血浆抵抗素水平与心房颤动关系的临床研究
2016-11-11王梅香殷屹岗陈各才
王梅香 殷屹岗 陈各才
血浆抵抗素水平与心房颤动关系的临床研究
王梅香殷屹岗陈各才
目的通过测定血浆抵抗素的水平,研究其在孤立性心房颤动(房颤)的发生与维持中的作用;同时分析影响其水平的相关因素及房颤的风险因素。方法 研究对象为2014年6月至12月因心悸等不适就诊我院心内科的患者140例,其中试验组为房颤人群,分为孤立性房颤(60例)和房颤合并高血压(55例);根据发病时间不同,孤立性房颤又分为阵发性与持续性房颤,各30例。正常对照组为正常人群,共25例。使用单因素方差分析比较房颤人群与正常人群血浆抵抗素水平的差异。用Pearson及多重线性回归法分析影响房颤患者抵抗素水平的相关因素。用Logistic回归分析影响房颤的风险因素。结果① 超敏C反应蛋白(hs-CRP)及血浆抵抗素水平:所有房颤组的水平均高于对照组,其中孤立性房颤组低于房颤合并高血压组;阵发性房颤组低于持续性房颤组。② Pearson相关分析:血浆抵抗素水平与hs-CRP水平、左房内径大小及收缩压均呈正相关(分别为r=0.530,P=0.000;r=0.265,P=0.004;r=0.364,P=0.000)。多重线性回归分析进一步显示收缩压(SBP)、hs-CRP水平与血浆抵抗素的水平存在线性关系:Y=-2.172+0.089 SBP+1.347 hs-CRP(R2=0.307,P<0.05)。③ Logistic回归分析表明血浆抵抗素水平、hs-CRP水平均被纳入回归方程,且OR值均>1。结论① 血浆抵抗素水平孤立性房颤组明显高于对照组,其中又以持续性房颤组增高为著,表明抵抗素与房颤的发生、节律的维持相关。② 血浆抵抗素水平与hs-CRP的水平呈正相关,间接表明房颤的发生可能与抵抗素具有某种炎性特质相关,提示抵抗素可引起炎症反应并和炎症介质一起参与了房颤发生、维持。③ 血浆抵抗素水平在房颤合并高血压患者中升高明显,且具有协同效应,提示抵抗素也许具有独立表达高血压与房颤疾病的潜质。同时本研究也证实了高血压为房颤的风险因素,可推测抵抗素通过高血压影响房颤。
心房颤动;血浆抵抗素;炎症
抵抗素是一种分泌型的蛋白,且半胱氨酸残基含量较高。人的抵抗素主要由单核巨噬细胞分泌而来。研究发现动脉粥样硬化、冠心病及高血压患者血浆的抵抗素普遍升高[1],并推测其可能与胰岛素的抵抗有关,认为抵抗素也许是联系炎症与胰岛素抵抗的纽带,从而参与冠心病、高血压等疾病的发生、发展[2]。目前,众多研究证实了抵抗素与炎症存在关系,且与超敏C反应蛋白(hs-CRP)的水平呈正性相关[3]。最新2016年ESC房颤管理指南对房颤进行了临床分类,包括继发于结构性心脏病的房颤、局灶性房颤、多基因房颤、术后房颤、二尖瓣狭窄和人工心脏瓣膜相关房颤、运动员房颤和单基因房颤等类型。本研究试验组为孤立性房颤患者,是指房颤发生在无基础心脏病变的中青年,且临床相关检查未发现心房明显扩大、心功能不全及相关的心外疾病。目前关于房颤的具体机制仍不确定。Anné等[4]报道房颤的发生及维持与心房内径增大导致结构重构和电重构有关联,主要机制包括心房临界物质增多,心房扩大导致机械-电反馈,细胞外基质变性、纤维化,神经内分泌改变等。近年来,众多研究都支持炎症作用于房颤的发生与维持,但多数是hs-CRP水平与房颤关系的相关报道[5]。本研究分析了抵抗素直接通过其炎性特质及其对相关风险因素的间接作用参与房颤的发生及发展。
1 资料与方法
1.1一般资料
2014年6月至12月因心悸就诊于泰州市人民医院心内科的患者,共入选140例(男72/女68),平均(54.45±6.10)岁。其中25例为正常对照组(男12/女13),平均(55.28±7.28)岁;孤立性房颤组60例(男32/女28),平均(53.42±5.00)岁,其中阵发性房颤及持续性房颤患者各30例;另外55例为房颤合并高血压组(男28/女27),平均(55.20±6.55)岁。
1.2方法
体质量指数=体质量(kg)/身高2(m2);连续测量两次不同时间的肱动脉血压水平,取其平均值;采用酶法(日立生化分析仪)测定空腹静脉血糖、低密度脂蛋白、三酰甘油、高密度脂蛋白及总胆固醇。左房内径通过二维超声在胸骨旁的左室长轴切面测定。hs-CRP水平采用免疫放射比浊法测定。
血浆抵抗素水平的测定:采取空腹静脉血,通过离心( 3 000 r/min,离心15 min)收集血浆0.5 mL,并置于-80℃的冰箱中保存待检,所有标本保存未超过6个月;用人抵抗素定量试剂盒(大连泛邦化工技术开发有限公司)采用ELISA法测定血浆抵抗素的浓度:① 向预先包被抵抗素抗体的包被微孔中依次加入标本、标准品、HRP标记的检测抗体,经过温育及彻底洗涤;② 用底物TMB显色,TMB在过氧化物酶的催化下转化成蓝色,并在酸作用下最终转换成黄色;其颜色的深浅和样品中抵抗素浓度呈正相关;③ 用酶标仪在450 nm波长下测定吸光度;④ 计算机绘出标准品的标准曲线,根据样品的吸光度读出相应的浓度,再乘以稀释倍数(×5),即为所测样品的实际浓度。
1.3统计学分析

2 结果
2.1血浆抵抗素及hs-CRP的水平比较
血浆抵抗素及hs-CRP水平房颤组均高于正常对照组(P<0.05,P<0.01);持续性房颤组高于阵发性房颤组(P<0.05);而且房颤合并高血压组高于孤立性房颤组(P<0.05,P<0.01),差异均有统计学意义。见表1。
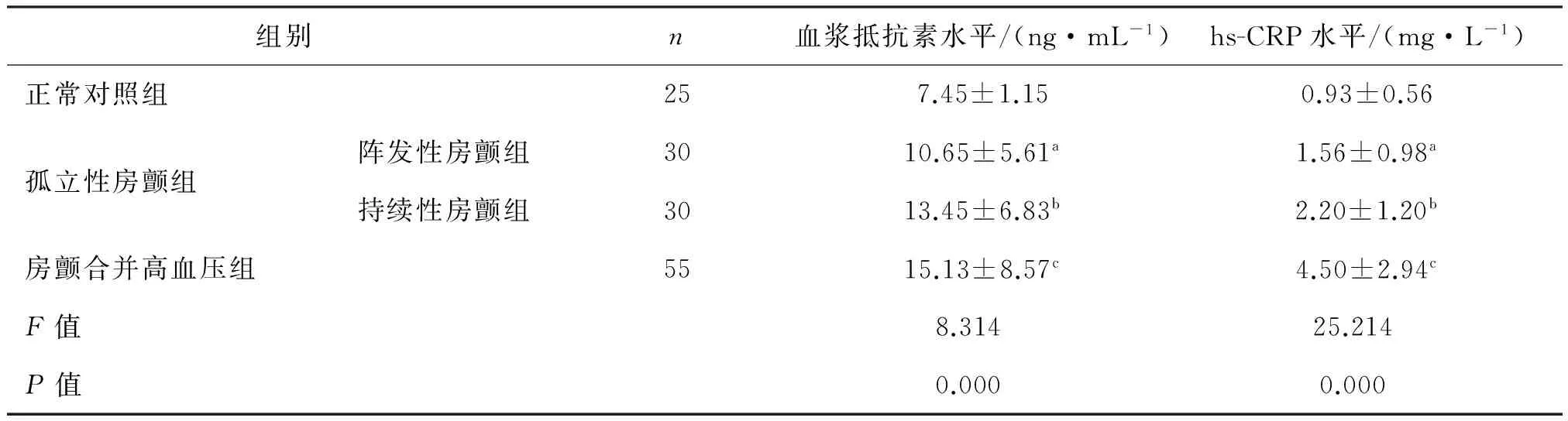
表1 正常对照组、孤立性房颤组与房颤合并高血压组血浆抵抗素及hs-CRP水平的比较
a:与正常对照组相比,P<0.01;b:与阵发性房颤组相比,P<0.05;c:与孤立性房颤组相比,P<0.05
2.2Pearson相关分析
将血浆抵抗素水平分别与hs-CRP水平、左房内径及收缩压进行相关性分析,结果分别为r=0.530,P=0.000;r=0.265,P=0.004;r=0.364,P=0.000,均呈正相关。见图1。
2.3多重线性回归分析
血浆抵抗素水平与收缩压(SBP)、hs-CRP水平呈线性关系:Y=-2.172+0.089 SBP+1.347 hs-CRP(R2=0.307,P<0.05)。见表2。
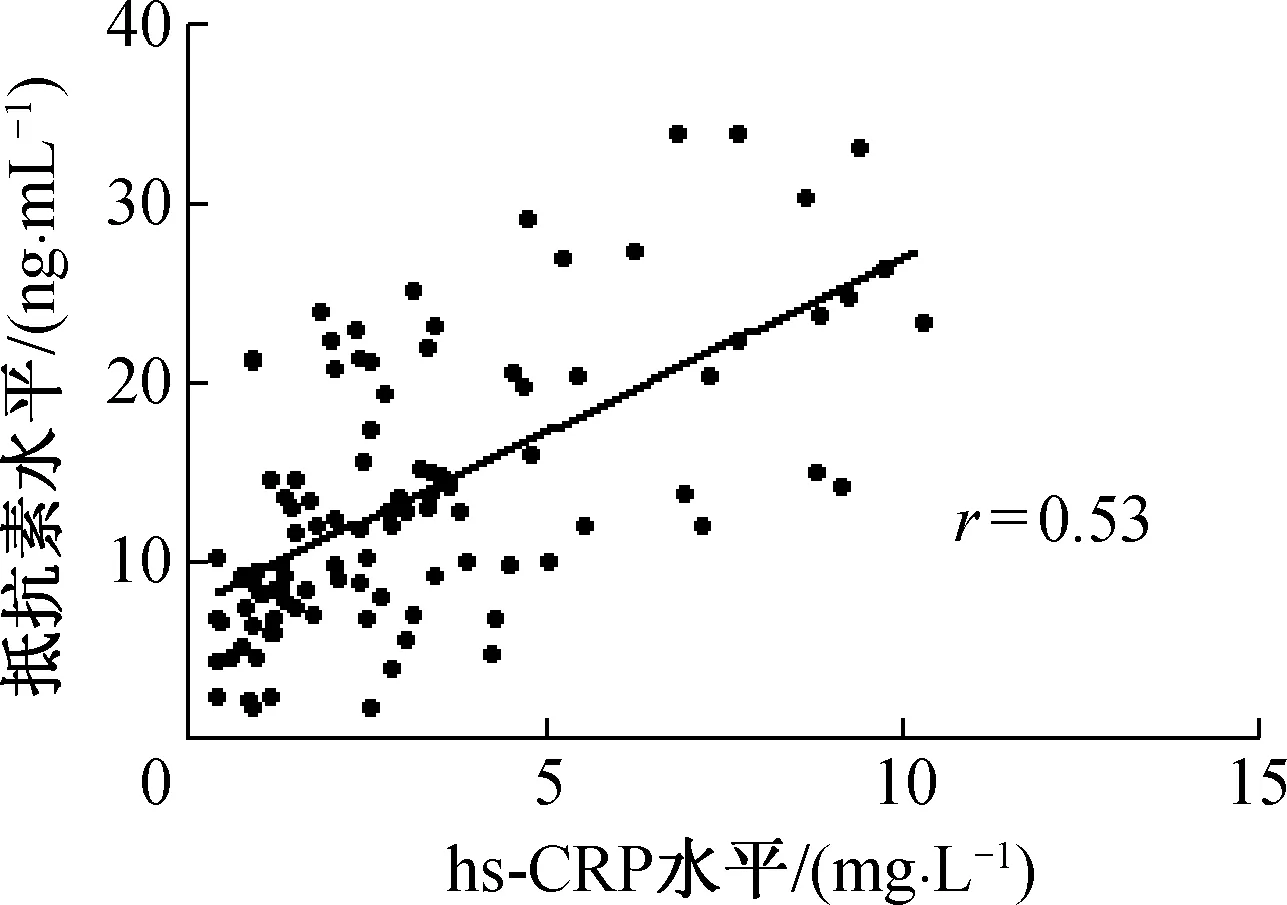
图1 血浆抵抗素与hs-CRP水平的相关性

变量偏回归系数标准误标准偏回归系数t值P值常数项-2.1725.390—-0.4030.688收缩压0.0890.0440.1782.0220.046

续表
2.4二分类Logistic分析(向前逐步回归法)
以房颤的有无为应变量,一般测量指标(年龄、性别、胆固醇、血压、血糖等)、左房内径、hs-CRP及血浆抵抗素水平为自变量。结果显示SBP、左房内径、血浆抵抗素及hs-CRP水平进入回归模型,且均有统计学意义(P<0.05)。而且结果显示它们的OR值均>1。

表3 以房颤有无为应变量的Logistic回归分析
3 讨论
本研究显示,血浆抵抗素水平在持续性房颤患者中高于阵发性房颤患者,且高于正常人群,提示抵抗素与房颤节律的维持及其发生存在关系,但目前尚无相关的大量临床研究直接报道,有待继续追踪证实。另外,本研究还显示hs-CRP存在于孤立性房颤组(持续性与阵发性)的浓度均高于正常对照组,同时持续性房颤患者的浓度高于阵发性房颤患者,考虑炎症反应与房颤的发生和节律维持相关,结果与Hagiwara[6]及Chung等[7]的研究相符。
研究还显示,血浆抵抗素水平与收缩压呈正相关,且多重线性回归也显示抵抗素水平与收缩压存在线性关系,提示高血压与抵抗素水平存在着密切的联系。这与Takata等[8]及Zhang等[9]的研究相一致。房颤合并高血压患者的血浆抵抗素水平较单纯房颤患者的明显升高,且具有协同效应,提示高血压与房颤这两者可能相互独立作用于血浆的抵抗素水平,从而推测抵抗素水平可能具有独立表达高血压与房颤这两种疾病的潜质。同时,本研究也证实了高血压为房颤的风险因素,可推测抵抗素通过高血压导致房颤的发生。
研究中两种线性关系分析表明血浆抵抗素水平与hs-CRP水平、左房内径呈正相关,间接表明房颤的发生可能与抵抗素具有炎症性质相关,提示抵抗素可能引起炎症反应并和炎症介质一起参与了房颤的发生、维持。并且血浆抵抗素水平与hs-CRP水平都被纳入了Logistic回归模型,且两者的OR值均>1,提示两者均是房颤的重要风险因素,说明两者增高的患者发生房颤的概率高于正常人。这与Rienstra等[10]及Gungor等[11]的发现相符。
综上,本研究发现抵抗素可以作为新的炎症介质之一,它通过与其他各种炎性因子(氧化亚氮、白介素、缓激肽及肿瘤坏死因子等)共同参与NF-κB信号通路及其自身mRNA的表达,进入了系统性炎症反应的恶性循环,导致心房的内径变大和电紊乱,从而促进房颤的发生与发展;也可以通过影响房颤的多个风险因素(高血压、肥胖、冠心病及心衰等),间接参与房颤的发生与维持。所以推测抵抗素会在不久的将来成为房颤的早期预测因子,联合动态监测病情的发展与转归,进而改善患者预后。
[1] Muse ED,Feldman DI,Blaha MJ,et al.The association of resistin with cardiovascular disease in the Multi-Ethnic Study of Atherosclerosis[J].Atherosclerosis, 2015, 239(1):101-108.
[2] Park HK, Qatanani M, Briggs ER, et al. Inflammatory induction of human resistin causes insulin resistance in endotoxemic mice[J].Diabetes, 2011,60(3):775-783.
[3] Aksoy DY, Cinar N, Harmanci A,, et al. Serum resistin and high sensitive CRP levels in patients with subclinical hypothyroidism before and after L-thyroxine therapy[J]. Med Sci Monit, 2013,19:210-215.[4] Anné W, Willems R, Holemans P, et al. Self-terminating AF depends on electrical remodeling while persistent AF depends on additional structuralchanges in a rapid atrially paced sheep model[J]. J Mol Cell Cardiol, 2007,43(2):148-158.
[5] Issac TT, Dokainish H, Lakkis NM. Role of inflammation in initiation and perpetuation of atrial fibrillation: a systematic review of the published data[J]. J Am Coll Cardiol, 2007,20,50(21):2021-2028.
[6] Hagiwara N.Inflammation and atrial fibrillation[J].Circ J,2010,74(2):246-247.
[7] Chung MK, Martin DO, Sprecher D,et al. C-reactive protein elebation in patients with atrial arrhythmias:inflammatory mechanisms and persistence of atrial fibrillation[J]. Circulation,2001,104(24): 2886-2891.
[8] Takata Y,Osawa H,Kurata M,et al.Hyperresistinemia is associated with coexistence of hypertension and type 2 diabetes[J].Hypertension,2008,51(2):534-539.
[9] Zhang L, Curhan GC, Forman JP. Plasma resistin levels associate with risk for hypertension among nondiabetic women[J]. J Am Soc Nephrol,2010,21(7):1185-1191.
[10] Rienstra M, Sun JX, Lubitz SA, et al.Plasma resistin, adiponectin, and risk of incident atrial fibrillation: the Framingham Offspring Study[J]. Am Heart J, 2012,163(1):119-124.
[11] Gungor H, Ayik MF, Kirilmaz B,et al. Serum resistin level:as a predictor of atrial fibrillation after coronary artery bypass graft surgery[J].Coron Artery Dis, 2011,22(7):484-490.
Clinical study on the relationship between plasma resistin level and atrial fibrillation
WangMei-xiang,YinYi-gang,ChenGe-cai
(Department of Cardiology, Jiangsu Taizhou People’s Hospital, Taizhou Jiangsu 225300, China)
ObjectiveBy measuring the level of plasma resistin, to study its roles in the occurrence and maintenance of lone atrial fibrillation(LAF), and analyze the related influential factors of plasma resistin level and risk factors of AF. MethodsResearch objects were 140 patients consulting in the department of cardiology of our hospital because of palpitation from June to December in 2014. The experimental group consisted of AF patients who were classified into patients with LAF(60 cases) and those with AF complicating hypertension(55 cases), respectively. The LAF cases were further divided into paroxysmal AF group and persistent AF group, each with 30 cases. In the control group were normal people(25 cases). The difference of plasma resistin level was analyzed between AF patients and normal people by one-way abalysis of variance, and its related influential factors for AF patients were analyzed in methods of Pearson correlation analysis and multiple linear regression. Logistic regression was applied in analyzing risk factors of AF. Results(i) In terms of high sensitive C reactive protein( hs-CRP) and plasma resistin level, the levels of AF group were all higher than those of control group; among the AF patients, the levels of LAF group were lower than those of AF complicating hypertension group and the levels of paroxysmal AF group were lower than those of persistent AF group. (ii) Pearson correlation analysis showed that plasma resistin level was positively correlated with hs-CRP level(r=0.530,P=0.000), left atrial diameter(r=0.265,P=0.004) and systolic blood pressure(SBP)(r=0.364,P=0.000). Multiple linear regression analysis further revealed that there was a linear relationship among SBP, hs-CRP and plasma vesistin levels:Y=-2.172+0.089 SBP+1.347 hs-CRP(R2=0.307,P<0.05). (iii) Logistic regression analysis indicated that plasma resistin and hs-CRP levels were both enrolled into the regression equation, withOR>1. Conclusion(i) The level of plasma resistin in LAF group was significantly higher than that in control group, especially the cases in persistent AF group, which indicated that resistin participated in the occurrence and maintenance of AF. (ii) Plasma resistin level was positively correlated with hs-CRP level. It implied that the occurrence of AF may be related with some inflammatory characteristics of resistin, which suggested that resistin could give rise to inflammatory reaction and participate in the occurrence and maintenance of AF with inflammatory mediators. (iii) Plasma resistin level increased significantly in AF patients complicating hypertension and showed synergistic effect, which suggested possible potentiality of resistin in expressing hypertension and AF independently. Meanwhile, the study also demonstates that hypertension is a risk factor of AF. It might be suspected that resistin can impact on AF via hypertension.
atrial fibrillation; plasma resistin; inflammation
225300 江苏 泰州,泰州市人民医院心内科
王梅香,住院医师,主要从事心脏电生理方向的研究,E-mail:569896951@qq.com
10.13308/j.issn.2095-9354.2016.05.013
2016-09-07)(本文编辑:郭欣)
R541.7
A
2095-9354(2016)05-0359-04
