妊娠及产褥期溃疡性结肠炎管理
2017-03-18李召风贾爱芹孙琳管丽芳
李召风++贾爱芹++孙琳+++管丽芳

[摘要] 溃疡性结肠炎(UC)在青年女性中发病率越来越高,与生育年龄重叠。UC与妊娠相互影响,其疾病活动会增加患者的不孕率,导致不良妊娠结果等,因此,建议在病情缓解期妊娠。此外,妊娠过程中及产后如何维持疾病缓解、复发后的治疗、妊娠及产褥期UC患者的诊断与检查等问题受到广泛关注。本文就妊娠期患者疾病缓解期的维持、活动期的治疗及产褥期哺乳、用药等问题作一综述,为妊娠前、妊娠中及产褥期UC患者提供参考。
[关键词] 溃疡性结肠炎;妊娠;产褥期;生育率;管理
[中图分类号] R574.62 [文献标识码] A [文章编号] 1673-7210(2017)01(b)-0041-04
Management of ulcerative colitis in pregnancy and puerperium
LI Zhaofeng JIA Ai'qin SUN Lin GUAN Lifang LIU Tongting
Ji'nan Military General Hospital, Shandong Province, Ji'nan 250000, China
[Abstract] The incidence of ulcerative colitis (UC) in young women is higher and higher, overlapping with reproductive age. UC and pregnancy affect each other, active disease may increase the risk of infertility and adverse pregnancy outcomes. Therefore, doctors suggest delaying conception until disease remission. In addition, It has attracted our attention on how to maintain disease remission, treatment after recurrence, diagnose and examination of UC patients in pregnancy and puerperium. This article discusses the maintenance of disease remission, treatment of active UC, and the breast-feed and drugs in puerperium, in order to provide reference for woman before or in pregnancy and puerperium.
[Key words] Ulcerative colitis; Pregnancy; Puerperium; Fertility rate; Management
目前,潰疡性结肠炎(ulcerative colitis,UC)发病率越来越高,且青壮年居多,与生育时期重叠[1]。UC与妊娠相互影响,尤其疾病活动状态对妊娠期患者及胎儿的不良影响更加显著[2]。产褥期爆发重度UC的病例较少见,发病往往病情较重,预后差,死亡率高(约13%)。规范妊娠期UC的治疗对于降低UC患者妊娠风险具有重要意义。
1 溃疡性结肠炎对妊娠的影响
1.1 对生育率影响
就整个育龄期UC女性而言,85%~90%可正常妊娠,缓解期患者生育能力与正常人无明显差异,疾病活动期患者生育能力显著下降[3]。Miller[4]在1986年进行的一项荟萃分析显示,UC患者的正常妊娠率为83%,与健康患者无明显差别。Schulze等[5]在2014年研究显示UC患者缓解期正常妊娠率为84%,活动期患者正常妊娠率为65%。有研究表明,UC患者子女较正常人减少,可能与担心疾病加重病情、遗传后代、心理压力过大等问题恐于妊娠有关[6]。同时,外科手术也会对生育率产生影响,如接受回肠肛门吻合术(ileal pouch anal anastomosis,IPAA)治疗后,生育率显著下降[7],这可能与回肠病变和肠切除术后出现的营养吸收障碍有关。
1.2 溃疡性结肠炎对妊娠结局的影响
UC可导致不良分娩结局,其原因与疾病状态有关。缓解期妊娠患者与普通人群面临相同的妊娠风险[8],但疾病活动期患者胎儿畸胎发生率、流产率、死产率均较正常人升高。近些年一项荟萃分析显示,UC患者可出现早产(OR=1.85,95%CI:1.67~2.05)、生长发育迟缓(OR=1.36,95%CI:1.16~1.60)、先天畸形(OR=1.29, 95%CI:1.05~1.58)、死胎(OR=1.57,95%CI:1.03~2.38)等不良妊娠结局[9]。Broms等[10]对瑞典2006~2010年间1833例UC患者进行回顾性分析发现,UC患者病情复发是导致早产、死胎、生长发育迟缓等不良妊娠的危险因素。因此,建议在UC缓解期妊娠,若妊娠前已存在贫血和营养不良等情况,应先补充铁剂和维生素等改善症状后再考虑妊娠[11]。
2 妊娠对溃疡性结肠炎的影响
妊娠过程中疾病的进程主要取决于妊娠时疾病的活动状态,缓解期妊娠患者与正常女性所面临的妊娠风险无明显差异,而活动期妊娠患者,其胎儿早产、低出生体重、剖腹分娩的风险加重[12]。研究表明,疾病缓解期受孕的患者,约2/3患者整个妊娠过程仍处于缓解期[13];而疾病活动期受孕的患者,即使予以积极的治疗,多数患者妊娠期间疾病仍将处于活动期,甚至少数患者病情会加重甚至暴发[14]。对于妊娠期或产褥期初次发病的UC女性而言,一旦发病,UC病情主要为重型或暴发型,病情极为凶险,需引起高度重视,及时诊治。
3 妊娠期合并潰疡性结肠炎的诊断与检查
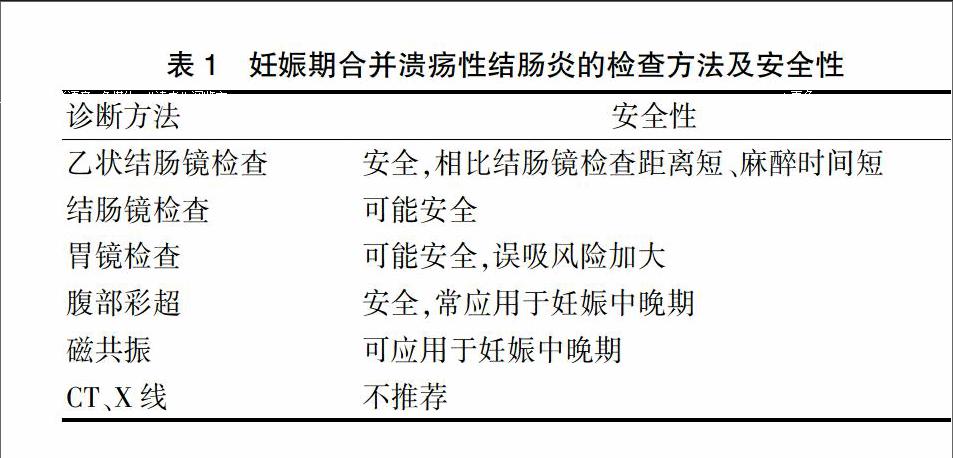
结肠镜检查是确定妊娠期UC是否处于活动期的重要检查手段。Cappell等[15]回顾性分析1986~2007年20例妊娠期行肠镜检查患者,结果显示妊娠期结肠镜检查与不良妊娠结果没有确切关系,同时妊娠3~6个月行结肠镜检查对分娩结果有重要意义,结肠镜检查并不会导致早产或胎儿先天性畸形。近期,Ludvigsson等[16]对3000例行内镜检查的妊娠妇女进行分析,发现妊娠期间内镜检查与早产(ARR,1.16)相关,但不包含SGA(ARR,1.19)、死胎(ARR,1.11)或先天性畸形(ARR,0.90),但其不良妊娠结局发生概率低,应权衡利弊。具体检查方法及安全性见表1。
表1 妊娠期合并溃疡性结肠炎的检查方法及安全性
4 妊娠及产后溃疡性结肠炎的管理
4.1 缓解期溃疡性结肠炎的维持治疗
对于妊娠期UC患者而言,维持缓解及活动期诱导缓解至关重要。根据2015多伦多妊娠期炎症性肠病管理共识意见[17],临床常见维持缓解药物及药物安全等级划分如表2。
5-氨基水杨酸(5-ASA)类药物在妊娠安全用药中属于B级,应用剂量不超过3 g/d时,相对安全[18],临床常应用于妊娠期UC的维持缓解治疗。激素在妊娠期安全用药中属于C级,糖皮质激素常用于中重度UC患者急性期诱导缓解,不作为维持治疗[19]。硫唑嘌呤和6-巯基嘌呤都属于嘌呤类似物,在妊娠安全用药中属于D级,是临床应用于诱导缓解的另一类常见药物[20]。甲氨蝶呤在妊娠安全用药中属于X级,禁止用于妊娠期UC的治疗,因为该药可在体内长期停留,建议停药3~6个月以上考虑妊娠[21]。生物制剂在妊娠用药中属于B级,可以用于孕前及妊娠过程。正在使用生物制剂的患者,建议妊娠期间及产后继续使用[22]。
4.2 妊娠期活动期溃疡性结肠炎治疗
使用5-ASA维持治疗期间出现轻中度疾病复发,建议采用5-ASA口服联合直肠给药尽快诱导缓解[23]。使用5-ASA或巯基嘌呤维持治疗过程中出现疾病复发,建议使用糖皮质激素诱导缓解或直接使用生物制剂。若出现糖皮质激素抵抗性复发时,建议尽快使用生物制剂诱导缓解[24]。妊娠期首选药物治疗,但在紧急并发症发生时要尽早进行外科干预[25-26]。
4.3 分娩方式
妊娠期间疾病缓解后,由于分娩这一应激因素,病情可能复发,甚至暴发。但多数学者认为,在决定分娩方式时,应将UC孕妇视为普通人,但应尽量避免会阴切开术[27]。IPAA术后及活动期肛周及直肠疾病患者应首选剖宫产手术,以降低肠梗阻发生率[28]。
4.4 产褥期管理
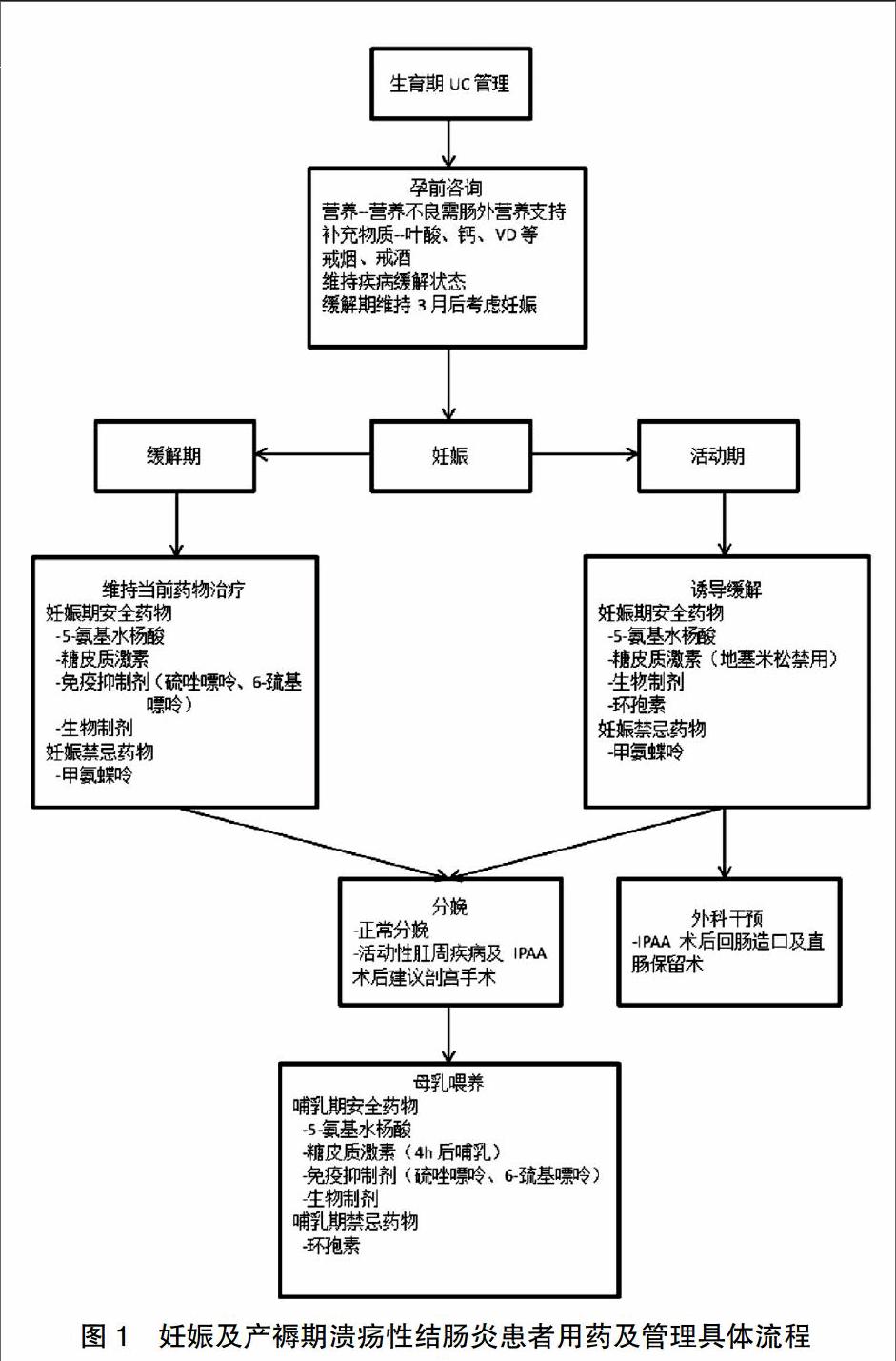
产褥期暴发重度UC的病例较少见,发病往往病情重,预后差,死亡率高。其原因可能与患者妊娠期间及产后情绪焦虑、体内激素水平变化、分娩这一应激因素等有关[29]。另外,2013年韩国一项荟萃分析显示,妊娠及分娩时间与疾病初发及暴发有相关性,尤其1~2个月分娩的患者其发病率最高[30-32]。2005年Kitayama等[31]一项研究显示,除了环孢素类药物,产后大多数药物对患者及婴儿都是安全的。2004年Klement等[33]报道称,母乳喂养可以降低婴儿UC的发生率,这可能与乳汁中泌乳素水平有关[34]。但2005年Kane等[35]的一项研究显示,母乳喂养可以导致疾病复发,甚至暴发(OR=2.2,95%CI:1.2~3.9),这可能与妊娠期间及产后患者未规律服药、恢复吸烟、妊娠及分娩导致体内激素水平变化有关。因此,鼓励妊娠及哺乳期药物维持治疗。同时,妊娠期间对患者要加强心理疏导,加强营养,戒烟戒酒,继续药物治疗。妊娠及产褥期患者用药及管理具体流程见图1。
5 结论
UC病情反复,迁延难愈,多发于生育期,因而需要广泛关注。疾病活动期妊娠会增加患者不孕率,加大不良妊娠风险。因此,孕前、妊娠过程中及产褥期维持病情缓解十分重要。尽管如此,但只要孕前将疾病有效地控制在缓解期,妊娠过程中积极与医师沟通,疾病复发时及时给予适当的治疗措施,UC女性仍能像健康人一样妊娠和生产。
[参考文献]
[1] Abdul Sultan A,West J,Ban L,et al. Adverse Pregnancy Outcomes Among Women with Inflammatory Bowel Disease:A Population-Based Study from England [J]. Inflammatory Bowel Diseases,2016,22(7):1621-1630.
[2] Feagins LA,Kane SV. Caring for Women with Inflammatory Bowel Disease [J]. Gastroenterology Clinics of North America,2016,45(2):303-315.
[3] Winter R,Norgard BM,Friedman S. Treatmant of the Pregnant Patient with Inflammatory Bowel Disease [J]. Inflammatory Bowel Diseases,2016,22(3):733-744.
[4] Miller JP. Inflammatory bowel disease in pregnancy a review [J]. JP Soc Med,1986,79(4):221-225.
[5] Schulze H,Esters P,Dignass A. Review article: the management of Crohn's disease and ulcerative colitis during pregnancy and lactation [J]. Alimentary Pharmacology & Therapeutics,2014,40(9):991-1008.
[6] Puri A,Bharadwaj V,Sachdeva S. Extent of disease is a major outcome predictor in patients with ulcerative colitis and pregnancy [J]. Indian Journal of Gastroenterology,2015,34(2):108-111.
[7] Habal FM,Huang VW. Review article:a decision-making algorithm for the management of pregnancy in the inflam-matory bowel disease patient [J]. Alimentary pharmacology & therapeutics,2012,35(5):501-515.
[8] Boyd HA,Basit S,Harpsoe MC,et al. Inflammatory Bowel Disease and Risk of Adverse Pregnancy Outcomes [J]. PloS One,2015,10(6):1-14.
[9] Pedersen N,Bortoli A,Duricova D,et al. The course of inflammatory bowel disease during pregnancy and postpa-rtum:a prospective European ECCO-EpiCom Study of 209 pregnant women [J]. Alimentary Pharmacology & Therap-eu-tics,2013,38(5):501-512.
[10] Broms G,Granath F,Linder M,et al. Birth outcomes in women with Inflammatory bowel disease:effects of disease activity and drug exposure [J]. Inflamm Bowel Dis,2014, 20(6):1091-1098.
[11] Shand AW,Chen JS,Selby W,et al. Inflammatory bowel disease in pregnancy:a population-based study of prevalence and pregnancy outcomes [J]. BJOG:An International Journal of Obstetrics and Gynaecology,2016,123(11):1862-1870.
[12] Kwan LY,Mahadevan U. Inflammatory bowel disease and pregnancy:an update [J]. Expert Rev Clin Immunol,2010, 6(4):643-657.
[13] Khosla R,Willoughby CP,Jewell DP. Crohn's disease and pregnancy [J]. Gut and liver,1984,25:52-60.
[14] O'Toole A,Nwanne O,Tomlinson T. Inflammatory Bowel Disease Increases Risk of Adverse Pregnancy Outcomes:A Meta-Analysis [J]. Digestive Diseases and Sciences,2015,60(9):2750-2761.
[15] Cappell MS,Fox SR,Gorrepati N. Safety and efficacy of colonoscopy during pregnancy:an analysis of pregnancy outcome in 20 patients [J]. Journal of Reproductive Medicine,2010,55(3-4):115-123.
[16] Ludvigsson JF,Lebwohl B,Ekbom A,et al. Outcomes of Pregnancies for Women Undergoing Endoscopy While They Were Pregnant-a Nationwide Cohort Study [J]. Gastroenterology,2016,10(20):1750-1760.
[17] Nguyen GC,Seow CH,Maxwell C,et al. The Toronto Consensus Statements for the Management of Inflammatory Bowel Disease in Pregnancy [J]. Gastroenterology,2016,150(3):734-757.
[18] Cury DB,Moss AC. Treatment of Crohn's disease in pregnant women:Drug and multidisciplinary approaches [J]. World J Gastroenterol,2014,20(27):8790-8795.
[19] Pinder M,Lummis K,Selinger CP. Managing inflammatory bowel disease in pregnancy:current perspectives [J]. Clinical and Experimental Gastroenterology,2016,9:325-335.
[20] Goel RM,Blaker P,Mentzer A,et al. Optimizing the use of thiopurines in inflammatory bowel disease [J]. Akusherstvo I Ginekologiia,2015,6(3):45-48.
[21] Panaccione R,Ghosh S,Middleton S,et al. Combination therapy with infliximab and azathioprine is superior to monotherapy with either agent in ulcerative colitis [J]. Gastroenterology,2014,146(2):392-400.
[22] Schulze H,Esters P,Dignass A. Editorial:the management of IBD during pregnancy and lactation--author's reply [J]. Alimentary Pharmacology & Therapeutics,2014,40(40):1247-1248.
[23] Jana G,Hashash MD,Sunanda K,et al. Pregnancy and inflammatory bowel disease [J]. Pregnancy And Inflammatory Bowel Disease,2015,11(2):96-102.
[24] Han J,Wang J,Wang JH. Effects of jianpi herbal sup-pository on hemorheology and CD62P in patients with ul-cerative colitis [J]. J Tradit Chin Med,2014,34(2):155-158.
[25] Uchino M,Ikeuchi H,Matsuoka H,et al. Surgery for Severe Ulcerative Colitis during Pregnancy:Report of Two Cases [J]. Case Reports in Gastroenterology,2015,9(1):74-80.
[26] Quddus A,Martin-Perez B,Schoonyoung H,et al. Toxic megacolon during pregnancy in ulcerative colitis:A case report [J]. International Journal of Surgery Case Reports,2015,11:83-86.
[27] Aytac E,Ozuner G,Isik O,et al. Surgical management of patients with ulcerative colitis during pregnancy: maternal and fetal outcomes [J]. Journal of Crohn's & Colitis,2015, 9(1):82-85.
[28] Vincenzo S,Massimo G,Cristina F,et al. Postpartum com-plications in a patient with a previous proctocolectomy and ileo-pouch-anal anastomosis(IPAA)for ulcerative colitis [J]. Case Report,2012,6(2):31-33.
[29] Roomruangwong C,Kanchanatawan B,Sirivichayakul S,et al. Antenatal depression and hematocrit levels as pred-ictors of postpartum depression and anxiety symptoms [J]. Psychiatry Research,2016,238:211-217.
[30] Jung YS,Song CS,Kim ER,et al. Seasonal variation in months of birth and symptom flares in Korean patients with inflammatory bowel disease [J]. Gut and Liver,2013, 7(6):661-667.
[31] Kitayama T,Funayama Y,Fukushima K,et al. Anal function during pregnancy and postpartum after ileal pouch anal anastomosis for ulcerative colitis [J]. Surgery Today,2005, 35(3):211-215.
[32] Moffatt DC,Ilnyckyj A,Bernstein CN. A population-based study of breastfeeding in inflammatory bowel disease:initiation,duration,and effect on disease in the postpartum period [J]. The American Journal of Gastroenterology,2009,104(10):2517-2523.
[33] Klement E,Cohen RV,Boxman J,et al. Breastfeeding and risk of inflammatory bowel disease:a systematic review with meta-analysis [J]. Am J Clin Nutr,2004,80(5):1342-1352 .
[34] Draca S,Levic Z. The possible role of prolactin in the immunopathogenesisof multiple sclerosis [J]. Med Hypo-theses,1996,47(2):89-92 .
[35] Kane S,Lemieux N. The role of breastfeeding in postpartum diseaseactivity in women with inflammatory bowel disease [J]. Am J Gastroenterol,2005,100(1):102-105.
(收稿日期:2016-10-10 本文編辑:程 铭)
