复杂型腹主动脉瘤血管腔内介入治疗效果分析及评价
2016-08-03李浩诚沈永斌姜维良哈尔滨医科大学附属第二医院血管外科哈尔滨150086
李浩诚 沈永斌 姜维良哈尔滨医科大学附属第二医院 血管外科,哈尔滨 150086
复杂型腹主动脉瘤血管腔内介入治疗效果分析及评价
李浩诚 沈永斌 姜维良*
哈尔滨医科大学附属第二医院 血管外科,哈尔滨 150086
目的 通过对患者病情、术前相关检查、手术方法、术后治疗措施及随访这几方面进行回顾性研究,讨论分析应用血管腔内介入技术治疗复杂型腹主动脉瘤的治疗效果。方法 将2011年1月至2015年6月就诊于哈尔滨医科大学附属第二医院血管外科并行手术治疗的156例患者的病情、术前相关检查、手术方法、术后治疗措施等资料整理收集,共将其分为2组:复杂型腹主动脉瘤患者组(A组),共63例,普通型腹主动脉瘤患者组(B组),共93例,将这些患者的临床资料,整理总结,并进行分析。结果 2组手术成功率均为100%。围手术期及随访期间,复杂型腹主动脉瘤组出现1例死亡,围术期内出现内漏11例,经治疗内漏均消失;随访期发生4例内漏,多数经保守观察后消失,仅1例需治疗。普通型腹主动脉瘤组未出现死亡病例,围术期内出现内漏14例,经治疗内漏均消失;随访期内出现内漏6例,经保守治疗观察期内漏消失。计算机断层扫描血管造影(CTA)检查证实在术后及随访期间2组患者无明显支架移位发生。结论 复杂型腹主动脉瘤组与普通型腹主动脉瘤组,在住院时间、手术时间、远期存活率及并发症的发生率2组无明显差异。血管腔内介入技术能够有效的治疗复杂型性腹主动脉瘤。
复杂型腹主动脉瘤;腹主动脉瘤腔内修复术;并发症
腹主动脉瘤(abdominal aortic aneurysm, AAA)多数治疗并不能取得满意的效果[1]。血管腔内介入治疗的出现[2]使AAA得以有效的治疗,整体生存率明显提高。AAA患者多为老年患者,对于常规手术不能耐受[3],既往存在高血压、冠心病、心梗、脑梗等病史。腔内修复术(endovascular aneurysm repair, EVAR)手术相较于传统开放手术而言[4],其创伤小,恢复快,患者可早期下地活动,并可减少或无需术中输血,同时术后监护时间缩短,患者整体住院时间缩短,EVAR能减少手术对于患者的创伤。随访发现尽管开放手术的方式在肾动脉水平以上钳夹主动脉出现的风险较低[6],但其术后产生的并发症与死亡率较高,面对这样的患者时,许多术者拒绝施行开放性手术[7]。应用EVAR治疗复杂型腹主动脉瘤逐渐成为最佳的治疗方法。但EVAR能否使复杂型腹主动脉瘤患者以较小的代价获得较大的收益,临床上虽然进行了大量的随访研究,但对其有效性和可靠性仍需长期观察[8]。近几年,新型开窗—分支型支架的出现使AAA的治疗有了更好的发展[9],目前多数仍处于临床试验研究阶段,但在不久的将来,随着不断改进和发展,越来越多的患者将能够接受开窗—分支支架的治疗。新型支架的发展必将为AAA的治疗带来更好的前景[10]。
1 材料及方法
1.1 研究对象
对2011年1月至2015年6月就诊于哈尔滨医科大学附属第二医院血管外科并行手术治疗的156例患者的病情、术前相关检查、手术方法、术后治疗措施等资料进行整理收集。将156例患者共分2组,A组为复杂型腹主动脉瘤组,63例;B组为普通型腹主动脉瘤组,93例。所有患者均经主动脉计算机断层扫描血管造影(CTA)、数字减影血管造影(DSA)等明确诊断。
1.2排纳标准
入选标准:术前所有患者均行主动脉CTA检查,主要包括观察动脉瘤形态,是否呈明显偏心性生长,近端锚定区长度、成角畸形等;瘤体长度及直径;腹主动脉分叉部直径;肾动脉开口至腹主动脉分叉处长度、腹主动脉分叉处至双侧髂内动脉开口处长度等。经测量及3维影像观察,将患者分为复杂型腹主动脉瘤(A)组和普通型腹主动脉瘤(B)组。A组诊断标准主要包括:瘤颈成角扭曲;近端锚定区处瘤颈长度<15 mm,近端瘤颈直径>30 mm;瘤颈成角>45°;瘤颈处钙化面积≥25%或主动脉壁附壁血栓面积≥50%;肾动脉旁及肾上腹主动脉瘤;累积髂血管的腹主动脉瘤;入路狭窄、肾动脉狭窄;动脉瘤破裂及假性动脉瘤。符合以上标准的患者为A组,其余患者收入B组。
排除标准:感染性腹主动脉瘤、多发性大动脉炎、自身免疫性疾病等。
1.3 手术过程
除急诊手术外,一般术前均给予内科治疗,控制血压、心率等至平稳状态,待患者状态稳定。术前精确测量多部位主动脉直径,观察动脉瘤瘤颈及瘤体形态,备选腔内及人工血管移植物,决定施行EVAR或杂交手术。全麻下气管插管,确切术野下逐层切开显露双侧股总动脉近、远端套带备用或预置双缝合器备用,静脉推注肝素,实现全身肝素。术前以CTA轴位图像测得的直径做为主动脉主体覆膜支架选择的标准,术中结合造影结果,再次对支架的选择进行评估。分别释放主体与髂肢支架。支架释放完成后,需再次进行造影观察支架形态与位置是否有内漏存在、动脉瘤是否隔绝完全。将导管连同导丝一起撤出动脉,缝合动脉壁穿刺处,逐层缝合皮肤及皮下组织;预置缝合器患者行缝合器缝合并剪断,加压包扎创口,转入ICU监护。
1.4 术后治疗与随访
术后患者均转入ICU病房监护,常规为24 h。对于高血压患者,早期静脉输注药物降压治疗,待患者血压平稳后,逐步改为口服降压药控制,并观察其效果,叮嘱患者长期口服降压药物,维持血压平稳。
本次入组患者术后随访期为0~24个月。以电话的形式通知其随访治疗,随访结果均以门诊复诊的主动脉CTA为主。
1.5 资料采集
1.5.1一般信息采集
(1)患者基本情况;
(2)患者入院情况如首发症状,伴随症状如下肢血运,腹腔脏器灌注,代谢情况,住院天数等;
(3)手术操作过程如具体手术及麻醉方式、时间,血管腔内移植物型号规格及术中特殊情况记录等;
(4)围手术期患者实验室(如肝、肾功指标)及影像学(如CTA)检查,生命体征变化情况、术后并发症等;
(5)随访内容包括并发症的发生与治疗,原发疾病是否复发等。
1.5.2 影像学信息收集
径线测量:(1)近端瘤颈内径;(2)动脉瘤最大直径;(3)瘤体远端主动脉直径;(4)分叉部位血管直径; (5)髂总动脉内径;(6)近端瘤颈的长度; (7)瘤体上缘至下缘的长度。

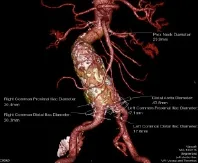

图1 测量示意图
1.6 统计学分析
收集整理所有患者的住院病历及随访资料,用均数±标准差表示正态分布的计量资料,采用t检验;样本比较率采用Fisher确切概率法。应用SPSS 17.0国际标准统计学编程软件进行统计分析。P>0.05表明无明显统计学意义,P<0.05表明差异有明显统计学意义。
2 结果
患者在疼痛的症状、动脉瘤长度及直径方面有明显差异(P<0.05),在既往史方面无明显统计学意义。但复杂型腹主动脉瘤组患者年龄明显高于普通型动脉瘤组,且平均手术时间、平均住院时间较普通型动脉瘤组长(表1)。
复杂型腹主动脉瘤(A组)组与普通型腹主动脉瘤组(B组)在死亡率、内漏发生率、血管损伤比率方面无明显差异(表2)。
复杂型腹主动脉瘤组(A组)与普通型腹主动脉瘤组(B组),在内漏发生、支架阻塞及总生存率方面无统计学差异(表3)。

表1 研究对象临床资料

表2 围手术期治疗比较
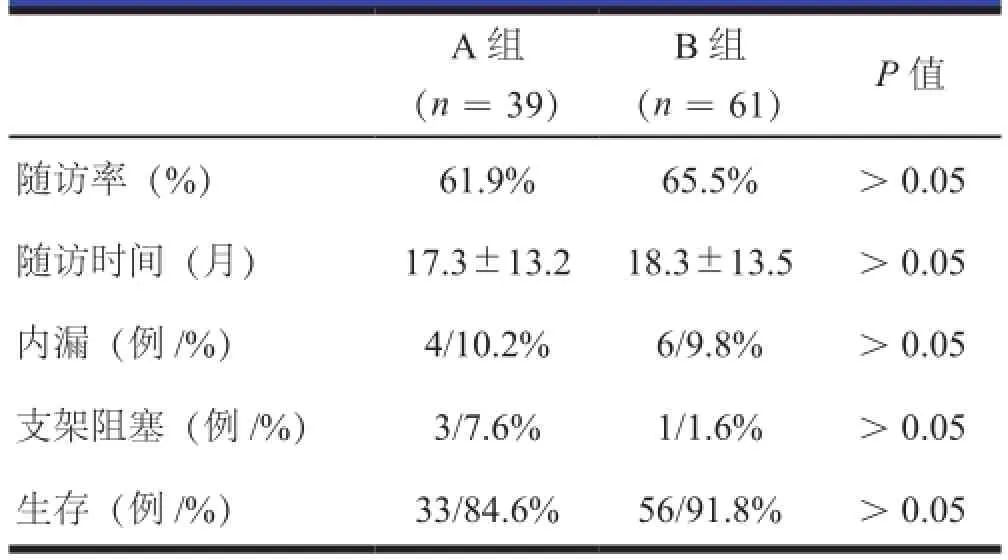
表3 术后随访比较
3 讨论
3.1 数据分析讨论
复杂型腹主动脉瘤患者组与普通型腹主动脉瘤患者组2者进行比较,虽然在年龄、性别、住院时间、基础疾病等方面未出现明显差异。但可以看到的是相较于普通型动脉瘤组而言,复杂型动脉瘤组平均年龄高,解剖条件较复杂,在瘤体直径及瘤体长度上有明显差异,有腹部疼痛主诉的患者较多,均提示其治疗的高危性及复杂性。从平均手术时间来看,复杂型腹主动脉瘤组除其中3例患者施行杂交手术外,其余患者均行EVAR手术,与普通型腹主动脉瘤组相比较,其平均手术时间更长。这是由于解剖条件的复杂性,包括入路动脉的狭窄、成角、闭塞;髂动脉夹层、动脉瘤形成;瘤体成角较大;部分存在较大的附壁血栓。研究结果显示:复杂型腹主动脉瘤组及普通型腹主动脉瘤组均出现随访期内漏,多数经观察随访自行封闭,仅1例需再次治疗。2组患者均有支架内阻塞出现。在总体生存率上,普通型组优于复杂腹主动脉瘤组。
3.2内漏治疗讨论
EVAR手术中最主要的并发症为内漏[11]。相关随访[12]表明随访期内有漏并接受再次干预的患者,动脉瘤从第2年开始增长。无内漏的患者,动脉瘤尺寸持续下降。内漏的发生与治疗是评价手术与治疗效果的一项重要标准。过去,内漏的存在是限制EVAR应用于复杂型腹主动脉瘤的原因之一[13]。现在,随着相关经验的积累及支架移植物的改进,使得内漏的发生率降低,并得到很好的治疗[14]。从表2和表3的数据可以看出,虽然复杂型腹主动脉瘤组较普通型腹主动脉瘤组内漏发生率高,却无明显统计学意义。从相关经验来看,首先在支架的选择上,oversize要适当选择[15],瘤颈不良者更应该适当放大,结构不良性疾病应该缩小。球囊扩张治疗、cuff支架及裸支架植入、反流血管弹簧圈栓塞等均可有效治疗内漏。
由于近年来随着经验的积累,介入器材的不断改进、支架种类的丰富及设计的进步、EVAR技术的不断发展等使得复杂型腹主动脉瘤通过血管腔内介入技术进行治疗的想法得以实现,且取得了满意的治疗效果。在多项指标的比较上可见,复杂型腹主动脉瘤组在治疗效果、并发症、生存率等方面与普通型动脉瘤组无明显差异。
[1]Dijkstra ML, Tielliu IFJ, Meerwaldt R, et al. Dutch experience with the fenestrated Anaconda endograft for short-neck infrarenal and juxtarenal abdominal aortic aneurysm repair. Journal of vascular surgery, 2014, 60 (2): 301-307.
[2]Oderich GS, Correa MP, Mendes BC. Technical aspects of repair of juxtarenal abdominal aortic aneurysms using the Zenith fenestrated endovascular stent graft. Journal of vascular surgery, 2014, 59 (5): 1456-1461.
[3]Farber MA, Vallabhaneni R, Marston WA. "Off-the-shelf" devices for complex aortic aneurysm repair. Journal of vascular surgery, 2014, 60: 579-584.
[4]Quiñones-Baldrich WJ, Holden A, Mertens R, et al. Prospective,multicenter experience with the Ventana Fenestrated System for juxtarenal and pararenal aortic aneurysm endovascular repair. Journal of vascular surgery, 2013, 58: 1-9.
[5]Kitagawa A, Greenberg RK, Eagleton MJ, et al. Zenith p-branch standard fenestrated endovascular graft for juxtarenal abdominal aortic aneurysms. Journal of vascular surgery, 2013, 58: 291-300.
[6]Starnes BW. Physician-modified endovascular grafts for the treatment of elective, symptomatic, or ruptured juxtarenal aortic aneurysms. Journal of vascular surgery, 2012, 56: 601-607.
[7]Starnes BW, Tatum B. Early report from an investigatorinitiated investigational device exemption clinical trial on physician-modified endovascular grafts. Journal of vascular surgery, 2013, 58: 311-317.
[8]Ricotta JJ, Tsilimparis N. Surgeon-modified fenestratedbranched stent grafts to treat emergently ruptured and symptomatic complex aortic aneurysms in high-risk patients. Journal of vascular surgery, 2012, 56: 1535-1542.
[9]Wong S, Greenberg RK, Brown CR, et al. Endovascular repair of aortoiliac aneurysmal disease with the helical iliac bifurcation device and the bifurcated-bifurcated iliac bifurcation device. Journal of vascular surgery, 2013, 58: 861-869.
[10]Patel VI, Lancaster RT, Conrad MF, et al. Comparable mortality with open repair of complex and infrarenal aortic aneurysm. Journal of vascular surgery, 2011, 54: 952-959.
[11]Tallarita T, Sobreira ML, Oderich GS. Results of open pararenal abdominal aortic aneurysm repair: tabular review of the literature. Annals of vascular surgery, 2011, 25: 143-149.
[12]Ferrer C, De Crescenzo F, Coscarella C, et al. Early experience with the Excluder iliac branch endoprosthesis.Journal of cardiovascular surgery, 2014, 55: 679-683.
[13]Ricotta JJ, Tsilimparis N. Surgeon-modified fenestratedbranched stent grafts to treat emergently ruptured and symptomatic complex aortic aneurysms in high-risk patients. Journal of vascular surgery, 2012, 56: 1535-1542.
[14]Bisdas T, Donas KP, Bosiers M, et al. Anatomical suitability of the t-branch stent-graft in patients with thoracoabdominal aortic aneurysms treated using custom-made multibranched endografts. Journal of Endovascular Therapy, 2013, 20: 672-677.
[15]Bosiers MJ, Bisdas T, Donas KP, et al. Early experience with the first commercially available off-the-shelf multibranched endograft (t-branch) in the treatment of thoracoabdominal aortic aneurysms. Journal of Endovascular Therapy, 2013,20: 719-725.
Analysis and evaluation of endovascular interventional treatment of complex abdominal aortic aneurysm
LI Hao-cheng SHEN Yong-bin JIANG Wei-liang*
Department of Vascular Surgery, the 2nd Second Affiliated Hospital of Harbin Medical University, Harbin 150086, China
Objective Retrospectively analyse and evaluate the therapeutic effect of endovascular interventional technique in the treatment of complicated abdominal aortic aneurysm according to the patients' condition, preoperative examination, surgical methods, postoperative treatment measures and follow-up data. Methods Collecting the data which including the condition, preoperative examination, surgical methods, and postoperative treatment measures of patients who are treated in the department of vascular surgery, Second Affiliated Hospital of Harbin Medical Universityfrom 2011 January to 2015 June. Divided the patients into two groups: Complex abdominal aortic aneurysm patients group (A group), a total of 63 cases; abdominal aortic aneurysm patients group (B group), a total of 93 cases. Collate and summarize the clinical data of these patients. Results The success rates of the two groups were 100%. During the perioperation period and follow-up period, complicated abdominal aortic aneurysm group appeared 1 cases died. 11 cases of endoleaks was found in perioperative period. After treatment the endoleaks disappeared. 4 cases of endoleaks were found during follow-up period, only 1 case need treatment. The common type of abdominal aortic aneurysm group has no deaths occurred in the perioperative period and 14 cases of endoleaks occurred. Endoleaks disappeared after treatment. 6 cases appeared during the follow-up period. All of the endoleaks disappeared during the observation period. CTA examination showed that there were no significant stent shift occurred in the two groups after the operation and follow-up period. Conclusions There were no significant differences in the length of stay and operation time between the complex abdominal aortic aneurysm group and the common type of abdominal aortic aneurysm. The incidence rate of long-term survival rate and complication of complicated abdominal aortic aneurysm group and common type of abdominal aortic aneurysm group had no significant difference. Endovascular interventional techniques can be effective in the treatment of complex abdominal aortic aneurysm.
complex abdominal aortic aneurysm; endovascular repair of abdominal aortic aneurysm; complication
R656.5
A
2096-0646.2016.02.03.03
姜维良,E-mail:wljiang6666@sohu.com
