早期去骨瓣减压并颅内压监测治疗大面积脑梗死*
2016-09-26王建伟王文学刘宇梁伏光辉康新袁涛彭霞林张爱娟
王建伟王文学刘宇梁伏光辉康新袁涛彭霞林张爱娟
早期去骨瓣减压并颅内压监测治疗大面积脑梗死*
王建伟①王文学①刘宇梁①伏光辉①康新①袁涛①彭霞林①张爱娟①
目的:本研究旨在评估早期去骨瓣减压术对大面积脑梗死早期及短期预后的影响。方法:选取2010年9月-2015年12月本院大面积脑梗死患者42例,根据是否同意手术分为三组,9例<12 h手术为A组,24例>12 h手术为B组,9例保守治疗为C组。采用美国国立卫生院脑卒中量表(NIHSS)及昏迷评分(GCS)评估神经功能,弥散加权磁共振(DWI)或CT用于界定脑梗死范围,在NICU统一治疗并行颅内压(ICP)监测,ICP持续超过30 mm Hg给予降颅压无效行梗死侧颞极切除。采用巴氏指数(BI)和预后评分(GOS)评估所有患者病后3个月神经功能。结果:脑梗死后12 h内颅脑CT诊断的准确率为44.4%,DWI的准确率为100%。入院后GCS均呈现下降趋势,A、B组术前GCS比较差异有统计学意义(P<0.05)。手术组早期及短期治疗效果均优于保守组,A组早期及短期评价指标亦大多优于B组,比较差异有统计学意义(P<0.05)。结论:去骨瓣减压术手术本身风险相对较低,容易实施并可确切降低大面积脑梗死的死亡率,尤其12 h内实施更能改善预后,术后连续ICP监测可及早发现恶性高颅压并及时实施颞极切除。
去骨瓣减压术; 大面积脑梗死; 颅内压; 颞极切除; 预后
大面积脑梗死保守治疗死亡率高达80%,去骨瓣减压术可以有效降低颅内压(intracranial pressure,ICP),打破脑水肿的恶性循环,是目前公认的挽救该类患者生命的手段[1]。但存活患者的健康状况及生活满意度低,目前研究证实大骨瓣减压术可有效提高存活患者的生活质量,尤其对于年轻患者更加重要。本前瞻性临床研究在密切观察病情配合先进的影像学技术前提下[2-3],早期实施手术,并且术后行ICP监测早期发现恶性脑水肿并及时实施了梗死侧颞极切除,获得了较好的疗效,现报道如下。
1 资料与方法
1.1 一般资料 选取本院2010年9月-2015年12月符合研究条件的大面积脑梗死患者42例,年龄40~78岁。所有患者均有手术指征,根据是否同意手术分为保守组和手术组,手术组中发病至手术时间小于12 h者为A组9例,大于12 h者为B组24例,但均在72 h内实施;保守组为C组9例。纳入标准:(1)发病后24 h内入院;(2)美国国立卫生院脑卒中量表(National Institutes of health Stroke Scale,NIHSS)评分>20分且意识水平单项评分≥1分;(3)颅脑CT显示缺血区超过大脑中动脉供血范围的50%或弥散加权磁共振(diffusion-weighted imaging,DWI)显示梗死体积大于145 cm3。排除标准:(1)双侧脑梗死;(2)脑梗死合并明显出血;(3)小面积脑梗死;(4)脑疝晚期;(5)严重器官功能障碍。该研究已经伦理学委员会批准,患者知情同意。
1.2 方法 (1)保守治疗:根据缺血性卒中等的诊疗指南进行管理[1-4],侧脑室穿刺置管外接有创压力传感器行连续ICP监测,ICP增高明显者行气管插管以保证供氧,尽量控制加重脑水肿的因素,静滴甘露醇及速尿仅仅用于脑水肿明显者。(2)手术治疗:梗死侧实施大骨瓣减压术[5],骨瓣范围包括额颞顶及部分枕骨,星形剪开硬脑膜,根据患者术中颅压情况可选做人工硬膜减张缝合[6],若术前显示梗死范围超出大脑中动脉或ICP持续超过30 mmHg给予甘露醇等降颅压措施,无效则行颞极切除内减压[7-8]。
1.3 观察指标及预后评分 完整记录所有患者性别、年龄、发病至手术时程等临床资料。使用昏迷评分(Glasgow Coma Scale,GCS),NIHSS量表对患者入院时评分。发病后3个月应用巴氏指数(Barthel Index,BI)对患者日常生活能力进行评估,应用预后评分(Glasgow Outcome Scale,GOS)对患者预后情况进行评估,4~5分为预后良好,1~3分为预后差。
1.4 统计学处理 使用SPSS 19.0统计学软件进行数据分析,计量资料以(±s)表示,比较采用t检验,计数资料采用 χ2检验,组间比较采用Fisher确切概率法,以P<0.05为差异有统计学意义。
2 结果
2.1 三组患者临床基本资料比较 三组患者年龄、性别、梗死侧别、入院时GCS、入院时NIHSS、入院时出现脑疝人数、梗死体积等指标比较差异均无统计学意义(P>0.05)。脑梗死后12 h内颅脑CT诊断的准确率为4/9(44.4%),DWI的准确率为100%。术前患者GCS均呈现下降趋势,经保守治疗神经功能均呈现恶化趋势,A、B组术前GCS比较差异有统计学意义(P<0.05),见表1。
2.2 各组的临床指标比较 A组术后有1例行颞极切除术,B组有3例行颞极切除术。手术组早期及短期治疗效果均优于C组,A组早期及短期评价指标亦大多优于B组,比较差异有统计学意义(P<0.05),见表2,典型病例见图1。
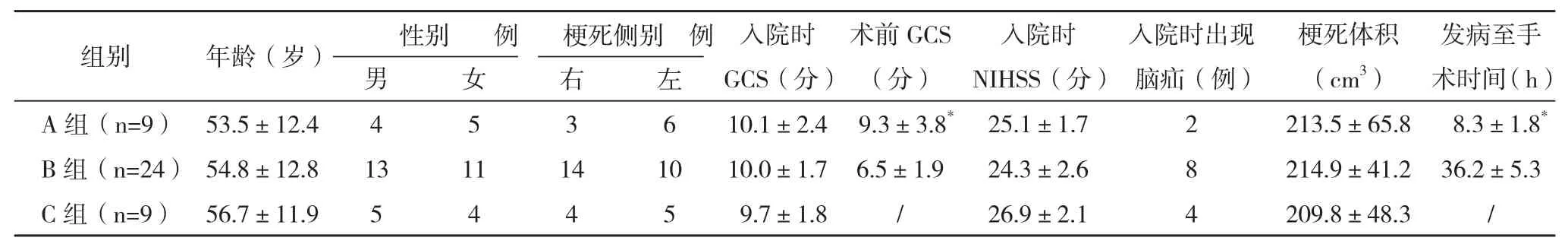
表1 各组一般资料比较

表2 各组临床指标比较

图1 典型病例
3 讨论
单侧大面积脑梗死包括大脑中动脉梗死占到幕上梗死病例的10%~15%,缺血性水肿导致早期出现ICP增高,从而继发脑疝甚至死亡,死亡率高达80%,存活者临床预后差[7-10]。已证实内科治疗无法有效预防脑疝,大面积脑梗死发生恶性脑水肿内科保守无效,需实施去骨瓣减压术,动物实验表明去骨瓣减压术可以增加梗死后缺血区的供血,改善预后甚至可以减小梗死体积,且越早实施此项手术效果越好[11]。研究表明去骨瓣减压术可将大面积脑梗死死亡率由80%降低至34%以下,且接受手术治疗存活患者的日常生活能力优于保守治疗者[11-12]。本研究同样表明手术组患者存活率及神经功能恢复均优于保守组,且手术时间越早效果越好。
去骨瓣减压旨在挽救缺血半暗区,而缺血半暗区受缺血时间和缺血严重程度不同可逆程度不同,如何在早期预测发生恶性脑水肿的可能性是关键。手术时机的把握是决定大面积脑梗死手术效果和预后的关键因素,目前认为一旦有手术指征应该尽早手术,据神经系统体征、GCS、早期及连续颅脑CT、MRI检查和ICP动态监测等综合分析,以决定最适合的手术时机。Kiphuth等[13]指出NHISS>20分预示着恶性脑梗死,且可预示卒中程度。Taylor等[14]指出意识水平下降、肢体运动障碍程度、凝视麻痹均与患者的预后相关。GCS及脑疝程度是常用于判断病情和选择治疗时机的重要指标,本研究中虽然三组患者入院时GCS无统计学差异,但入院后均呈现下降趋势,神经功能亦呈现恶化趋势,<12 h手术组与>12 h手术组术前GCS比较差异有统计学意义(P<0.05)。有关报道缺血性脑卒中7 h内CT诊断的准确率为14%~43%,而DWI诊断的准确率为57%~86%,特异性为92%~100%。本研究表明脑梗死后12 h内CT诊断的准确率为4/9 (44.4%),DWI的准确率为100%。因此为能早期诊断脑梗死及行去骨瓣减压术,DWI的重要性凸显出来。随着影像学技术的日新月异,如今颅脑CT可以在梗死发病后12 h发现梗死灶,临床上DWI在梗死发病后6 h即可清楚显示病灶范围,这就保证了早期实施去骨瓣减压术的可行性。因此,DWI、NHISS>20分及GCS可作为早期诊断恶性大脑中动脉梗死的依据。
去骨瓣减压术本身并不能直接减轻缺血脑组织的局部损伤,但去骨瓣后ICP下降,可减轻由于高颅压导致的继发性脑损伤[15],所以去骨瓣的范围成为手术的关键因素,本研究采取标准大骨瓣开颅,统一术中咬平前、中颅窝底,向后跨过顶结节,获得充分减压;咬除或磨平蝶骨嵴返折部,使侧裂血管充分减压,改善侧裂供血和静脉回流。术中是否切除缺血失活的脑组织仍有争议,因为目前尚无有效的方法确定缺血坏死区和半暗区,但本研究权衡患方经济负担及ICP监测必要性前提下统一采用侧脑室置管外接有创压力传感器的方法,在术中或术后出现ICP持续超过30 mm Hg情况下给予甘露醇等降颅压措施,无效时果断采用梗死侧颞极切除,术后显示ICP得以控制。目前临床大多探索应用标准大骨瓣减压+颞肌贴敷术[16-17]、大骨瓣减压+血管吻合术试图早期恢复脑组织供血,也有学者试图改良大骨瓣减压术[18-19],但均缺乏大规模多中心随机对照研究的支持,故本研究未采用以上方法。
在DWI确定梗死体积大于145 cm3后无手术禁忌情况下尽早实施大骨瓣减压术可降低死亡率并改善存活患者的生活质量[20]。本研究表明<12 h手术组死亡率仅为9.5%,>12 h手术组为37.8%,而保守治疗组死亡率却高达82.0%。<12 h手术组有88.3%的患者术后7 d可配合医生完成简单指令,<12 h手术组3个月BI及GOS同样优于其他两组,可见尽早实施大骨瓣减压术并配合ICP监测及早实施必要的梗死侧颞极切除术可降低死亡率、缩短患者意识恢复时间、改善神经功能,关于去骨瓣减压术后大脑中动脉的血流动力学参数改变是本研究深入的方向。
[1]杜伟,庞长河,薛亚轲,等.美国神经重症监护学会《大面积脑梗死治疗指南(2015)》解读[J].中华神经医学杂志,2016,15(1):2-5.
[2] Kim H,Jin S T,Kim Y W,et al.Predictors of malignant brain edema in middle cerebral artery infarction observed on CT angiography[J].Journal of Clinical Neuroscience Official Journal of the Neurosurgical Society of Australasia,2015,22(3):554-560.
[3] Son S,Choi D S,Choi N C,et al.Serial magnetic resonance images of a right middle cerebral artery infarction : persistent hyperintensity on diffusion-weighted MRI over 8 months[J].Journal of Korean Neurosurgical Society, 2011,50(4):388-391.
[4] Jauch E C,Saver J L,Adams H P,et al.Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/ American Stroke Association[J].Stroke,2013,44(3):870-947.
[5] Johnson R D,Maartens N F,Teddy P J.Technical aspects of decompressive craniectomy for malignant middle cerebral artery infarction[J].Journal of Clinical Neuroscience Official Journal of the Neurosurgical Society of Australasi,2011,18(8):1023-1027.
[6] Yao Y,Mao Y,Zhou L.Decompressive craniectomy for massive cerebral infarction with enlarged cruciate duraplasty[J].Acta Neurochirurgica,2008,149(12):1219-1221.
[7] Cho D Y,Chen T C,Lee H C.Ultra-early decompressive craniectomy for malignant middle cerebral artery infarction[J]. Surgical Neurology,2003,60(3):232-233.
[8] Hao Z,Chang X,Zhou H,et al.A Cohort Study of Decompressive Craniectomy for Malignant Middle Cerebral Artery Infarction: A Real-World Experience in Clinical Practice[J]. Medicine,2015,94(25):e1039.
[9] Vahedi K,Vicaut E,Mateo J,et al.Sequential-design,multicenter,randomized,controlled trial of early decompressive craniectomy in malignant middle cerebral artery infarction (DECIMAL Trial)[J].Stroke,2007,38(9):2506-2517.
[10] Raffiq M A,Haspani M S,Kandasamy R,et al.Decompressive craniectomy for malignant middle cerebral artery infarction:Impact on mortality and functional outcome[J].Surgical Neurology International,2014,5(1):102.
[11] Amorim R L,De Andrade A F,Gattás G S,et al.Improved hemodynamic parameters in middle cerebral artery infarction after decompressive craniectomy[J].Stroke,2014,45(5):1375-1380.
[12] Yamaguchi H,Yamamoto K,Akutsu N,et al.Decompressive craniectomy 116 h after malignant middle cerebral artery infarction[J].Pediatrics International Official Journal of the Japan Pediatric Society,2016,58(7):622-624.
[13] Kiphuth I C,Köhrmann M,Lichy C,et al.Hemicraniectomy for malignant middle cerebral artery infarction: retrospective consent to decompressive surgery depends on functional longterm outcome[J].Neurocritical Care,2010,13(3):380-384.
[14] Taylor B,Appelboom G,Connolly ES.Age selection for decompressive craniectomy in malignant middle cerebral artery infarction[J].World Neurosurgery,2015,83(3):301-302.
[15] Lu X,Huang B,Zheng J,et al.Decompressive craniectomy for the treatment of malignant infarction of the middle cerebral artery[J].Scientific Reports,2014,4(17):7070.
[16]高玉华,张远明.大面积脑梗死行大骨瓣减压加颞肌贴敷术的手术时机[J].江苏医药,2014,40(20):2499-2500.
[17]章月江,屠传建,陈华炜,等.标准大骨瓣减压加颞肌贴敷开颅术治疗大面积脑梗死的临床研究[J].浙江创伤外科,2014,19(6):990-991.
[18]蔡恩源,白志强,董玲.“双C形”去骨瓣减压术治疗大面积脑梗死的效果[J].青岛大学医学院学报,2009,45(6):522-523.
[19]张新平,徐庆余,卢鹏,等.双侧额颞平衡改良大骨瓣减压术治疗大面积脑梗死的疗效[J].中国实用神经疾病杂志,2016,19(7):2.
[20] Kenning T J,Gooch M R,Gandhi R H,et al.Cranial decompression for the treatment of malignant intracranial hypertension after ischemic cerebral infarction: decompressive craniectomy and hinge craniotomy[J].Journal of Neurosurgery,2012,116(6):1289-1298.
Early Decompressive Craniectomy and Intracranial Pressure Monitoring and Treatment of Malignant
Massive Cerebral Infarction
/WANG J ian-wei,WANG Wen-xue,L IU Y u-liang,et al.//Medical Innovation of China,2016,13(25):007-010
Objective:To assess the influence of short term prognosis of early decompressive craniectomy in patients with massive cerebral infarction.Method:From September 2010 to December 2015,42 cases of massive cerebral infarction in our hospital were selected,they were divided into three groups,9 cases of <12 h operation as group A,24 cases of >12 h operation as B group,9 cases with conservative treatment as group C.The national institutes of health stroke scale(NIHSS) and glasgow coma scale(GCS) were used to evaluate clinical neurologic function.Diffusion weighted imaging(DWI) and CT were used to evaluate the cerebral infarction territory. All patients were treated in NICU with intracranial pressure(ICP)monitoring.Anterior temporal lobectomy was performed when the ICP continued to exceed 30 mm Hg.The outcome was assessed using the Barthel Index (BI) and the GOS in all patients after 3 months.Result:The accuracy rate of diagnosis by CT was 44.4% and the accuracy rate of DWI was 100% within 12 h after onset.Compared group A and B of GCS scores beforeoperation,the difference was statistically significant(P<0.05).The early and short term outcome of the operation group were better than that of the conservative group.The early and short-term evaluation indexes of the group A were also better than those of group B,the difference was statistically significant(P<0.05).Conclusion:In this trial,the risk of decompressive craniectomy is relatively low,it is easy to implement and can significantly reduce the mortality rate,especially within 12 h. Postoperative continuous ICP monitoring can detect malignant high ICP and timely implementation of temporal lobectomy.
Decompressive craniectomy; Massive cerebral Infarction; Intracranial pressure;Anterior temporal lobectomy; Prognosis
10.3969/j.issn.1674-4985.2016.25.003
2016-05-27) (本文编辑:周亚杰)
江苏省连云港市521高层次人才培养工程资助项目(521-3-11)
①江苏省连云港市东方医院 江苏 连云港 222042
王文学
First-author’s address:Dongfang Hospital of Lianyungang City,Lianyungang 222042,China
