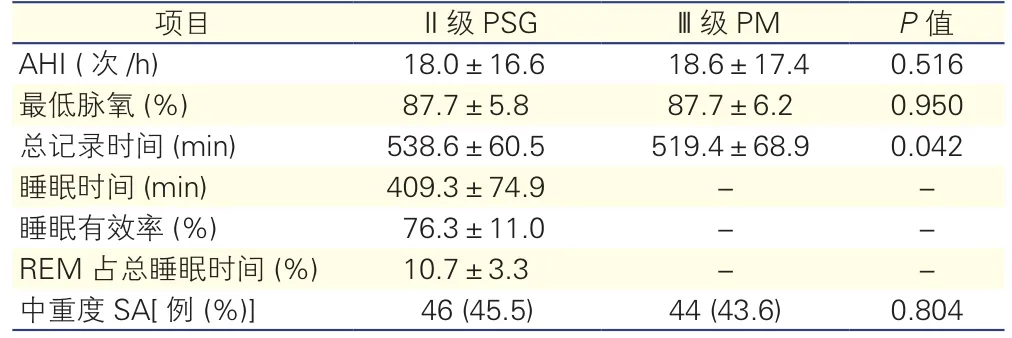
表1 101例患者两种设备主要监测指标比较
注: AHI: 睡眠呼吸暂停低通气指数;SA: 睡眠呼吸暂停;PSG:多导睡眠呼吸监测设备;PM:便携式睡眠呼吸监测设备;REM:快速眼动睡眠期;-:未测
项目 Ⅱ级PSG Ⅲ级PM P值AHI (次/h) 18.0±16.6 18.6±17.4 0.516最低脉氧 (%) 87.7±5.8 87.7±6.2 0.950总记录时间 (min) 538.6±60.5 519.4±68.9 0.042睡眠时间 (min) 409.3±74.9 - -睡眠有效率 (%) 76.3±11.0 - -REM占总睡眠时间 (%) 10.7±3.3 - -中重度SA[例 (%)] 46 (45.5) 44 (43.6) 0.804
2.2 以AHI为连续型变量作一致性分析结果
Pearson相关分析,Ⅱ级PSG与Ⅲ级PM所得AHI呈强相关(r=0.838,P<0.05),总体符合度高(图1)。从Bland-Altman散点图可以看出(图2),Ⅱ级PSG和Ⅲ级PM AHI差值为(0.63±9.73)次/h,95%一致性界限为-18.4 ~19.7次/h。5.0%(5/101)的点在95%一致性界限以外;在95%一致性界限范围内,Ⅱ级PSG与Ⅲ级PM的AHI差值的绝对值最大为19.40次/h。
2.3 以AHI为等级资料作一致性分析结果
Ⅱ级PSG 、Ⅲ级PM按AHI正常、轻度、中度、重度4等级资料分类的人数分布情况见表2。Kendall相关系数为0.701,P<0.01,呈强相关关系。一致性检验Kappa值为0.493,P<0.01,呈中等强度一致性。配对卡方检验P=0.631,两者根据等级资料分类差异无统计学意义。
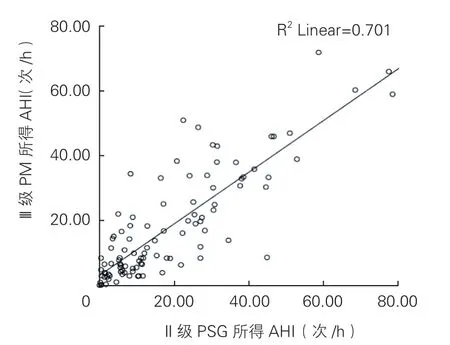
图1 两种设备AHI Pearson相关分析
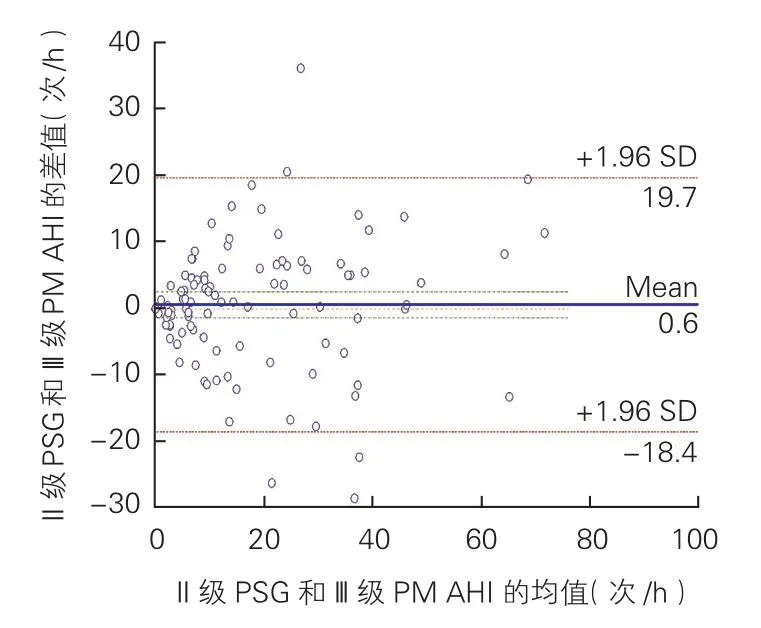
图2 两种设备AHI Bland-Altman散点图

表2 两种设备按AHI正常、轻度、中度、重度4等级资料分类的人数分布情况(例)
2.4 以Ⅱ级PSG的AHI≥15 次/h为诊断临界值时Ⅲ级PM与Ⅱ级PSG一致性及诊断价值评价
Ⅱ级PSG和Ⅲ级PM均以AHI≥15 次/h作为诊断SA的标准时,符合率为84.2%[(48+37)/101],一致性检验 Kappa值为0.679(P<0.05),可认为Ⅱ级PSG、Ⅲ级PM AHI呈高度一致性(表3)。以Ⅱ级PSG AHI≥15 次/h为诊断标准作ROC曲线,Ⅲ级PM曲线下面积0.918(图3)。取AHI≥15 次/h为临界值时,敏感度为80.4%,特异度为87.3%,约登指数0.677,阳性似然比6.331,阴性似然比0.225(表4)。根据ROC曲线,当AHI取15.70 次/h时为最佳诊断截点,此时约登指数最大,为0.695。
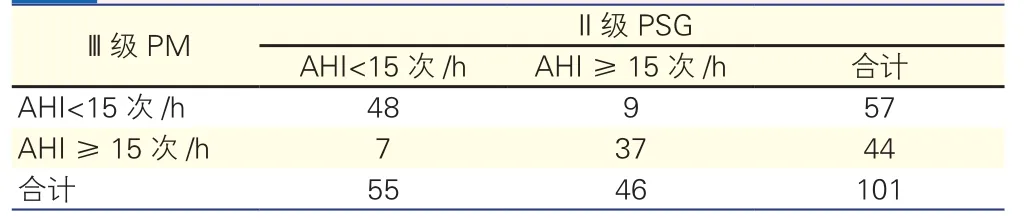
表3 两种设备以AHI≥15 次/h为诊断临界值的人数分布(例)
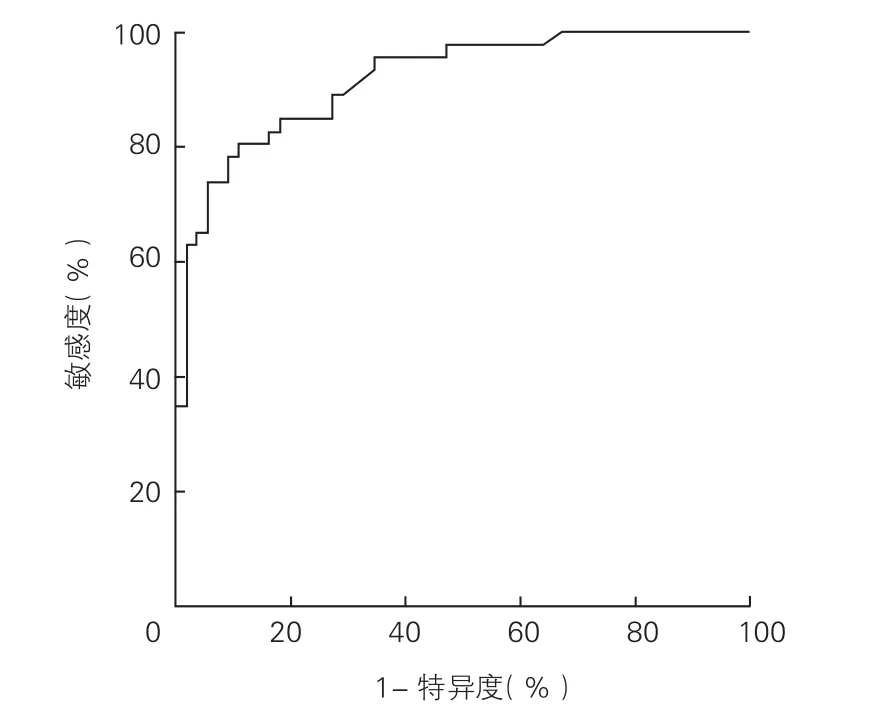
图3 以Ⅱ级PSG AHI≥15 次/h作为诊断标准时Ⅲ级PM的受试者工作特征曲线

表4 以Ⅱ级PSG AHI≥15 次/h为诊断临界值Ⅲ级PM诊断方法参数比较
3 讨论
本研究通过比较Ⅲ级PM和Ⅱ级PSG所得AHI值,两种监测方式一致性较高,以Ⅱ级PSG为参照,取AHI≥15 次/h为临界值时Ⅲ级PM诊断的准确性良好,AHI=15.70 次/h为Ⅲ级PM诊断SA的最优截点。本研究中Ⅱ级和Ⅲ级监测仪AHI呈强相关性,差异性小,以Ⅱ级为对照标准计算Ⅲ级ROC曲线下面积为0.918,有较高的诊断价值。
分析Ⅱ级PSG与Ⅲ级PM 监测差异的可能原因包括:(1)根据AHI计算原理Ⅱ级PSG AHI结果更为准确[7],但研究中发现Ⅲ级PM结果有接近10%患者的AHI高于Ⅱ级PSG。Santos等[10]也同样发现Ⅲ级PM AHI可能比Ⅱ级PSG AHI更高。(2)部分患者认为Ⅱ级PSG比Ⅲ级PM监测干扰睡眠。表现为入睡困难、睡眠维持困难和睡眠效率降低[8]。Ⅱ级PSG在信号采集过程中还存在电极脱落、脑电伪迹、颏肌电伪迹、设备干扰等问题[10-13]。住院CVD患者睡眠障碍发生率高[14]。本研究中患者(52±13)岁,Ⅱ级PSG监测平均睡眠有效率为(76.3±11.0)%,快速眼动睡眠期(REM)占总睡眠时间为(10.7±3.3)%,REM减少可致REM相关SA事件减少[6]。(3)体位改变。Ⅲ级PM监测患者比Ⅱ级PSG仰卧位时间长仰卧位REM睡眠中呼吸事件可能增多[15-19]。(4)首夜效应是影响睡眠时间、睡眠结构的另一重要因素[20]。(5)不同设备传感器、技术员之间判读的准确性可能存在误差[21-23]。
RERA是睡眠呼吸紊乱指数(RDI)的组成部分,但《国际睡眠疾病分类》第3版中诊断SA应用AHI,RERA在中重度患者中所占比例少[24]。按AASM判读手册2.1版Ⅱ级PSG在判读SA时RERA不是必须判读指标[9]。根据本研究结果,Ⅲ级PM可能比Ⅱ级PSG记录到更加接近真实睡眠情况下的呼吸事件,如操作规范,选用适当的诊断界值,选用Ⅲ级PM有利于优化住院心血管疾病患者的SA筛查诊断。
结论:对于住院CVD患者监测SA严重程度,Ⅲ级PM(Philip Alice PDx)与Ⅱ级PSG(Compumedics Somté V2)相比较,使用AHI≥15次/h为诊断标准时一致性及准确性良好,AHI=15.70次/h为Ⅲ级PM诊断中重度SA的最优截点。
[1] Somers VK. Braunwald's heart disease: a textbook of cardiovascular medicine: Sleep Apnea and Cardiovascular Disease. 9th edition. Philadelphia: Elsevier Health Sciences, 2012: 1719-1725.
[2] Somers VK, White DP, Amin R, et al. Sleep apnea and cardiovascular disease: an American Heart Association/american College Of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council On Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). Circulation, 2008, 118: 1080-1111.
[3] 蔡煦, 黄剑锋, 徐非, 等. 应用便携式多导睡眠监测仪对边远地区慢性心力衰竭伴睡眠呼吸暂停患者的临床意义. 中国循环杂志, 2015, 30: 433-437.
[4] 赵青, 柳志红, 罗勤, 等. 持续气道正压通气对冠心病合并阻塞性睡眠呼吸暂停患者血压和昼间嗜睡的影响. 中国循环杂志, 2012, 27: 365-368.
[5] Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep, 2008, 31: 1071-1078.
[6] Parati G, Lombardi C, Hedner J, et al. Recommendations for the management of patients with obstructive sleep apnoea and hypertension. Eur Respir J, 2013, 41: 523-538.
[7] Qaseem A, Dallas P, Owens DK, et al. Diagnosis of obstructive sleep apnea in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med, 2014, 161: 210-220.
[8] Redline S, Sanders MH, Lind BK, et al. Methods for obtaining and analyzing unattended polysomnography data for a multicenter study. Sleep Heart Health Research Group. Sleep, 1998, 21: 759-767.
[9] de Vries GE, van der Wal HH, Kerstjens HA, et al. Validity and Predictive Value of a Portable Two-Channel Sleep-Screening Tool in the Identification of Sleep Apnea in Patients With Heart Failure. J Card Fail, 2015, 21: 848-855.
[10] Santos-Silva R, Sartori DE, Truksinas V, et al. Validation of a portable monitoring system for the diagnosis of obstructive sleep apnea syndrome. Sleep, 2009, 32: 629-636.
[11] 中华医学会呼吸病学分会睡眠呼吸障碍学组. 阻塞性睡眠呼吸暂停低通气综合征诊治指南(2011年修订版). 中华结核和呼吸杂志, 2012, 35: 9-12.
[12] Yin M, Miyazaki S, Ishikawa K. Evaluation of type 3 portable monitoring in unattended home setting for suspected sleep apnea: factors that may affect its accuracy. Otolaryngol Head Neck Surg, 2006, 134: 204-209.
[13] 王莞尔, 高和. 睡眠中心外睡眠监测在诊断成人阻塞性睡眠呼吸暂停中的应用. 中华医学杂志, 2015, 95: 1203-1205.
[14] 李艳春, 王建秀. 心血管内科住院病人失眠相关因素分析及对策.护理研究, 2003, 17: 1067-1068.
[15] Li CK, Flemons WW. State of home sleep studies. Clin Chest Med, 2003, 24: 283-295.
[16] Levendowski D, Steward D, Woodson BT, et al. The impact of obstructive sleep apnea variability measured in-lab versus in-home on sample size calculations. Int Arch Med, 2009, 2: 2.
[17] Littner MR. Portable monitoring in the diagnosis of the obstructive sleep apnea syndrome. Semin Respir Crit Care Med, 2005, 26: 56-67. [18] BaHammam AS. Signal failure of type 2 comprehensive unattended sleep studies in patients with suspected respiratory sleep disordered breathing. Sleep Breath, 2005, 9: 7-11.
[19] El-Kersh K, Cavallazzi R, Patel PM, et al. Effect of Sleep State and Position on Obstructive Respiratory Events Distribution in Adolescent Children. J Clin Sleep Med, 2016, 12: 513-517.
[20] Ma J, Zhang C, Zhang J, et al. Prospective study of first night effect on 2-night polysomnographic parameters in adult Chinese snorers with suspected obstructive sleep apnea hypopnea syndrome. Chin Med J, 2011, 124: 4127-4131.
[21] Silva GE, Vana KD, Goodwin JL, et al. Identification of patients with sleep disordered breathing: comparing the four-variable screening tool, STOP, STOP-Bang, and Epworth Sleepiness Scales. J Clin Sleep Med, 2011, 7: 467-472.
[22] Ballester E, Solans M, Vila X, et al. Evaluation of a portable respiratory recording device for detecting apnoeas and hypopnoeas in subjects from a general population. Eur Respir J, 2000, 16: 123-127.
[23] Garde A, Dehkordi P, Karlen W, et al. Development of a screening tool for sleep disordered breathing in children using the phone Oximeter. PLoS One, 2014, 9: e112959.
[24] Somers VK. Frequency and accuracy of "RERA" and "RDI" terms in the Journal of Clinical Sleep Medicine from 2006 through 2012. J Clin Sleep Med, 2014, 10: 121-124.
Accuracy Assessment of Type III Portable Monitor of Sleep Apnea for In-hospital Patients With Cardiovascular Disease
WANG Ling, ZHANG Jia-wei, HUANG Bi-xia, WANG Rui, LUO Jian-fang, CHEN Ji-yan.
Department of Cardiology, Guangdong Provincial Hospital, Guangzhou (510080), Guangdong, China
WANG Ling, Email: 13922711188@163.com
Objective: To assess the accuracy and application value of type III portable monitor (III PM) of sleep apnea (SA) for in-hospital patients with cardiovascular disease (CVD).
��A total of 101 CVD patients
sleep apnea monitoring by both type II polysomnography ( II PSG) and III PM were enrolled to compare the apnea-hypopnea index (AHI) measured by 2 instruments. AHI was assigned into 4 grades: Normal (AHI<5), Mild grade (5≤AHI<15), Moderate grade (15≤AHI<30) and Severe grade (AHI≥30). Kendall correlation coeff i cient and Kappa value were calculated, pair wise t test was conducted in relevant patients.
Results: II PSG and III PM measured AHI were (18.0±16.6) events/h and (18.6±17.4) events/h, P>0.05. Kendall correlation coeff i cient for 4 AHI grades was 0.701, P<0.01 which assumed strong correlation; Kappa value of consistency was 0.493, P<0.01 which assumed medium strong correlation. Using AHI≥15 as cut-off point, Kappa coefficient for the consistency between II PSG and III PM was 0.679, P<0.05, which meant high consistency. Taking II PSG as standard and AHI≥15 as cut-off point, the AUC of III PM measured AHI was 0.918 with the specif i city at 80.4% and sensitivity at 87.3%. The best diagnosing cut-off value of III PM was AHI=15.70, at this point, the maximum Youden’s index was obtained as 0.695.
Conclusion: Using AHI≥15 as standard, III PM and II PSG had the favorable consistency and accuracy for monitoring the severity of SA for in-hospital patients with cardiovascular disease. AHI=15.7 was the best cut-off point of III PM indiagnosing moderate and severe SA in relevant patients.
Sleep apnea Cardiovascular disease Syndrom; Sleep apnea monitoring
2016-08-01)
(编辑:王宝茹)
广东省科技计划资助项目(2014A020212637)
510080 广东省广州市,广东省人民医院(广东省医学科学院) 广东省心血管病研究所 广东省冠心病重点实验室 心内科(王玲、章佳伟、王锐、罗建方、陈纪言);中山大学公共卫生学院(黄碧霞)
王玲 副主任医师 博士 主要研究方向为心血管疾病与睡眠呼吸暂停 Email:13922711188@163.com 通讯作者:王玲*为共同第一作者
R54
A
1000-3614(2017)05-0485-04
10.3969/j.issn.1000-3614.2017.05.015