经皮经肝胆囊穿刺引流术后择期行腹腔镜胆囊切除术治疗60岁以上急性重症胆囊炎患者的最佳时机探讨
2017-04-24赵红光刘亚辉
赵红光, 刘 凯, 刘亚辉
(吉林大学第一医院 肝胆胰外科, 长春 130021)
论著/胆道疾病
经皮经肝胆囊穿刺引流术后择期行腹腔镜胆囊切除术治疗60岁以上急性重症胆囊炎患者的最佳时机探讨
赵红光, 刘 凯, 刘亚辉
(吉林大学第一医院 肝胆胰外科, 长春 130021)
目的 观察经皮经肝胆囊穿刺引流术(PTGD)后择期行腹腔镜胆囊切除术(LC)治疗老年急性重症胆囊炎的效果,探究择期手术的最佳时机。方法 选取吉林大学第一医院肝胆胰外科2015年1月-2016年6月收治的行PTGD的60岁以上急性重症胆囊炎患者90例,根据择期LC时间将其分为3组:PTGD术后2个月内行LC(A组)、2~4个月行LC(B组)、4个月后行LC(C组),每组30例,观察PTGD的治疗效果及择期LC效果。计量资料2组间比较采用t检验,多组间比较采用方差分析,进一步两两比较采用LSD-t检验。计数资料组间比较采用χ2检验。结果 90例患者均成功完成PTGD,腹痛缓解时间(2.52±0.76)h;术后24~72 h内体温恢复正常,实验室指标(白细胞、中性粒细胞、ALT、AST、TBil)较术前均明显改善(t值分别为8.339、8.386、15.194、17.340、12.761,P值均<0.05),无1例患者出现因穿刺所致的胆漏、胆道出血、气胸、结肠穿孔等并发症;无1例脱管再次行PTGD。3组患者的术前胆囊壁厚度、手术时间、术中出血量、住院时间、中转开腹率、并发症发生率差异均有统计学意义(F值分别为8.029、24.674、12.864、22.844;χ2值分别为12.345、8.750,P值分别为<0.001、<0.001、<0.001、<0.001、0.002、0.013),其中B、C组患者的术前胆囊壁厚度、手术时间、术中出血量、住院时间、中转开腹率、并发症发生率均低于A组,差异均有统计学意义(P值均<0.05),B组手术时间、术中输血量、住院时间明显小于C组(P值均<0.05)。结论 PTGD术后2~4个月内择期行LC治疗老年急性重症胆囊炎效果显著,且安全性高。
胆囊炎, 急性; 引流术; 胆囊切除术, 腹腔镜; 老年人
急性胆囊炎常伴恶心、呕吐、寒战、发热等症状,病情严重者可并发全身性黄疸,严重影响患者的身心健康,甚至危及生命安全[1-2]。故早期行积极有效的诊疗,对改善患者预后有着重要意义。
老年胆囊炎患者早期功能和生理储备系统能力明显降低,动脉硬化造成胆囊动脉闭塞,胆囊坏死及穿孔,免疫功能降低,极易发生中毒症状,甚至休克。另外,老年患者常伴多种基础内科疾病,因此增加了治疗难度[3]。老年急性重症胆囊炎手术风险高,不仅要考虑彻底性,还需注重安全性,以降低术后并发症[4]。急诊经皮经肝胆囊穿刺引流术(percutaneous transhepatic gallbladder drainage,PTGD)可避免高危患者腹腔镜胆囊切除术(LC)的创伤,减少并发症的发生,通过穿刺置管引流感染胆汁,降低胆囊腔内压力,减少毒素的吸收,减轻中毒症状,同时结合抗感染、营养支持等对症综合治疗可有效控制症状,为择期行LC赢得时间[5]。目前,研究者一致认为若急性重症胆囊炎患者经保守治疗未见好转,则行PTGD术后择期LC治疗,但术后择期的时机选择尚无统一的标准和意见[6]。为进一步探讨PTGD术后择期行LC的最佳手术时机,笔者对老年急性重症胆囊炎患者PTGD术后不同时期行LC治疗,取得了显著的疗效,现报道如下。
1 资料与方法
1.1 研究对象 选取本院肝胆胰外科2015年1月-2016年6月收治的老年急性重症胆囊炎患者。纳入标准:(1)年龄60~90岁,性别不限;(2)急性重症胆囊炎患者,诊断符合《急性胆道系统感染的诊断和治疗指南(2011版)》[7],并根据急性胆囊炎东京指南[8]分级为Ⅲ级,伴有器官功能障碍;(3)发病时间<72 h;(4)疑有胆囊化脓或坏疽,但未穿孔;(5)合并转氨酶、胆红素水平升高或者胰腺炎表现,但彩超和CT等检查未证实胆管结石;(6)经科室会诊确定不宜行急诊外科手术治疗者;(7)符合PTGD适应证且完成手术者;(8)PTGD术后行LC治疗者。排除标准:(1)合并出血性疾病及凝血功能障碍者;(2)确诊为胆囊息肉、胆总管结石、胆道恶性肿瘤者;(3)行急诊开腹胆囊切除术或LC者;(4)因各种因素导致PTGD术后多次穿刺治疗者;(5)临床资料不全,影响疗效和安全性评估准确性的患者。研究经本院伦理委员会审核批准,患者及家属均签署知情同意书。
1.2 治疗和分组方法 患者入院后给予常规禁食、胃肠减压、补液、抗菌药物等治疗,完善各项实验室和影像学检查。PTGD操作前肌注50 mg哌替啶注射液,取左侧卧位,反复B超检查确定穿刺部位,常规消毒、铺巾后使用2%利多卡因对穿刺点进行局部麻醉。麻醉成功后,切开皮肤0.2 cm,B超引导下用7-8 F猪尾形穿刺引流套管沿着针道经肝穿入胆囊,B超复查确定位于胆囊后拔出针芯,接注射器抽取部分胆汁,穿刺针拔出过程中间套管尾部推入并盘曲在胆囊内,固定引流管,连接引流装置,无菌敷料包扎并妥善固定引流管。将抽取的胆汁立即送检,进行细菌培养和药敏试验。术后严密监测患者生命体征、腹部体征和引流情况,同时给予抗感染、抑酸、保肝、止血、营养补液等综合治疗。另外,根据细菌培养和药敏试验结果调整抗菌药物,待患者症状和体征缓解后,可逐渐进食少许清淡食物,无不适者则可间断夹闭引流管,继而持续夹闭;若腹部症状、发热、疼痛等仍存在,则继续引流。
PTGD术后定期复查B超,根据恢复情况拔管和行LC。将纳入患者按LC时间分为3组:A组于PTGD术后2个月内行LC,B组于2~4个月行LC,C组于4个月后行LC。术前完善各项检查和准备,全身麻醉后采用3孔或者4孔法完成,对于仍携带PTGD引流管者拔除后建立气腹,于脐上、剑突下、右肋缘下建立10 mm和5 mm手术通道,按常规LC切除胆囊,自剑突下切口取出胆囊并送检。检查穿刺窦道是否有出血、胆漏等,根据术中情况决定是否留置腹腔引流管。对于术中出现不可控出血、胆道和周围脏器损伤、胆囊分离极为困难等导致无法完成LC者则转开腹胆囊切除术。
1.3 观察指标 PTGD术后观察患者临床症状和体征改善情况、体温恢复情况、实验室指标(白细胞、中性粒细胞、肝功能指标)改善情况以及并发症发生情况。同时,观察LC手术情况,主要包括术前胆囊壁厚度、手术时间、术中出血量、中转开腹、并发症、住院时间等。1.4 PTGD拔管指征 置管时间>7 d;无腹痛、发热、黄疸;胆汁颜色清澈透明,呈黄色或黄绿色,无脓液及絮状物;胆汁细菌培养阴性;胆囊壁厚度<5 mm,胆囊横径较前减小;实验室检查外周血白细胞、中性粒细胞、血清ALT、TBil水平恢复正常[9]。对于年龄>70岁、全身营养不良、严重低蛋白血症、重度贫血、长期服用类固醇药物者可适当延长带管时间,必要时行胆囊造影,确保窦道已形成。

2 结果
2.1 一般资料 共纳入老年急性重症胆囊炎患者90例,每组30例。3组患者性别构成比、年龄、病程、并发症等基线资料比较,差异均无统计学意义(P值均>0.05)(表1)。
2.2 患者行PTGD前后体温及实验室指标比较 所有患者均成功完成PTGD,穿刺时间20~50 min,平均(32.58±7.36)min;术中胆汁引流量5~60 ml,平均(29.56±11.52)ml;腹痛缓解时间0.5 h~8 d,平均(2.52±0.76)h;进食时间1~4 d,平均(2.35±0.58)d。术后24~72 h内患者体温恢复正常,实验室指标(白细胞、中性粒细胞、肝功能)较术前均明显改善(P值均<0.05)(表2),无1例患者出现因穿刺所致的胆漏、胆道出血、气胸、结肠穿孔等并发症。置管时间7~49 d,平均(22.58±10.36)d,无1例脱管再次行PTGD。
2.3 3组患者LC观察指标比较 3组患者均无1例死亡。3组患者的术前胆囊壁厚度、手术时间、术中出血量、住院时间、中转开腹率、并发症发生率差异均有统计学意义(P值均<0.05)。B、C组术前胆囊壁厚度、手术时间、术中出血量、住院时间、中转开腹率、并发症发生率均低于A组(P值均<0.05);B组手术时间、术中输血量、住院时间均明显低于C组(P值均<0.05)(表3)。
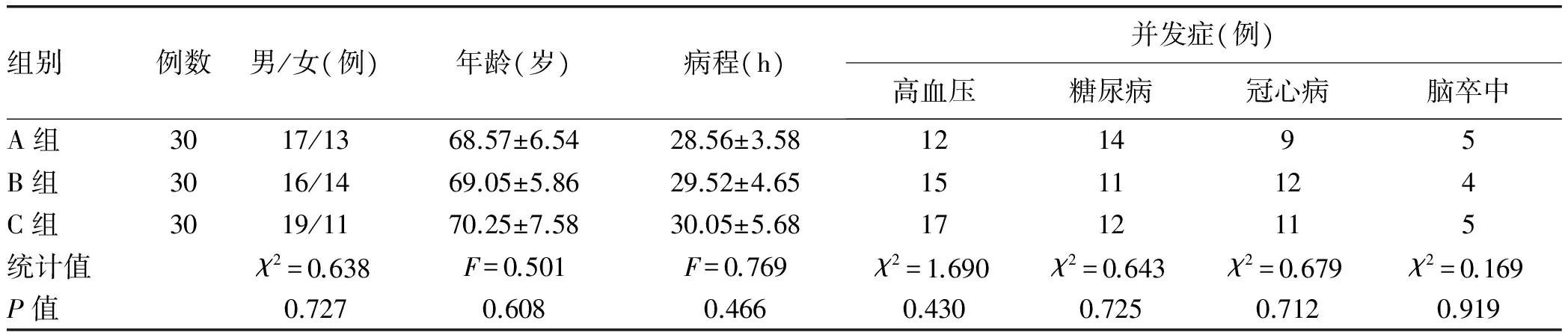
表1 3组患者一般资料
表2 PTGD术前和术后24~72 h体温及实验室指标比较

表3 3组患者LC手术相关指标比较
注:与A组比较,1)P<0.05;与B组比较,2)P<0.05
3 讨论
急性重症胆囊炎是临床常见的急腹症之一,老年重症胆囊炎起病急骤、病情进展快、急诊手术困难,可导致肝功能严重损伤甚至衰竭、胆囊坏疽穿孔、弥漫性腹膜炎以及败血症等多种严重并发症,未经及时处理可致患者死亡,故临床一旦确诊则需急诊处理[10]。急性胆囊炎患者明确诊断后立即给予禁食、营养支持、抗感染、补充维生素、纠正水电解质和酸碱平衡等综合保守治疗,多数患者病情可得到控制,为择期手术创造机会[11-12];对于病情无好转且逐渐加重者应行急诊手术[13]。目前临床常用的手术方式为传统开腹术、胆囊造瘘术、PTGD、LC等,长期实践发现急性胆囊炎最彻底的治疗方案为胆囊切除术。随着腹腔镜技术的逐渐发展,LC成为急性胆囊炎较常用的手术方式,其疗效确切且安全性高[14-16],但目前对于行LC时机的选择仍有众多争议[17],有待进一步的深入研究。
研究[18-19]报道急性胆囊炎症状出现的24~72 h内最宜行胆囊切除术,若发病时间超过72 h,胆囊和周围组织炎症较重,局部组织充血、水肿甚至坏死,与周围组织黏连严重进而明显增加手术难度,中转开腹率高,尤其是对于老年重症胆囊炎患者;麻醉和气腹亦会增加LC的手术风险[20]。此外,因老年重症胆囊炎患者症状重、胆囊三角结构模糊难以分离、极易出血和损伤胆总管,中转开腹率、术后并发症发生率及病死率高[21],故需要一种可快速缓解临床症状的干预方法即胆囊减压引流术。PTGD是临床常用的一种微创、操作简单、疗效确切的胆道持续引流减压治疗方法,不受年龄、病情的影响[22],在B超、CT、X线引导下穿刺,避免盲目穿刺,增加了穿刺的精准性,可在床边完成,广泛应用于急性胆囊炎患者胆囊减压治疗,已替代了开腹胆囊引流术[23]。同期配合全身抗感染等支持治疗迅速缓解临床症状和体征,阻止病情进一步恶化,为并发症的治疗及择期行LC赢得充足时间[24]。本研究纳入患者均成功完成PTGD,且无穿刺所致并发症发生,腹痛缓解和炎症消退快,再次证实上述观点。故常采用PTGD引流炎性胆汁,待炎症完全消退和体质状况恢复后再行LC,可明显降低手术难度及风险,提高临床疗效并改善患者预后[25]。
关于PTGD术后行LC时机的选择存在众多争议,术后1周行LC中转开腹率较高;术后3周左右行LC操作困难,且术后并发症发生率高,影响患者术后早期恢复,不符合目前外科快速康复理念;术后4~5周行LC可能存在胆囊三角严重黏连情况,手术操作较为困难。故目前多建议PTGD术后2~4个月行LC,可明显缩短手术时间,减少术中出血量,降低中转开腹率,且术后并发症明显减少,有利于患者术后早期康复。但目前PTGD术后行LC的最佳时机尚无定论,主要取决于胆囊炎症消退情况及其他基本条件、医院设备、术者临床经验等,故笔者为进一步探究最佳的手术时机,对比分析了PTGD术后3个不同时期行LC患者的术中和术后情况,结果发现PTGD术后2个月行LC操作更为简单,术中出血量、中转开腹率较2个月内行LC患者明显降低(P值均<0.05);患者术后康复情况显示2个月后行LC较2个月内行LC,患者术后并发症明显减少,住院时间明显缩短(P值均<0.05);此外,2个月后胆囊壁厚度明显降低(P<0.05),提示PTGD术后2个月内胆囊内压力降低,但炎症尚未完全消退,胆囊壁水肿严重,胆囊周围黏连严重,局部解剖结构不清,胆囊三角分离难度大;2个月后胆囊炎症明显改善,局部黏连减轻,手术操作相对较容易,故笔者认为2个月后行LC较2个月内行LC效果更为显著。此外,2~4个月内行LC的手术时间、术中出血量、中转开腹率、住院时间均明显低于4个月后行LC者,结果与邱明[26]和姜庆贺等[27]报道一致,故认为2~4个月内行LC患者并发症少、恢复较快,可极大程度减轻患者的痛苦,完全符合快速康复理念。此外,笔者认为PTGD术后应动态复查胆囊壁厚,若2~4个月内胆囊壁厚≤4.2 mm则可视为LC最佳的手术时机,但尚需后期大样本、多中心系统性研究证实。
综上所述,PTGD术后2~4个月内择期行LC治疗老年急性重症胆囊炎可明显缩短手术时间、减少术中出血量,降低中转开腹率和并发症发生率,术后恢复较快,具有极其重要的临床意义和价值。
[1] XIA MF, ZHANG S, TIAN H, et al. Study of the effects of percutaneous transhepatic gallbladder drainage guided by B ultrasound in the treatment of elderly patients with critical calculus obstructive cholecystitis[J]. China J Modern Med, 2014, 24(21): 102-105. (in Chinese) 夏明峰, 张帅, 田虎, 等. B超引导下经皮肝胆囊穿刺治疗老年危重结石梗阻性胆囊炎[J]. 中国现代医学杂志, 2014, 24(21): 102-105.
[2] HUA SY, XU RL, QI B, et al. Clinical value of percutaneous gallbladder catheterized drainage in the treatment of acute severe cholecystitis[J]. J Southeast Univ: Med Sci Edit, 2014, 33(4): 479-481. (in Chinese) 华双一, 徐仁良, 祁波, 等. 经皮胆囊穿刺置管引流治疗高危急性胆囊炎[J]. 东南大学学报: 医学版, 2014, 33(4): 479-481.[3] PEPINGCO L, ESLICK GD, COX MR. The acute surgical unit as a novel model of care for patients presenting with acute cholecystitis[J]. Med J Aust, 2012, 196(8): 509-510.
[4] FEI HJ, SU ZJ, PAN QX, et al. Clinical effet of percutaneous transhepatic gallbladder drainage combined with selective laparoscopic cholecystectomy in treatment of acute severe cholecysitis: an analysis of 386 cases[J]. J Hepatopancreatobiliary Surg, 2014, 26(6): 486-488. (in Chinese) 费洪江, 苏子剑, 潘群雄, 等. 经皮经肝胆囊穿刺引流术加择期腹腔镜胆囊切除术治疗急性重症胆囊炎386例分析[J]. 肝胆胰外科杂志, 2014, 26(6): 486-488.
[5] ABI-HAIDAR Y, SANCHEZ V, WILLIAMS SA, et al. Revisiting percutaneous cholecystostomy for acute cholecystitis based on a 10-year experience[J]. Arch Surg, 2012, 147(5): 416-422.
[6] JIANG B. The research of opportunity selection in acute calculous cholecystitis laparoscopic cholecystectomy[D]. Dalian: Dalian Med Univ, 2014. (in Chinese) 江滨. 急性结石性胆囊炎腹腔镜手术时机的选择[D]. 大连医科大学, 2014.
[7] Biliary Surgery Group, Surgery Branch of Chinese Medical Association. Diagnosis and treatment guidelines for acute biliary infection (2011 edition)[J]. Chin J Dig Surg, 2011, 10(1): 9-13. (in Chinese) 中华医学会外科学分会胆道外科学组. 急性胆道系统感染的诊断和治疗指南(2011版)[J].中华消化外科杂志, 2011, 10(1): 9-13.[8] YAMASHITA Y, TAKADA T, KAWARADA Y, et al. Surgical treatment of patients with acute cholecystitis: Tokyo guidelines[J]. J Hepatobiliary Pancreat Surg, 2007, 14(1): 91-97.
[9] XU D. Study on indications for extubation of percutaneous transhepatic gallbladder drainage[D]. Shihezi: Shihezi Univ, 2014. (in Chinese) 徐东. 经皮经肝胆囊穿刺引流术后拔管指征的探讨[D]. 石河子大学, 2014.
[10] JIANG JT, LI Q. Clinical effect of sequential percutaneous transhepatic gallbladder drainage and laparoscopic cholecystectomy in treatment of acute severe cholecystitis in elderly patients[J]. Zhejiang Pract Med, 2015, 20(3): 206-207. (in Chinese) 蒋建庭, 李巧. 经皮经肝胆囊穿刺引流术序贯腹腔镜胆囊切除术治疗老年急性重症胆囊炎[J]. 浙江实用医学, 2015, 20(3): 206-207.
[11] ZHANG JJ, LI HZ. Clinical analysis of Lidan Paishi Tang in expectant treatment of chronic cholecystitis[J]. Chin J Exp Med Formul, 2016, 22(7): 187-190. (in Chinese) 张洁靖, 李汉智. 利胆排石汤保守治疗慢性胆囊炎的临床分析[J]. 中国实验方剂学杂志, 2016, 22(7): 187-190.
[12] XIE MP, WANG J. Current research status of acute cholecystitis in elderly patients[J]. Trauma Crit Med, 2016, 4(1): 62-64. (in Chinese) 解民鹏, 王静. 高龄患者急性胆囊炎研究现状[J]. 创伤与急危重病医学, 2016, 4(1): 62-64.
[13] LENG K, LUO YQ, ZENG PF. Percutaneous transhepatic gallbladder catheterizing drainage guided by ultrasound for acute severe cholecystitis in the senile patients[J]. China J Modern Med, 2014, 24(24): 86-88. (in Chinese) 冷凯, 罗燕青, 曾鹏飞. 老年急性胆囊炎经皮经肝胆囊穿刺引流术应用[J]. 中国现代医学杂志, 2014, 24(24): 86-88.
[14] HUANG ZM, XU L, ZHOU D. Laparoscopic cholecystectomy for acute cholecystitis[J]. Chin J Gen Surg, 2012, 21(8): 1038-1040. (in Chinese) 黄志明, 徐亮, 周栋. 腹腔镜胆囊切除术治疗急性胆囊炎[J]. 中国普通外科杂志, 2012, 21(8): 1038-1040.
[15] WANG WH. Clinical efficacy of percutaneous transhepatic cholecystostomy combined with laparoscopic cholecystectomy for elderly patients with severe calculous cholecystitis[J]. J Clin Hepatol, 2015, 31(8): 1291-1294. (in Chinese) 王为华. 经皮经肝胆囊穿刺造瘘术联合腹腔镜下胆囊切除术治疗60岁以上重症结石性胆囊炎患者的疗效观察[J]. 临床肝胆病杂志, 2015, 31(8): 1291-1294.
[16] LIU C, ZHANG L. Clinical efficacy of transumbilical single-port laparoscopic cholecystectomy in treatment of acute cholecystitis[J]. J Clin Hepatol, 2015, 31(10): 1678-1681. (in Chinese) 刘超, 张磊. 经脐单孔腹腔镜胆囊切除术治疗急性胆囊炎的效果评价[J]. 临床肝胆病杂志, 2015, 31(10): 1678-1681.
[17] KOMATSU S, TSUKAMOTO T, IWASAKI T, et al. Role of percutaneous transhepatic gallbladder aspiration in the early management of acute cholecystitis[J]. J Dig Dis, 2014, 15(12): 669-675.
[18] CHOK KS, CHU FS, CHEUNG TT, et al. Results of percutaneous transhepatic cholecystostomy for high surgical risk patients with acute cholecystitis[J]. ANZ J Surg, 2010, 80(4): 280-283.
[19] LIU H, FAN MM, CHANG YX, et al. Clincal analysis of cases converted to open surgery during laparoscopic cholecystectomy[J]. Chin J Med Offic, 2016, 44(8): 809-811. (in Chinese) 刘虎, 范明明, 常颜信, 等. 腹腔镜胆囊切除术中转开腹临床分析[J]. 临床军医杂志, 2016, 44(8): 809-811.
[20] CHEN MJ, ZHENG JB. Sequential laparoscopic cholecystectomy compared with simple laparoscopic cholecystectomy in treating eld-erly acute severe cholecystitis[J]. Anhui Med J, 2013, 34(6): 756-758. 陈敏捷, 郑剑波. 经皮经肝胆囊穿刺序贯腹腔镜胆囊切除治疗老年急性重症胆囊炎效果比较[J]. 安徽医学, 2013, 34(6): 756-758.
[21] KWON YJ, AHN BK, PARK HK, et al. What is the optimal time for laparoscopic cholecystectomy in gallbladder empyema?[J]. Surg Endosc, 2013, 27(10): 3776-3780.
[22] LO HC, WANG YC, SU LT, et al. Can early laparoscopic cholecystectomy be the optimal management of cholecystitis with gallbladder perforation? A single institute experience of 74 cases[J]. Surg Endosc, 2012, 26(11): 3301-3306.
[23] YANG HQ, NIU JH, ZHANG SJ, et al. Laparoscopic cholecystectomy following percutaneous transhepatic gallbladder drainage for patients with severe acute cholecystitis[J]. J Abdominal Surg, 2012, 25(2): 100-101. (in Chinese) 杨宏强, 牛建华, 张示杰, 等. 高危急性胆囊炎经PTGD处理后再行腹腔镜胆囊切除术137例[J]. 腹部外科, 2012, 25(2): 100-101.
[24] TAO P, WU XY, ZHANG L. Clinical effect of ultrasound-guided percutaneous transhepatic gallbladder drainage in treatment of acute cholecystitis in elderly patients[J]. J Clin Hepatol, 2016, 32(10): 1929-1931. (in Chinese) 陶平, 吴向阳, 张磊. 超声引导经皮经肝胆囊穿刺引流术治疗老年急性胆囊炎的效果分析[J]. 临床肝胆病杂志, 2016, 32(10): 1929-1931.
[25] JIANG HS, HUANG B, GAN WB. Percutaneous transhepatic gallbladder drainage combined with laparoscopiccholecystectomy in severe acute cho-lecystitis for the elderly patients[J]. Sichuan Med, 2015, 36(7): 999-1001. (in Chinese) 江华山, 黄斌, 甘文斌. 经皮经肝胆囊穿刺引流后择期性腹腔镜胆囊切除治疗老年急性重症胆囊炎的临床观察[J]. 四川医学, 2015, 36(7): 999-1001.
[26] QIU M. Timing of the laparoscopic cholecystectomy after PTGD for acute cholecystitis[D]. Shihezi: Shihezi Univ, 2014. (in Chinese) 邱明. 急性胆囊炎经皮经肝胆囊穿刺引流术后手术时机的选择[D]. 石河子: 石河子大学, 2014.
[27] JIANG QH, WANG AZ, CUI WH. The influence of operation effects of timing of the laparoscopic cholecystectomy after PTGD for acute cholecystitis[J]. Modern Med J, 2015, 43(7): 832-836. (in Chinese) 姜庆贺, 王爱芝, 崔文海. 经肝胆囊穿刺置管引流术后不同手术时机对急性胆囊炎患者手术效果的影响[J]. 现代医学, 2015, 43(7): 832-836.
引证本文:ZHAO HG, LIU K, LIU YH. The most appropriate timing for selective laparoscopic cholecystectomy after percutaneous transhepatic gallbladder drainage in patients with acute severe cholecystitis aged above 60 years[J]. J Clin Hepatol, 2017, 33(4): 705-710. (in Chinese) 赵红光, 刘凯, 刘亚辉. 经皮经肝胆囊穿刺引流术后择期行腹腔镜胆囊切除术治疗60岁以上急性重症胆囊炎患者的最佳时机探讨[J]. 临床肝胆病杂志, 2017, 33(4): 705-710.
(本文编辑:葛 俊)
The most appropriate timing for selective laparoscopic cholecystectomy after percutaneous transhepatic gallbladder drainage in patients with acute severe cholecystitis aged above 60 years
ZHAOHongguang,LIUKai,LIUYahui.
(DepartmentofHepatopancreatobiliarySurgery,TheFirstHospitalofJilinUniversity,Changchun130021,China)
Objective To investigate the clinical effect of selective laparoscopic cholecystectomy (LC) after percutaneous transhepatic gallbladder drainage (PTGD) in the treatment of elderly patients with acute severe cholecystitis, as well as the most appropriate timing for selective operation. Methods A total of 90 patients with acute severe cholecystitis aged above 60 years who were admitted to Department of Hepatobiliary Surgery in The First Hospital of Jilin University from January 2015 to June 2016 were enrolled, and according to the time of selective LC, they were divided into group A (with 2 months), group B (2-4 months), and group C (>4 months), with 30 patients in each group. The clinical effects of PTGD and selective LC were observed. Thet-test was used for comparison of continuous data between two groups, an analysis of variance was used for comparison between three groups, and LSD-ttest was used for comparison between any two groups; the chi-square test was used for comparison of categorical data between groups. Results All the patients underwent successful PTGD, and the time to abdominal pain remission was 2.52±0.76 hours. Body temperature returned to normal with 24-72 hours after surgery, and there were significant improvements in laboratory markers (white blood cell count, neutrophil count, and liver function) (allP<0.05). No patient experienced complications such as bile leakage, hematobilia, pneumothorax, and colon perforation caused by puncture, and there was no case of PTGD after the tube was detached. There were significant differences between the three groups in gallbladder wall thickness before LC(F=8.029,P<0.001), time of operation (F=24.674,P<0.001), intraoperative blood loss (F=12.864,P<0.001), length of hospital stay (F=22.844,P<0.001), rate of conversion to laparotomy (χ2=12.345,P=0.002), and incidence rate of complications (χ2=8.750,P=0.013). Compared with group A, groups B and C had significantly lower gallbladder wall thickness before LC, intraoperative blood loss, length of hospital stay, rate of conversion to laparotomy, and incidence rate of complications (allP<0.05), and group B had significantly lower time of operation, intraoperative blood loss, and length of hospital stay than group C (allP<0.05). Conclusion Selective LC with 2-4 months after PTGD has a marked clinical effect and high safety in the treatment of elderly patients with acute severe cholecystitis.
cholecystitis, acute; drainage; cholecystectomy, laparoscopic; aged
10.3969/j.issn.1001-5256.2017.04.021
2016-10-12;
2016-12-12。
赵红光(1991-),男,主要从事肝胆胰疾病方面的研究。
刘亚辉,电子信箱:liuyahui2008@yeah.net。
R657.41
A
1001-5256(2017)04-0705-06
