椎体成形术患者椎体再骨折的危险因素分析
2016-07-13李连华王浩桑庆华任继鑫刘智孙天胜
李连华 王浩 桑庆华 任继鑫 刘智 孙天胜
椎体成形术患者椎体再骨折的危险因素分析
李连华 王浩 桑庆华 任继鑫 刘智 孙天胜
【摘要】目的 通过对椎体成形术后的骨质疏松性椎体压缩骨折(osteop-orosis vertebral compression fracture,OVCF)患者的纵向回顾性研究,探讨发生再骨折的高危因素。方法 自 2012 年 7 月至 2014 年7 月,我科共应用椎体成形术治疗 OVCF 患者 220 例,分别采集患者的性别,年龄,骨密度,认知能力评分,骨水泥量,骨水泥渗漏,椎体后凸畸形,椎体再骨折等资料。应用单因素分析模型观察每种因素与椎体再骨折发生的相关性,筛查可疑的相关因素,接着采用 Logistic 回归分析明确与椎体再骨折发生相关的高危因素。结果 220 例椎体成形术的患者,共 334 个椎体,30 例(30 个椎体)发生再骨折,约占 9.0%。再骨折组年龄为(81.2±5.5)岁,非再骨折组年龄为(78±7.2)岁。认知功能评分 MMSE(mini-mental state examination)再骨折组为(23.2±9.03)分,非再骨折组为(27.48±5.27)分。椎体后凸畸形再骨折组为 40%,非再骨折组为16.32%。骨水泥渗漏再骨折组为 16.67%,非再骨折组为 7.37%。Logistic 回归分析显示年龄,认知功能评分,椎体术后后凸畸形,骨水泥渗漏等因素与椎体再骨折相关。结论 年龄,认知功能评分,椎体术后后凸畸形,骨水泥渗漏等因素是 OVCF 椎体成形术后再骨折的危险因素,应对危险人群加强再骨折风险的宣教及防护。
【关键词】椎体成形术;性骨折,压缩性;脊柱骨折;骨质疏松;危险因素fracturesL
随着社会的老龄化进程加速,骨质疏松患者越来越多,骨质疏松性骨折目前已成为老年患者的常见病、多发病。骨质疏松性椎体压缩骨折(osteoporosis vertebral compression fracture,OVCF)约占骨质疏松性骨折的 45%,导致患者疼痛、活动受限,严重时伴有出现脊柱畸形,影响心肺功能,导致死亡率增高[1]。
椎体成形术治疗 OVCF 的疗效越来越被人们所认可和接受,止痛效果在 90% 以上[2-3]。随着椎体成形术的广泛开展,椎体成形术后的椎体再骨折发生也越来越多[4-5]。本研究对 220 例行椎体成形术的OVCF 患者的进行纵向研究,探讨发生再骨折的高危因素。
资料与方法
一、纳入标准与排除标准
1. 纳入标准:(1)2012 年 7 月至 2014 年 7 月,我科收治的 OVCF 患者;(2)年龄≥55 岁;(3)新鲜 OVCF,疼痛剧烈(VAS≥7 分);(4)骨折经严格保守治疗 4 周症状缓解不满意;(5)椎体骨折进展风险较高者;(6)患者强烈要求手术。
2. 排除标准:(1)年龄<55 岁;(2)无症状的隐匿性骨折;(3)凝血机制障碍;(4)骨水泥或造影剂过敏;(5)局部感染;(6)患者心肺功能差,不能耐受手术。
二、随访与资料收集
随访方式采用对每位患者在术后常规进行4次门诊复查的方式(术后1、3、6、12个月),至少随访1年,随访满1年后,每半年对患者进行电话随访。对纳入的患者分别采集患者的性别,年龄,骨密度,认知能力评分,骨水泥量,骨水泥渗漏,椎体后凸畸形,椎体再骨折等资料。
认知能力采用简易智力状况检查法(mini-mental state examination,MMSE)评分从定向力,记忆力,注意力和计算能力,回忆能力,语言能力5个方面对认知能力进行评估,最高得分为30分,分数在27~30分为正常,分数<27为认知功能障碍[6]。
三、统计学分析
应用SPSS 18.0软件进行统计分析,计量资料采用独立样本t检验,计数资料采用卡方检验,单因素模型观察每种因素差异的统计学意义;将单因素中P<0.1列为潜在危险因素,采用Logistic回归分析明确与椎体再骨折发生相关的高危因素,将P<0.05设为差异有统计学意义。
结 果
符合本研究纳入标准者共220例(334个椎体),其中男146例,女74例;年龄 65~95岁,平均78.45岁;骨折椎体包括T9~L5,至少随访1年。其中30例发生椎体再骨折,占 13.6%,共30个椎体,男女比例为11∶19,年龄69~94岁,平均81.37岁,再骨折椎体包括 T11~L2,邻近椎体骨折与非临近椎体比例为13∶17。再骨折发生在第1次术后随访期间1例,第2次术后随访期间9例,第3次术后随访期间8例,第4次术后随访期间4例,发生在手术后1年8例(最长术后10年)。
将30例椎体再发骨折者(再骨折组)与190例无椎体再发骨折者(无再骨折组)进行比较。
单因素回归分析显示,椎体再发骨折组无椎体再发骨折组的年龄(P<0.01)、认知状态(P<0.01)及后凸畸形(P<0.01)与再骨折相关,而性别、骨密度、骨水泥量、骨水泥椎间隙渗漏等因素无明显相关(表1)。进一步多因素回归分析结果发现,年龄(OR=0.925,P=0.018)、MMSE评分(OR=1.072,P=0.013)、后凸畸形(OR=0.384,P=0.044)及骨水泥渗漏(OR=0.306,P=0.049)是导致椎体成形术后再骨折的危险因素(表2)。
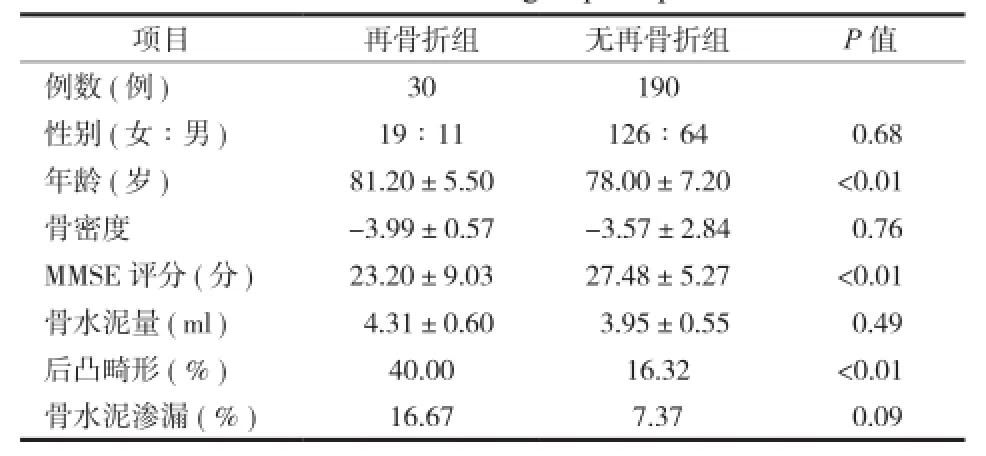
表1 患者一般资料Tab.1 General information of the 2 groups of patients
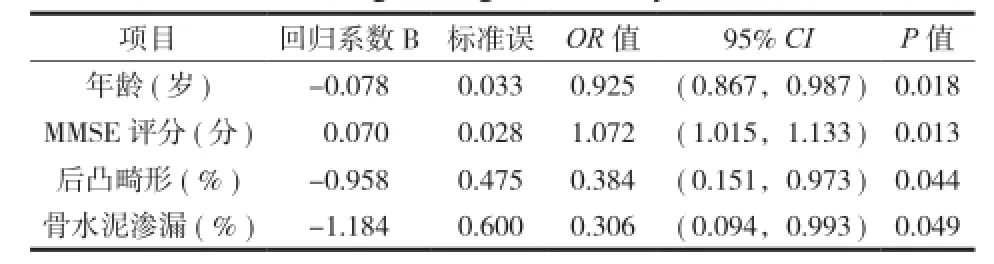
表2 Logistic 回归分析结果Tab.2 Results of the Logistic regression analyses
讨 论
导致椎体成形术后椎体再骨折发生的可能因素有很多,较多的文献关注高龄[7],邻近椎体骨折[8],骨水泥剂量[9],骨水泥分布[10],骨水泥椎间隙渗漏[11],骨密度[12],脊椎力线异常[13]等因素。
2011 年,Fahim 等[14]进行的尸体研究发现,椎体成形术后改变了前柱的应力状态,使得椎体承受应力的能力下降 32%,容易发生再次骨折。但也有学者的生物力学研究证实,椎体成形术后并不对邻近椎体的椎板造成过多的应力,因此不会导致邻近椎体骨折的发生[15]。也有文献报道,与保守治疗相比较,椎体成形术并不增加其它椎体骨折的风险[16-17]。本研究中发生的再骨折部位,仅 40% 发生于邻近节段,也间接说明椎体成形术本身不大可能是导致再骨折的因素。
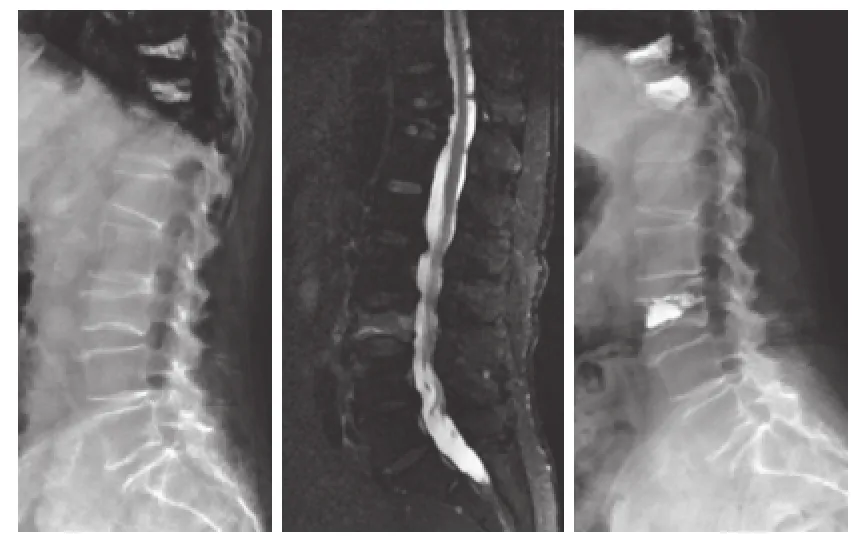
图1 患者,女,81 岁,老年痴呆,因椎体压缩骨折行 T10、11椎体成形术后,术后8个月L3发生椎体再骨折,行椎体成形术后Fig.1 New vertebral compression fracture at L3occurred 8 months after osteoporotic compression fracture of T10and T11. The patient was an 81 years old female who was diagnosed as Alzheimer's disease. She had been performed vertebroplasty becaurse of of osteoporotic compression fractureof. later the and the vertebroplasty was performed again
本研究发现,认知能力下降是导致椎体成形术后再骨折的危险因素。认知能力下降是指涉及学习记忆以及思维判断有关的大脑高级智能加工过程出现异常,从而引起学习、记忆障碍同时伴有失语、失用、失认或失行等改变的病理过程。认知能力下降后,患者对于在发生危害自己健康的行为时不能自我感知,因此容易发生骨折(图1)。有学者研究发现,认识能力下降是髋部骨折发生的危险因素之一[18]。
本研究中得出的高龄,后凸畸形及骨水泥渗漏是导致椎体成形术后再骨折的危险因素,高龄患者意味着身体素质更加衰弱,而后凸畸形和骨水泥渗漏都改变了椎体的应力负重状态,导致再骨折的发生,这与其他学者的研究结果相一致[7,11,13]。
总之,随着椎体成形术的不断广泛应用,发生再骨折的患者会越来越多,对于高龄,认知功能障碍,后凸畸形及骨水泥渗漏的患者,要警惕发生再骨折的危险,及早做好防护。另外,还有其它一些重要因素未纳入本研究中,这些因素之间的相互联系还需在以后多中心的研究中进一步探索。
参 考 文 献
[1]Lyritis GP, Mayasis B, Tsakalakos N, et al. The natural history of the osteoporotic vertebral fracture. Clin Rheumatol, 1989,8(Suppl 2):S66-69.
[2]Alexandru D, So W. Evaluation and management of vertebral compression fractures. Perm J, 2012, 16(4):46-51.
[3]Li L, Ren J, Liu J, et al. Results of vertebral augmentation treatment for patients of painful osteoporotic vertebral compression fractures: A Meta-analysis of eight randomized controlled trials. PLoS One, 2015, 10(9):e0138126.
[4]Al-Nakshabandi NA. Percutaneous vertebroplasty complications. Ann Saumed, 2011, 31(3):294-297.
[5]李智斐, 钟远鸣. 椎体成形术后再骨折相关因素研究进展. 中国矫形外科杂志, 2013, 21(18):1844-1847.
[6]Mitchell AJ, Shukla D, Ajumal HA, et al. The Mini-Mental State Examination as a diagnostic and screening test for delirium: systematic review and meta-analysis. Gen Hosp Psychiatry, 2014, 36(6):627-633.
[7]Ma X, Xing D, Ma J, et al. Risk factors for new vertebral compression fractures after percutaneous vertebroplasty:qualitative evidence synthesized from a systematic review. Spine, 2013, 38(12):E713-722.
[8]Tanigawa N, Komemushi A, Kariya S, et al. Radiological follow-up of new compression fractures following percutaneous vertebroplasty. Cardiovasc Intervent Radiol, 2006, 29(1):92-96.
[9]余鹏, 夏群, 皮红林, 等. 经皮椎体成形术后相邻椎体再骨折的相关因素. 中华创伤杂志, 2013, 29(11):1063-1067.
[10]Liu WG, He SC, Deng G, et al. Risk factors for new vertebral fractures after percutaneous vertebroplasty in patients with osteoporosis: a prospective study. J Vasc Interv Radiol, 2012,23(9):1143-1149.
[11]Nieuwenhuijse MJ, Putter H, van Erkel AR, et al. New vertebral fractures after percutaneous vertebroplasty for painful osteoporotic vertebral compression fractures: a clustered analysis and the relevance of intradiskal cement leakage. Radiology, 2013, 266(3):862-870.
[12]Sun G, Tang H, Li M, et al. Analysis of risk factors of subsequent fractures after vertebroplasty. Eur Spine J, 2014, 23(6):1339-1345.
[13]Lee WS, Sung KH, Jeong HT, et al. Risk factors of developing new symptomatic vertebral compression fractures after percutaneous vertebroplasty in osteoporotic patients. Eur Spine J, 2006, 15(12):1777-1183.
[14]Fahim DK, Sun K, Tawackoli W, et al. Premature adjacent vertebral fracture after vertebroplasty: a biomechanical study. Neurosurgery, 2011, 69(3):733-744.
[15]Aquarius R, van der Zijden AM, Homminga J, et al. Does bone cement in percutaneous vertebroplasty act as a stress riser?Spine, 2013, 38(24):2092-2097.
[16]Chosa K, Naito A, Awai K. Newly developed compression fractures after percutaneous vertebroplasty: comparison with conservative treatment. Jpn J Radiol, 2011, 29(5):335-341.
[17]Zou J, Mei X, Zhu X, et al. The long-term incidence of subsequent vertebral body fracture after vertebral augmentation therapy: a systemic review and meta-analysis. Pain Physician,2012, 15(4):E515-522.
[18]Tseng WJ, Hung LW, Shieh JS, et al. Hip fracture risk assessment: artificial neural network outperforms conditional logistic regression in an age- and sex-matched case control study. BMC Musculoskelet Disord, 2013, 14:207.
(本文编辑:李贵存)
. 综述 Review .
DOI:10.3969/j.issn.2095-252X.2016.06.006中图分类号:R683.2, R687.3
作者单位:100700 北京,陆军总医院骨科
收稿日期:(2016-02-14)
Risk factors of subsequent fractures after vertebroplasty in patients with osteoporotic vertebral compression
LI Lian-hua, WANG Hao, SANG Qing-hua, REN Ji-xin, LIU Zhi, SUN Tian-sheng.
Chinese People's ibration Army Institute of Orthopedics, Beijing Military Command General Hospital, Beijing, 100700, PRC
【Abstract 】Objective To explore the risk factors that may affect the development of subsequent fractures after vertebroplasty in patients with osteoporotic vertebral compression fractures. Methods A retrospective study was conducted to review 220 patients who underwent vertebroplasty for osteoporotic vertebral compression fractures from July 2012 to July 2014. Clinical data including age, gender, bone mineral density(BMD)T-score, cognitive ability scores, the amount of injected bone cement, cement leakage, vertebral kyphosis deformity and subsequent fractures were recorded. Univariate analysis was performed to screen the suspicious factors and Logistic regression analysis were used to assess the relations between the suspicious factors and the incidence of subsequent fractures. Results Thirty of the 220 patients(9.0%)experienced subsequent fractures. Average age was(81.2 ± 5.5)in patients with subsequent fractures and(78 ± 7.2)in patients without subsequent fractures. Average mini-mental state examination(MMSE)score was(23.2 ± 9.03)in patients with subsequent fractures and(27.48 ± 5.27)in patients without subsequent fractures. The percentage of vertebral kyphosis deformity was 40% in patients with subsequent fractures and 16.32% in patients without subsequent fractures. The percentage of cement leakage was 16.67% in patients with subsequent fractures and 7.37% in patients without subsequent fractures. Logistic regression analysis showed that the risk factors infuencing subsequent fractures were age, MMSE score, vertebral kyphosis deformity and bone density and cement leakage. Conclusions Age, MMSE score, vertebral kyphosis deformity and bone cement leakage were the independent risk factors associated with subsequent fractures after vertebroplasty in patients with osteoporotic vertebral compression fractures. For people with these risk factors more efforts should be made to protect subsequent fracture.
【Key words】Vertebroplasty; Fractures, compression; Spinal fractures; Osteoporosis; Risk factors