Characteristics and visual outcomes of open globe injuries in children of amblyogenic age in Hong Kong
2016-11-09YolyYeukYingFongLauHingWaiHenryWilsonWaiKuenYipAlvinLerrmannYoung
Yoly Yeuk Ying Fong, Lau Hing Wai Henry,Wilson Wai Kuen Yip, Alvin Lerrmann Young
Characteristics and visual outcomes of open globe injuries in children of amblyogenic age in Hong Kong
Yoly Yeuk Ying Fong, Lau Hing Wai Henry,Wilson Wai Kuen Yip, Alvin Lerrmann Young
Department of Ophthalmology & Visual Sciences, Prince of Wales Hospital,The Chinese University of Hong Kong, Hong Kong 999077, China
方法:回顾性研究并分析了2005/2015年所有0~8岁眼球开放性创伤儿童的病历记录,对其眼部特征及所进行的初次及其后手术、手术前后的最佳矫正视力及并发症进行分析。
结果:开放性眼球创伤7例(男2例,女5例)中,年龄的中位数为5岁。全部是眼球穿破伤(100%)。其中4例(57%)手术后视力有进步。最终视力:手动(1例患者),20/200~20/50(4例患者),20/40或以上(2例患者)。
结论:在香港,眼球开放性创伤在儿童群组相对罕见。眼球受伤破裂的位置和严重性,及时手术治疗恢复眼球的完整性和对弱视的积极治疗等是预后良好视力的关键因素。
•AIM: To evaluate the demographics, characteristics and visual outcomes of open globe injuries in children of amblyogenic age in Hong Kong.
•METHODS: All medical records of children aged between 0 to 8y old who sustained open globe injuries between Jan. 1st, 2005 and Jan. 1st, 2015 were reviewed retrospectively. The demographics, clinical features (laterality, etiology and zone of injury, other associated ocular injuries), type of primary and secondary operations performed, preoperative and postoperative best spectacle corrected visual acuity (BSCVA) complications were collected and analysed.
•RESULTS: A total of 7 cases, 2 males and 5 females were identified. The median age of presentation was 5 years old. All suffered from penetrating injuries (100%). Four cases (57%) had improvement of visual acuity compared with preoperative visual acuity. Final visual acuity was hand movement in one (14%) patient, 20/200-20/50 in four (57%) patients, and 20/40 or better in two (29%) patients.
•CONCLUSION: There is a relative low rate of open globe injuries in young children in Hong Kong. Good visual outcomes may be obtained depending on the location and severity of the open globe injury together with prompt surgical management to restore the integrity of the globe and aggressive management of amblyopia.
open globe injuries; rupture globe; paediatric ocular injury
INTRODUCTION
Open globe eye injury is defined as full-thickness wound of the eyeball by the Birmingham Eye Trauma Terminology. It can be classified into rupture or laceration. Rupture is an injury caused by a blunt object whereas a sharp object causes laceration. Laceration injuries can be subdivided into penetrating wounds where there is an entrance wound or perforating wound where there is presence of an entrance and an exit wound[1-2]. Pattern and etiology of open globe injury is different among different age populations[3].
Ocular trauma is an important cause of ocular morbidity in children[4]. Open globe injuries in children occur mostly in preschool boys (66%), and 37.8% occur among those in the 3 to 6 years age group[5]. Children aged 8 years or younger who suffered from open globe injury may have poor long term visual outcomes as they have a risk of developing amblyopia[6-7]. In this retrospective study, we studied the characteristics and outcomes of open globe injuries in children aged 0 to 8 years old at a tertiary eye care centre in Hong Kong.
SUBJECTS AND METHODS
A retrospective review ofthe record notes of consecutive paediatric patients aged 8 years old or younger who sustained open globe injuries between Jan. 1st, 2005 and Jan. 1st, 2015 was conducted. Enrolled patients had presented to the department of Ophthalmology and Visual Sciences, Prince of Wales Hospital in Hong Kong. Institutional Ethics Committee approval was obtained. The study adhered to the tenets of the Declaration of Helsinki.
An open globe injury was defined as a full-thickness wound of the eye wall. Zone of injury was defined as zone Ⅰ if the injury was confined to the cornea including the corneoscleral limbus; zone Ⅱ, if the injury was located at the corneoscleral limbus to a point 5 mm posterior into the sclera, and as zone Ⅲ if the injury was located posterior to zone Ⅱ[8].
All patients were evaluated on arrival to the emergency room. A standard history taking from the guardian and/or patient and ocular examination were completed whenever possible depending on the cooperation of the patient. The injured eyes were protected with eye shields and intravenous (ciprofloxcain) and topical (levofloxacin 0.5%, 8 times a day) antibiotics were started according to our departmental protocol. Repair of the open globe was arranged as an emergency operation under general anaesthesia.
If intraocular lens(IOL) implantation was required after primary or secondary cataract extraction, IOL power was calculated using the modified SRK-Ⅱ formula based on keratometry and axial length reading, and chosen depending on the age and refractive error in the fellow eye. Whenever corneal trauma precluded keratometry, measurements data from the fellow eye were used. Refractive errors were corrected with spectacles within 4 weeks after the primary operation or secondary operation followed by immediate occlusion therapy to treat amblyopia.
Data including age, sex, laterality of injury, etiology of injury, zone of injury, other associated ocular injuries, primary and secondary operations performed, best spectacle corrected visual acuity (BSCVA) at presentation, 3 months and 1 year postoperative, complications and refractive outcome were collected and analysed. The data were then subjected to descriptive statistical tabulation and analysis using SPSS version 15.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
A total of 7 cases, 2 boys and 5 girls were identified. The median age of presentation was 5 years (interquartile range, 3-5.5 years). The injury occurred in the right eye of one patient (14.3%) and the left eye of 6 patients (85.7%). All suffered from penetrating injuries (100%) and there were no globe ruptures or intraocular foreign body. Five (71%) had ocular injury in zone Ⅰ, two in zone Ⅱ (29%) and none in zone Ⅲ. The home was the most common place of injury occurrence (5 injuries, 71%). Table 1 shows the characteristics of the included patients.
Three cases suffered from traumatic cataract (43%). One case received primary lens aspiration due to capsular rupture and cortical material in the anterior chamber, two cases had secondary lens aspiration. IOL implantation was done as a secondary procedure for all cases. One case required a further operation for IOL repositioning due to dislocated intraocular lens.
One case had open globe injury due to the handle of the toy presenting together with corneal foreign body and infective keratitis and laceration repair was performed. The patient subsequently required a tectonic graft 2 weeks later due to a persistent corneal ulcer which perforated. During the second operation, intraoperative fundus examination showed retinal dialysis which was likely due to the primary trauma. A second corneal graft for failed graft and retinal dialysis repair was done for the same patient as a secondary operation.
There were three cases where preoperative visual acuity was not obtained due to difficulty incooperation during examination. Four cases (57%) had improvement of VA compared with preoperative VA. Final VA was hand movement in one (14%) patient, 20/200-20/50 in four (57%) patients, and 20/40 or better in two (29%) patients. There were no cases with NLP. The main complication is corneal scarring, which if it was not axial the visual outcome was not significantly affected. Only one case had postoperative visual acuity of hand movement at 1 year due to failed corneal graft and subsequent band keratopathy.
DISCUSSION
This is the first study to be conducted in a tertiary eye center on open globe injuries in children of amblyogenic age in Hong Kong. In the USA, a population-based study found an annual incidence of ocular trauma in children of 15.2/100000[9]. Open globe injuries in children occur mostly in preschool boys (66%). The number of cases of open globe injury over a 10-year period in our study has been relatively low compared to other studies. Another study conducted in Hong Kong looked at all paediatric eye injuries over a 5 year period also showed only 6 penetrating eye injuries out of a total of 60 children with severe eye injuries[10]. A possible reason for the lower incidence of open globe injuries in Hong Kong may be due to lower rate of open globe injuries that occur outdoors[11]. Children in Hong Kong tend to spend less time outdoors and have lower level of sports participation[12]. Sports injuries have been reported to be one of the common causes of eye injuries, especially with baseball, which is an uncommon sport in Hong Kong[13]. In our study, majority of the injuries occurred at home. This is similar to other studies where pre-school children predominately have injuries at home with objects such as glasses, scissors and knives[5,14]. Special attention should be given to children at home and the home environment to prevent such injuries happening.
Table 1Characteristics, surgery received and visual outcomes

Age(a)PlaceofocularinjuryCauseofruptureZoneOtherocularinvolvementPrimaryOperationSecondaryoperation(s)Timingtoseco-ndaryoperationPre-opVABCVA3/12BCVA1aComplications2HomeBrokenspectacles2IrisprolapseLacerationrepairNilN/A20/12820/64Paraxialcorneascar2HomeBrokenglasscup2Hyphema,IrisprolapseLacerationrepairNilN/A20/3220/64Peripheralcornealscar4HomeScissors1Irisprolapse,traumaticcataractLacerationrepairLensaspiration+IOL+cryotherapyforretinaltear4wkLP20/10020/70Peripheralcorneascar5HomeHandleoftoy1Cornealforeignbody,infectivekeratitisLacerationrepair,removalofcornealFBTectonicgraftandlensaspiration→penetratingkeratoplastyandretinaldialysisoperation2wk4wkN/A1/200HMFailedgraft,bandkeratopathy5HomePencil1TraumaticcataractLacerationrepairLensaspiration+IOL→IOLrepositioning1wk2wkLP12/20020/70Axialscar6SchoolScissors1TraumaticcataractLacerationrepair,primarylensaspirationSecondaryIOL4wk20/20020/4020/40InferiorIOLcapture,Paraxialcorneascar8PlaygroundBrokenspectacles1IrisprolapseLacerationrepairNil20/7020/4020/20Paraxialcorneascar
LP: Light perception; HM: Hand movement; N/A: Not available due to difficulty in cooperation; IOL: Intraocular lens; VA: Visual acuity; BCVA: Best corrected visual acuity.
There have been several risk factors quoted in the literature to be associated with poor visual outcome after open globe injury. This includes a poor presenting visual acuity[15], presence of relative afferent pupillary defect[14], posttraumatic endophthalmitis[1], more posterior wound location[16]. In our case series, children were under 8 years old so it was difficult to obtain visual acuity and relative afferent pupillary defect due to poor cooperation during examination. There were no cases of posttraumatic endophthalmitis in our case series. All open globe injuries occurred in zone Ⅰ or Ⅱ, which was similar to previous studies showing that most paediatric open globe injuries are localized in zone Ⅰ.
Traumatic cataract has been identified as a factor with poor visual outcome[7,17]. The timing of cataract operation as a primary procedure or secondary procedure has been debated[18-19]. Primary globe repair with cataract operation should not be delayed due to potential development of amblyopia and loss of binocular singular vision. Furthermore, early cataract operation allows better visualisation of posterior segment for associated ocular comorbidities. However, some propose secondary cataract operation due to less inflammation, a more stable wound after globe repair, increased corneal clarity and visualisation of capsule for cataract operation. We observed good visual outcomes with patients that had early lens aspiration (within 4 weeks) for visually significant traumatic cataract, combined with aggressive patching postoperatively.
Young age has also been reported to be a risk factor for poor visual outcome[13]. Liuetal[20]showed that 70% of the children under age of 6 years old had a worse visual outcome of 20/200 or less. This is because visual deprivation of children during amblyogenic age can affect long term visual outcome. In our case series, 86% were able to achieve 20/200 or better visual outcome at 1 year, which was relatively good in the young age group albeit our case series being small.
We compared our case series with a retrospective study conducted at our unit studying open globe injuries and reanalyzed the data for subjects older than 8 years old[3](Table 2). All cases under 8 years old in our case series had visual acuity of 1/200 or better at 3 months. For cases that were 8 years or older, 49% had visual acuity of count finger or worse at 3 months. The preoperative logMAR visual acuity in was 2.19/1.90±0.9 and 2.35/2.70±0.83 in subjects younger than 8 years old and older than 8 years old respectively (median/mean±SD;P=0.646, Mann Whitney U test). The 3 month postoperative logMAR visual acuity was 0.83/0.70±0.74 and 1.79/2.30±0.74 in subjects younger than 8 years old and older than 8 years old respectively (median/mean±SD;P=0.030, Mann Whitney U test). Visually significant complications occurred in 29% in our case series, and 50.3% in subjects older than 8 years old, although there was no statistical difference between the two groups (P=0.26, Chi-square test). In another 10-year review of open globe injuries involving mainly adults in Hong Kong[21], the group reported 66% of cases presented with a poor presenting visual acuity of less than 5/200 and 46% with a final visual acuity less than 5/200 in a series of 121 patients. Their major causes of open globe injury are workplace injury (36%) followed by fall (32%) and assault (13%) which are associated with a higher force factor when compared with the causes of injury in children involving mainly domestic injury. Relatively good visual outcomes in our case series could have been due to less risk factors for poor final visual outcome as discussed above and due to early management of amblyopia.
Our present case series overall showed that the most common cause of open globe injuries in young children are domestic accidents. Good visual outcomes can be obtained especially if the laceration does not involve the central cornea, prompt management of open globe injuries together with aggressive management of other associated injuries and amblyopia, and if there are not infective complications. Our limitation of this study that it is a retrospective study with limited number of cases.
Table 2Comparison of visual outcomes between open globe injuries in children under 8 years old and over 8 years old (Patient data from Kuhnetal[2])
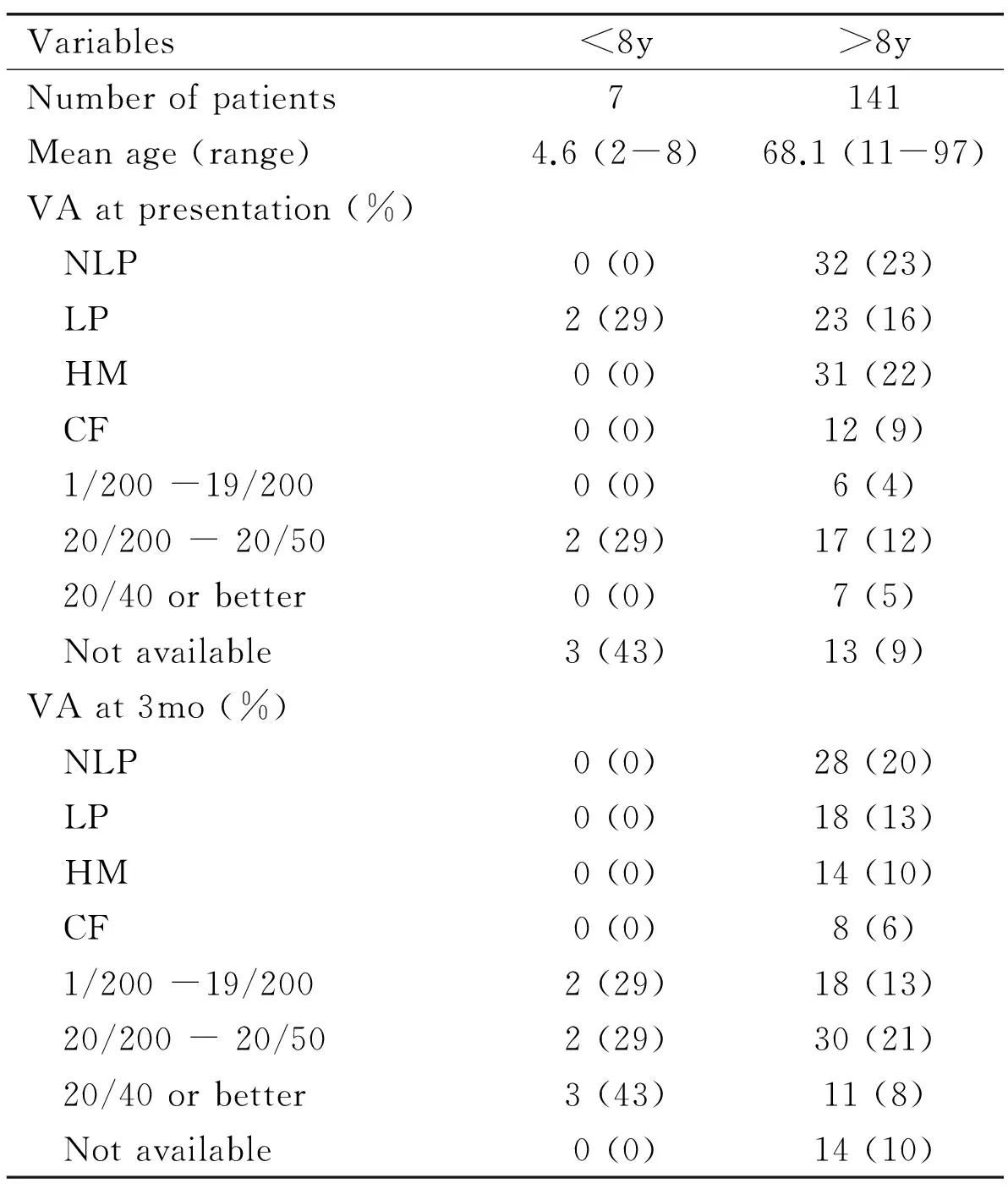
Variables<8y>8yNumberofpatients7141Meanage(range)4.6(2-8)68.1(11-97)VAatpresentation(%) NLP0(0)32(23) LP2(29)23(16) HM0(0)31(22) CF0(0)12(9) 1/200-19/2000(0)6(4) 20/200-20/502(29)17(12) 20/40orbetter0(0)7(5) Notavailable3(43)13(9)VAat3mo(%) NLP0(0)28(20) LP0(0)18(13) HM0(0)14(10) CF0(0)8(6) 1/200-19/2002(29)18(13) 20/200-20/502(29)30(21) 20/40orbetter3(43)11(8) Notavailable0(0)14(10)
VA: Visual acuity; NLP:No light perception; LP: Hand movement; HM: Hand movement; CF: Count finger.
In conclusion, although open globe injuries in paediatric population are uncommon in our locality, it can result in high morbidity. Special challenges in children occurred during preoperative and postoperative assessment and management, especially to prevent amblyopia.
1 Pieramici DJ, Au Eong KG, Sternberg P Jr, Marsh MJ. The prognostic significance of a system for classifying mechanical injuries of the eye (globe) in open-globe injuries.JTrauma2003;54(4):750-754
2 Kuhn F, Morris R, Witherspoon CD, Mester V. The Birmingham Eye Trauma Terminology system (BETT).JFrOphtalmol2004;27(2):206-210
3 Ying Fong YY, Yu M, Young AL, Jhanji V. Presentation and Management Outcomes of Corneal and Scleral Perforations in Geriatric Nursing Home Residents.Medicine(Baltimore) 2015;94(36):e1518-e1510
4 Jandeck C, Kellner U, Bornfeld N, Foerster MH. Open globe injuries in children.GraefesArchClinExpOphthalmol2000;238(5):420-426
5 Tok O, Tok L, Ozkaya D, Eraslan E, Ornek F, Bardak Y. Epidemiological characteristics and visual outcome after open globe injuries in children.JAAPOS2011;15(6):556-561
6 Bai H, Meng X, Wang D, Han J. Treatment for amblyopia after surgery for cataract and vitreoretina in pediatric ocular trauma.EyeSci2013;28(2):68-72
7 Reddy AK, Ray R, Yen KG. Surgical intervention for traumatic cataracts in children: Epidemiology, complications, and outcomes.JAAPOS2009;13(2):170-174
8 Pieramici DJ, Sternberg P Jr, Aaberg TM Sr, Bridges WZ Jr, Capone A Jr, Cardillo JA, de Juan E Jr, Kuhn F, Meredith TA, Mieler WF, Olsen TW, Rubsamen P, Stout T. A system for classifying mechanical injuries of the eye (globe). The Ocular Trauma Classification Group.AmJOphthalmol1997;123(6):820-831
9 Strahlman E, Elman M, Daub E, Baker S. Causes of pediatric eye injuries. A population-based study.ArchOphthalmol1990;108(4):603-606
10 Poon AS, Ng JS, Lam DS, Fan DS, Leung AT. Epidemiology of severe childhood eye injuries that required hospitalisation.HongKongMedJ1998;4(4):371-374
11 Health Do. Report on health effects of use of internet and electronic screen products. 2014. Available at: http://www.info.gov/hk/gia/general/201407/08/P201407070686.htm. Accessed Nov 22, 2015
12 Maffulli N, Bundoc RC, Chan KM, Cheng JC. Paediatric sports injuries inHong Kong: a seven year survey.BrJSportsMed1996;30(3):218-221
13 Cascairo MA, Mazow ML, Prager TC. Pediatric ocular trauma: a retrospective survey.JPediatrOphthalmolStrabismus1994;31(5):312-317
14 Bunting H, Stephens D, Mireskandari K. Prediction of visual outcomes after open globe injury in children: a 17-year Canadian experience.JAAPOS2013;17(1):43-48
15 Gupta A, Rahman I, Leatherbarrow B. Open globe injuries in children: factors predictive of a poor final visual acuity.Eye(Lond) 2009;23(3):621-625
16 Sternberg P Jr, de Juan E Jr, Michels RG, Auer C. Multivariate analysis of prognostic factors in penetrating ocular injuries.AmJOphthalmol1984;98(4):467-472
17 Shah MA, Shah SM, Shah AH, Pandya JS. Visual outcome of cataract in pediatric age group: does etiology have a role.EurJOphthalmol2014;24(1):76-83
18 Adlina AR, Chong YJ, Shatriah I. Clinical profile and visual outcome of traumatic paediatric cataract in suburbanMalaysia: a ten-year experience.SingaporeMedJ2014;55(5):253-256
19 Moisseiev J, Segev F, Harizman N, Arazi T, Rotenstreich Y, Assia EI. Primary cataract extraction and intraocular lens implantation in penetrating ocular trauma.Ophthalmology2001;108(6):1099-1103
20 Liu X, Liu Z, Liu Y, Zhao L, Xu S, Su G, Zhao J. Determination of visual prognosis in children with open globe injuries.Eye(Lond) 2014;28(7):852-856
21 Li EY, Chan TC, Liu AT, Yuen HK. Epidemiology of Open-Globe Injuries inHong Kong.AsiaPacJOphthalmol(Phila) 2016
香港地区儿童弱视易发性年龄组中开放性眼球创伤的特征及视力预后
方若盈, 刘庆伟, 叶伟权, 杨乐旼
999077中国香港,威尔斯亲王医院 香港中文大学眼科及视觉科学系)
Wilson Yip Wai Kuen.中国香港威尔斯亲王医院香港中文大学眼科及视觉科学学系. ywk806@ha.org.hk
目的:评估香港地区弱视易发期的儿童开放性眼球创伤的统计学及临床特征以及视力预后。
眼球破裂;开放性眼球创伤;儿童眼球创伤
Wilson Yip Wai Kuen. Department of Ophthalmology & Visual Sciences, Prince of Wales Hospital, Shatin, Hong Kong 999077, China. ywk806@ha.org.hk
2016-05-22Accepted: 2016-08-08
10.3980/j.issn.1672-5123.2016.11.02
Fong Y, Lau HW, Yip WW, Young AL. Characteristics and visual outcomes of open globe injuries in children of amblyogenic age in Hong Kong.GuojiYankeZazhi(IntEyeSci) 2016;16(11):1988-1991
引用:方若盈, 刘庆伟, 叶伟权, 等. 香港地区儿童弱视易发性年龄组中开放性眼球创伤的特征及视力预后.国际眼科杂志2016;16(11):1988-1991