残余羊水量对早期未足月胎膜早破围产结局影响
2017-03-09童重新尹红亚
童重新,刘 静,单 玲,尹红亚
(1.河北省儿童医院妇产科,河北 石家庄 050031;2.河北省妇幼保健院儿保科,河北 石家庄 050031)
·论 著·
残余羊水量对早期未足月胎膜早破围产结局影响
童重新1,刘 静2,单 玲1,尹红亚1
(1.河北省儿童医院妇产科,河北 石家庄 050031;2.河北省妇幼保健院儿保科,河北 石家庄 050031)
目的探讨早期未足月胎膜早破残余羊水量者并发症、分娩方式及早产儿结局。方法225例26~33+6周单胎胎膜早破者分为残余羊水过少A组67例(其中A1组26~31+6周32例,A2组32~33+6周35例)和羊水量正常B组158例(其中B1组26~31+6周78例,B2组32~33+6周80例),对4组并发症、分娩方式及早产儿结局进行比较。结果白细胞计数A1组高于B1、B2组。C反应蛋白A1组高于A2、B1、B2组。潜伏期A1组低于B1、B2组,高于A2组;A2组低于B1、B2组;B1组高于B2组。剖宫产率A1组高于A2、B1、B2组。绒毛膜羊膜炎A1组高于B1、B2,A2高于B2。胎儿窘迫A1组高于A2、B1、B2组。羊水污染B1、B2组低于A1、A2组。产褥感染 A1组高于B1、B2组。差异均有统计学意义(P<0.05)。活婴比例A1组低于B1、B2组;Apgar评分1 min≤7分A1组高于B1、B2组,A2组高于B2组;Apgar评分5 min≤7分、辅助呼吸及宫内感染情况,A1组高于B1、B2组;脐带炎A1、A2组高于B2组;脐动脉pH值A1、A2组低于B1、B2组。其差异具有统计学意义(P<0.05)。AFI≤20 mm中A1、A2组新生儿死亡发生率及剖宫产率差异有统计学意义(P<0.05)。结论对早期未足月胎膜早破残余羊水过少者应严密监测,孕周越小,残余羊水过少对母婴危害越大;相同孕周,残余羊水过少会增加剖宫产率、母亲感染率、早产儿窒息率、死亡发生率,潜伏期缩短;孕26~31+6周合并残余羊水指数≤20 mm,早产儿死亡发生率极高,应慎重选择剖宫产。
胎膜早破;分娩,过早;羊水过少
早期未足月胎膜早破(early preterm premature rupture of membranes,ePPROM)是指<34周的胎膜早破,因孕周小,胎肺不成熟,并发症较多,不良妊娠结局发生率较高,是临床治疗比较棘手的问题。残余羊水指数≤50 mm,诊断为残余羊水过少。未足月胎膜早破后羊水过少发生率为29%,残余羊水量是影响母婴结局的重要因素之一。研究发现,ePPROM剩余羊水过少时,容易出现绒毛膜羊膜炎和胎儿窘迫。如果羊水过少持续10~14 d,胎儿骨骼发育异常、胎体黏连、胎肺发育不全、机械损伤和新生儿死亡发生率明显增加[1]。国外将24~32周胎膜早破称为远离足月胎膜早破。美国妇产科学会2013临床指南建议24~33+6周胎膜早破无禁忌证时采取期待治疗,延长孕周[2]。既往国内<28周胎膜早破仍为难免流产,但随着新生儿救治能力的提高使得部分孕26~28周的早产儿得到救治。姚爱琴[3]将孕26~32周胎膜早破定义为极度早产胎膜早破。此阶段一方面孕周小,早产儿极度不成熟所致高患病率及病死率,另一方面是母体感染等风险使得此期未足月胎膜早破并发残余羊水过少处理更为棘手。本研究总结225例孕26~33+6周胎膜早破残余羊水量对围产结局的影响,旨在为采取最佳处理方式提供参考,报告如下。
1 资料与方法
1.1 一般资料 选择2008年1月—2014年12月在河北省儿童医院妇产科分娩的孕26~33+6周发生胎膜早破单胎孕妇225例,年龄18~36岁,平均 (28.3±5.5)岁。残余羊水量过少组A组:以最后一次B超羊水指数(amniotic fluid index,AFI)≤50 mm,并均经分娩后证实羊水量<300 mL者,共67例;其中A1组26~31+6周32例,A2组32~33+6周35例。羊水量正常组B组:以最后一次B超AFI>50 mm为依据者,分娩后证实羊水量>300 mL者,共158例;其中B1组26~31+6周78例,B2组32~33+6周80例。4组年龄、胎位、孕次等一般资料差异均无统计学意义(P>0.05),具有可比性。见表1。

表1 4组一般资料比较Table 1 Comparison of general information of 4 groups
1.2 方法 所有符合诊断标准孕妇入待产室待产,卧床休息;破膜>12 h或有感染迹象者,静脉滴注广谱抗生素;给予地塞米松促胎肺成熟;如出现宫缩,无感染因素,给予MgSO4抑制宫缩;B超检查2 d/次;胎心监护,1次/d;隔日查血常规+C反应蛋白。
1.3 观察指标 ①分娩前白细胞计数、C反应蛋白;②潜伏期:从破膜到分娩的时间间隔;③剖宫产率;④母亲并发症;⑤胎儿窘迫;⑥早发性新生儿败血症:出生72 h之内败血症;⑦新生儿脐带炎;⑧胎儿宫内感染;⑨早产儿活产率;⑩脐动脉pH值。
1.4 终止妊娠指征[4]出现临床感染征象;胎儿窘迫;宫口开大≥4 cm;孕周≥34周;残余AFI≤20 mm;羊水过少持续10 d以上。
1.5 统计学方法 应用SPASS 19.0统计软件分析数据。计量资料比较分别采用单因素方差分析、q检验和t检验;计数资料比较采用χ2检验。P<0.05为差异有统计学意义。
2 结 果
2.1 4组母体情况比较 白细胞计数A1组高于B1、B2组。C反应蛋白A1组高于A2、B1、B2组。潜伏期A1组低于B1、B2组,高于A2组;A2组低于B1、B2组;B1组高于B2组。剖宫产率A1组高于A2、B1、B2组。绒毛膜羊膜炎A1组高于B1、B2,A2高于B2。胎儿窘迫A1组高于A2、B1、B2组。羊水污染B1、B2组低于A1、A2组。产褥感染 A1组高于B1、B2组。其差异均有统计学意义(P<0.05)。胎盘早剥4组间差异均无统计学意义(P>0.05)。见表2。
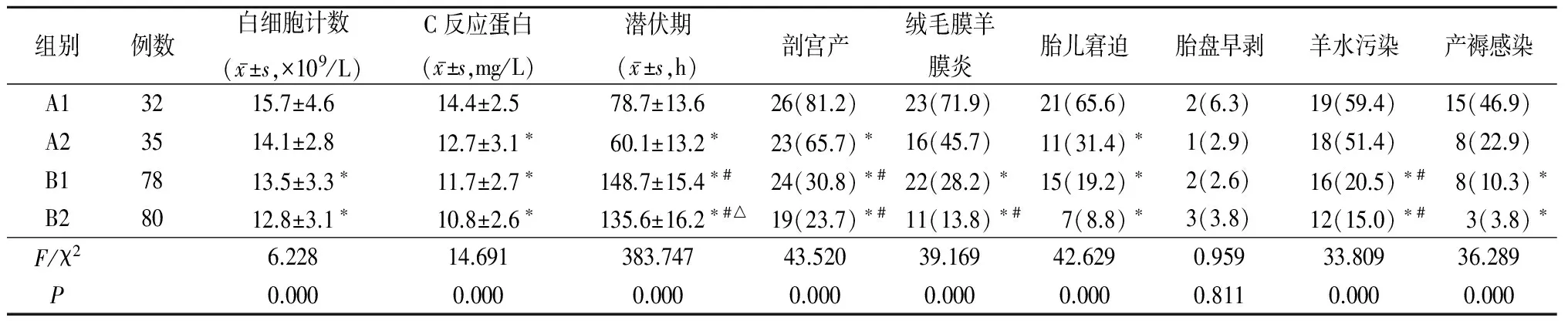
表2 4组母体情况比 较Table 2 Comparison of maternal condition of 4 groups (例数,%)
*P<0.05与A1组比较 #P<0.05与A2组比较 △P<0.05与B1组比较(q检验或χ2检验)
2.2 4组早产儿情况比较 活婴比例A1组低于B1、B2组;Apgar评分1 min≤7分A1组高于B1、B2组,A2组高于B2组;Apgar评分5 min≤7分、辅助呼吸及宫内感染A1组高于B1、B2组;脐带炎A1、A2组高于B2组;脐动脉pH值A1、A2组低于B1、B2组。其差异均有统计学意义(P<0.05)。早发性败血症4组间差异虽然有统计学意义(P<0.05),但两两比较差异无统计学意义(P>0.05)。见表3。

表3 4组早产儿情况比较Table 3 Comparison of premature infant in four groups (例数,%)
*P<0.05与A1组比较 #P<0.05与A2组比较(χ2检验或q检验)
2.3 A1和A2组AFI≤20 mm与AFI>20~50 mm时潜伏期、剖宫产率、新生儿窒息率及新生儿死亡发生率比较 AFI≤20 mm时A1、A2组新生儿死亡发生率和剖宫产率差异均有统计学意义(P<0.05),潜伏期和新生儿窒息率差异均无统计学意义(P>0.05);而AFI>20~50 mm时A1、A2组潜伏期、剖宫产率、新生儿窒息率、新生儿死亡发生率差异均无统计学意义(P>0.05)。见表4。

表4 A1组与A2组比较Table 4 Comparison between group A1 and group A2 (例数,%)
3 讨 论
3.1 残余羊水量对母亲影响 国外将孕24~32周胎膜早破称为远离足月胎膜早破,孕32~36周胎膜早破称为接近足月胎膜早破,处理策略不同。远离足月胎膜早破,在没有感染、胎盘早剥、胎儿窘迫情况下期待治疗。孕32~34周胎膜早破,胎肺成熟或促胎肺成熟后48 h或≥34周终止妊娠[4]。本研究将孕34周之前的胎膜早破称为早期未足月胎膜早破,是相对于孕34周之后胎膜早破而言。早期未足月胎膜早破合并羊水过少一旦发生,将伴随着短暂的潜伏期,潜在围产期感染增加,子宫、脐带压迫,将导致围产期严重的患病率与病死率。本研究孕26~31+6周,残余羊水过少组产前白细胞计数、C反应蛋白均升高。推测母体潜在感染是早期未足月胎膜早破重要原因之一,与伴随的绒毛膜羊膜炎和产褥感染有关。本研究显示残余羊水过少组剖宫产率显著高于与残余羊水正常组,差异有统计学意义; A1组剖宫产率高于A2,B1,B2组,差异亦有统计学意义。表明残余羊水量过少,剖宫产率增加,孕周越小,剖宫产率越高。Kurdoglu等[5]对191例孕24~34周胎膜早破研究发现,AFI<50 mm者由于胎儿窘迫行剖宫产率高达72%。本研究残余羊水过少组剖宫产率高于正常组,第1位原因为胎儿窘迫。羊水过少,致使胎盘血液循环不畅,造成胎儿窘迫,羊水粪染;羊水过少,羊水缓冲胎儿宫内压力的作用显著减弱,而未发育成熟的胎儿对宫缩引起的缺氧抵御能力较低,易引起胎儿宫内窘迫;加之孕周越小,胎肺发育越不成熟,两者叠加,胎儿宫内情况愈不稳定,剖宫产概率增加;羊水过少,易致宫缩不协调,产程异常,剖宫产率增加。本研究显示残余羊水过少A1组绒毛膜羊膜炎、胎儿窘迫、羊水污染、产褥感染率均高于羊水正常B1组,差异有统计学意义。羊水过少,易致羊水污染,胎儿窘迫;羊水过少,抗感染能力下降,绒毛膜羊膜炎、产褥感染概率增加。残余羊水过少组潜伏期明显缩短,与羊水正常组差异有统计学意义。表明残余羊水量与潜伏期相关。Ekin等[6]研究显示,大孕周、羊水过少、双胎是短潜伏期的独立危险因素;潜伏期延长,绒毛膜羊膜炎、胎盘早剥概率增加。本研究显示大孕周、羊水过少伴随短潜伏期;残余羊水量越少,潜伏期越短。表明羊水污染和羊水量多少有关,与孕周无关。Vermillion等[7]研究也显示孕24~32周未足月胎膜早破残余AFI<50 mm伴随着围产期感染及短潜伏期分娩高风险。本研究显示残余羊水过少不增加胎盘早剥发生率,而 Coolen等[8]结论相反,其研究认为去除混杂因素如分娩孕周、产次、临床表现、产前抗生素及激素应用,残余羊水过少仅与潜伏期缩短相关,不影响母婴感染患病率;残余羊水量过少增加剖宫产、母亲感染、胎儿窘迫、早产儿死亡发生率;残余羊水过少与分娩方式、产后子宫内膜炎、母亲住院时间、胎儿窘迫、新生儿患病率及病死率不相关。因此,不作为期待治疗考虑因素及引产指征。本研究认为残余羊水量应作为期待治疗时限考虑因素。
3.2 残余羊水量对早产儿影响 本研究显示早产儿活产率在羊水过少组为79.1%(53/67),羊水正常组为98.7%(156/158),二者对比差异有统计学意义;其中活婴A1组低于B1、B2组,差异有显著统计学意义。表明孕周、残余羊水量与早产儿存活率有关。推测孕周越小,胎儿肺发育越不成熟;羊水过少,可导致胎肺发育不全;残余羊水量越少,围产儿病死率越高。王静娴等[9]对561例28~33+6周胎膜早破患者行多因素回归分析,研究结论为AFI<40 mm及破膜孕周为新生儿死亡的影响因素,AFI<40 mm是新生儿窒息的影响因素。本研究显示A1和B1组1 min、5 min Apgar评分及辅助呼吸差异亦有统计学意义;同一孕周,残余羊水过少,胎儿窘迫概率越高,并导致围产不良结局。推测早产儿窒息与孕周、残余羊水量相关。王艳萍等[10]对256例28~34周胎膜早破研究发现,AFI≤50 mm剖宫产率、胎儿窘迫、羊水污染、胎儿宫内感染、新生儿窒息发生率均高于AFI>50 mm组,差异有统计学意义。本研究显示A1组胎儿宫内感染、新生儿脐带炎概率增高。羊水具有润滑及缓冲作用,未足月胎膜早破,持续羊水丢失,羊水量减少,影响胎盘的血液循环,使脐带受压易发生胎儿窘迫;羊水量越少,越易造成胎儿娩出时干涩困难,死胎死产、新生儿窒息死亡概率增加。Yu等[11]研究发现破膜孕周、短潜伏期与新生儿患病率及死亡发生率高度相关。本研究认为残余羊水过少、孕周是新生儿窒息、死亡的影响因素,尤其是残余AFI≤20 mm,早产儿死亡发生率极高。
3.3 残余羊水量对早期未足月胎膜早破处理的影响 国内建议孕24~31+6周胎膜早破期待治疗过程中羊水过少持续10 d以上需要终止妊娠[4]。本研究以AFI<50 mm作为羊水过少诊断依据。张秀云[12]研究653例孕28~36周胎膜早破孕妇,发现以AFI=40 mm为截断值,灵敏度77.6%,特异度75.4%,AFI≤40 mm,是新生儿窒息的唯一影响因素,建议AFI>40 mm可保守治疗,AFI≤40 mm则人工终止妊娠。王静娴等[9]研究也认为可将AFI≤40 mm 作为终止妊娠的指标。徐元春等[13]建议未足月胎膜早破AFI≤50 mm者,如为胎位不正( 臀位或横位) 应剖宫产结束分娩,余可在严密监测下阴道试产。杜鹃等[14]认为25~28 孕周时,新生儿并发症多且严重,成活率较低,阴道分娩是理想的选择,28~32孕周适当放宽剖宫产指征。本研究认为分娩方式的选择需结合孕周、残余羊水量、母婴儿状况决定,孕26~31+6周合并残余AFI≤20 mm,新生儿死亡发生率极高,应慎重选择剖宫产。表明残余羊水量过少者潜伏期缩短,应抓紧使用糖皮质激素促进胎肺成熟,减少围产期不良结局。
总之,未足月胎膜早破严密监测羊水残余量对正确选择分娩方式、降低母儿发病率及新生儿死亡发生率意义重大。破膜后残余羊水量多少需积极终止妊娠截断值的确定还需要大样本、多中心联合研究。
[1] ACOG Committee on Practice Bulletins-Obstetrics. ACOG Practice Bulletin No.80: Premature rupture of membranes.Clinical management guidelines for obstetrician-gynecologists[J]. Obstet Gynecol,2007,109(4):1007-1019.
[2] ACOG Practice Bulletin No. 139:premature rupture of membranes.The American College of Obstetricians and Gynecologists[J]. Obstet Gynecol,2013,115:918-928.
[3] 姚爱琴.极度早产胎膜早破的危险因素及其妊娠结局的初步研究[J].现代实用医学,2014,26(3):256-258.
[4] 白宇翔,漆洪波.妊娠34周前胎膜早破的处理[J].中国实用妇科与产科杂志,2014,30(6):410-413.
[5] Kurdoglu M, Kolusari A, Adali E,et al. Does residual amniotic fluid after preterm premature rupture of membranes have an effect on perinatal outcomes? 12 years experience of a tertiary care center[J]. Arch Obstet Gynecot,2010,281(4):601-607.
[6] Ekin A, Gezer C, Taner CE,et al. Risk factors and perinatal outcomes associated with latency in preterm premature rupture of membranes between 24 and 34 weeks of gestation[J]. Arch Gynecol Obstet,2014,290(3):449-455.
[7] Vermillion ST,Kooba AM,Soper DE. Amniotic fluid index values after preterm premature rupture of the membranes and subsequent perinatal infection[J]. Am J Obstet Gynecol,2000,183(2):271-276.
[8] Coolen J,Kabayashi K, Wong K,et al. Influence of oligohydramnios on preterm premature rupture of the membranes at 30 to 36 weeks' gestation[J]. J Obstet Gynaecol Can,2010,32(11):1030-1034.
[9] 王静娴,苏赞妍,潘成荣.未足月胎膜早破后残余羊水指数对妊娠结局和新生儿的影响[J].白求恩医学杂志,2014,12(3):236-237.
[10] 王艳萍,田丽娟.未足月胎膜早破孕妇羊水过少对妊娠结局的影响[J].中华实用诊断及治疗杂志,2014,28(1):100-101.
[11] Yu H, Wang X, Gao H,et al. Perinatal outcomes of pregnancies complicated by preterm premature rupture of the membranes before 34 weeks of gestation in a tertiary center in China:a retrospective review[J]. Biosci Trends,2015,9(1):35-41.
[12] 张秀云.未足月胎儿胎膜早破后残余羊水指数对妊娠结局和新生儿的影响[J].临床儿科杂志,2014,32(1):19-22.
[13] 徐元春,王细先,康程,等.未足月胎膜早破残余羊水量过少81例临床分析[J].中国优生与遗传杂志,2012,20(3):69-70,82.
[14] 杜鹃,王雪娇.未足月胎膜早破治疗进展[J].中国计划生育和妇产科,2015,7(4):3-6.
(本文编辑:刘斯静)
The influence of residual oligohydramnios on perinatal outcome of early preterm premature rupture of membranes
TONG Chong-xin1, LIU Jing2, SHAN Ling1, YIN Hong-ya1
(1.DepartmentofObstetricsandGynecology,HebeiChildren'sHospital,Shijiazhuang050031,Chian2.DepartmentofHebeiBeaufoyMaternityandChildCare,Shijiazhuang050031,Chian)
Objective To explore the complication, delivery model of pregnancy and the outcomes of premature infant on early preterm premature rupture with residue oligohydramnios. Methods Two hundred and twenty-five cases of 26-33+6weeks of singletons pregnant women were divided into four groups. Sixty-seven cases of residue oligohydramnios were group A, including group A1 which is 32 cases of 26-31+6weeks of singletons pregnant women and group A2 which is 35 cases of 32-33+6weeks of singletons pregnant women . One hundred and fifty-eight cases of normal amniotic fluid were group B, including group B1 which is 78 cases of 26-31+6weeks of singletons pregnant women and Group B2 which is 80 cases of 32-33+6weeks of singletons pregnant women .The indexes such as the complication, delivery model of pregnant and the outcomes of premature infant were compared in the four groups. Results In group A1,WBC count is above than that in group B1 and B2; C-reactive protein is higher than that in group A2, B1, B2. Latency period is lower in group A1 than that in group B1 and B2, but is higher than that in group A2, also it is lower in group A2 than group B1 and B2, it is higher in group B1 than that in group B2. The cesarean section rate of group A1 is higher than group A2, B1, B2. Chorioamnionitis is higher in group A1 than in group B1 and B2, it is also higher in group A2 than that in group B2. Fetal distress is above in group A1 than in group A2, B1, B2. Amniotic fluid contamination is lower in group B1 and B2 than that in group A1 and A2. Puerperal infection is higher in group A1 than that in group B1 and B2. There are significant difference in these groups(P<0.05). The premature infants asphyxia rate is lower and the death rate is higher in group A1 than that in group B1 and B2. Apgar score 1 min≤7 is higher in group A1 than that in group B1 and B2, also it is higher in group A2 than group B2. Apgar score 5 min≤7, assisted respiration and intrauterine infection are all higher in group A1 than that in group B1 and B2. Umbilical cord inflammation in group A1 and A2 is above than that in group B2. The pH of umbilical arterial is lower in group A1 and A2 than that in group B1 and B2. There are significant difference in all these groups(P<0.05). In group A1 and A2 with AFI≤20 mm, neonatal mortality and cesarean section rate are significantly different in the two groups(P<0.05). Conclusion Patients of residue oligohydramnios with early preterm premature rupture of membranes should be monitored closely,the smaller of the gestational age, the greater damage of the mother and children. In the same gestational age, residual oligohydramnios were associations with the higher rate of the cesarean section, maternal infection, premature infants asphyxia and mortality; also were associations with the shorter of latency period. The mortality of premature infants of 26-31+6weeks with AFI≤20 mm is more higher, the cesarean delivery should be choosed carefully.
fetal membranes, premature rupture; obstetric labor, premature; oligohydramnios
2016-09-21;
2016-10-25
河北省医学科学研究重点课题(20160421)
童重新(1975-),女,河北行唐人,河北省儿童医院副主任医师,医学硕士,从事产科疾病诊治研究。
R714.21
A
1007-3205(2017)02-159-05
10.3969/j.issn.1007-3205.2017.02.09
