Experimental study on the inhibition effect of m iR-106a inhibitor on tumor grow th of ovarian cancer xenografts m ice
2016-06-29ZhiHuiCaiLiMinChenYiJuanLiangJunRongShiYouJuMaeiMingWangHuanYang
Zhi-Hui Cai, Li-Min Chen*, Yi-Juan Liang, Jun-Rong Shi, You-Ju Ma, W ei-Ming Wang, Huan Yang
1Gynecology Department, Affiliated Hospital of Hebei University, Baoding City 071000, Hebei Province, China2Gynecology and Obstetrics Department, Jingxiu district hospital of Baoding city, Baoding City 071000, Hebei Province, China
Experimental study on the inhibition effect of m iR-106a inhibitor on tumor grow th of ovarian cancer xenografts m ice
Zhi-Hui Cai1, Li-Min Chen1*, Yi-Juan Liang1, Jun-Rong Shi1, You-Ju Ma1, W ei-Ming Wang1, Huan Yang2
1Gynecology Department, Affiliated Hospital of Hebei University, Baoding City 071000, Hebei Province, China
2Gynecology and Obstetrics Department, Jingxiu district hospital of Baoding city, Baoding City 071000, Hebei Province, China
AR T ICLE IN FO
Article history:
Received 15 April 2016
Received in revised form 16 May 2016 Accepted 15 June 2016
Available online 20 July 2016
Keywords:
Ovarian cancer
Xenografts
m iR-106a
Programmed cell death 4
ABSTRACT
Objective: To study the inhibition effect of miR-106a inhibitor on tumor grow th of ovarian cancer xenografts mice. Methods: BALB/c m ice were selected as experimental animals,ovarian cancer SKOV-3 cells transfected with m iR-106a inhibitor and its negative control were inoculated subcutaneously, intratumoral injection of miR-106a inhibitor and its negative control were continued after tumor formation, and they were enrolled as treatment group and model group, respectively. Tumor volume and weight as well as Ki-67 and programmed cell death 4 (PDCD4) expression were determ ined; miR-106a inhibitor and its negative control as well as m iR-106a m im ic and its negative control were transfected into SKOV-3 cells, and expression of PDCD4 in cells was determ ined. Results: Tumor tissue volume and weight as well as mRNA expression and protein expression of Ki-67 in treatment group were significantly lower than those in the model group while mRNA expression and protein expression of PDCD4 were significantly higher than those in the model group; transfection of m iR-106a m im ic could decrease mRNA expression and protein expression of PDCD4 in SKOV-3 cells, and transfection of m iR-106a inhibitor could increase mRNA expression and protein expression of PDCD4 in SKOV-3 cells. Conclusions: Transfection of m iR-106a inhibitor can inhibit the grow th of tumor in ovarian cancer xenografts m ice through increasing the expression of PDCD4.
Tel: 15932260538
E-mail: 304153929@qq.com
Foundation project: This research was supported by Science and Technology Program of Hebei Province in 2013 (No. 132777163).
1. Introduction
Ovarian cancer is one of the common malignant tumors of female reproductive system, and the death caused by ovarian cancer ranks first in gynecologic malignant tumors. Ovarian cancer patients can obtain complete remission after cytoreductive surgery and adjuvant chemotherapy, but the overall prognosis is still poor, and there w ill be local recurrence and distant metastasis in vast majority of patients[1,2]. Ovarian cancer involves many links, genes and steps,and the inactivation of tumor suppressor genes and activation of proto-oncogene as well as abnormal expression of apoptosis-related genes and invasion-related genes can all cause tumor recurrence and metastasis[3,4]. However, the upstream signals regulating the expression of above malignant tumor-related genes are still not clarified at present, and accurate targets for the clinical treatment of ovarian cancer are also scarce. MicroRNA (m iRNA) is a fam ily of evolutionarily highly conserved non-coding small molecule RNA found in recent years, which is combined with target gene mRNA 3’ untranslated region (3’UTR) so as to regulate the expression of multiple genes[5,6]. Studies have confirmed that m iR-106a has the characteristics of proto-oncogene, and participates in the occurrence and development of lung cancer[7], gastric cancer[8], colon cancer[9]and many other kinds of malignant tumors, thus it was speculated in the study whether m iR-106a was also involved in the occurrence and development of ovarian cancer, and whether inhibiting the biological functions of miR-106a could inhibit the grow th of ovariancancer. In the follow ing study, transfection of m iR-106a inhibitor was adopted to inhibit the biological effect of m iR-106 in tumor cells, and then the tumor grow th in ovarian cancer xenografts mice was analyzed.
2. Materials and methods
2.1. Experimental materials
Human ovarian cancer SKOV3 cell lines were bought from the cell center of Union Medical College, RPM I1640 medium and fetal bovine serum were purchased from Gibco Company, m iR-106a m im ic and negative control as well as m iR-106a inhibitor and negative control were synthesized by Genepharma Company (Shanghai), and Lipofectam ine 2000 transfection reagents were purchase from Invitrogen Company (USA). RNA extraction kits,reverse transcription kits and fluorescence quantitative PCR kits were bought from Tiangen Biotech Company (Beijing), and Elisa kits were purchased from Westang Biotech Company (Shanghai).
Twenty SPF female BALB/c m ice with body mass (18-24) g were bought and raised by the animal center of Hebei University, they were raised under constant temperature (18-22) ℃ and constant humidity 50%-80%, and they had free water and feeding. Mice were random ly divided into model group and treatment group, 10 in each group. The animal experiment was approved by the ethics comm ittee of Affiliated Hospital of Hebei University.
2.2. Experimental methods
2.2.1. Cell culturing and transfection of miR-106a inhibitor
SKOV3 cell lines were recovered and then cultured in RPM I1640 medium containing 10% fetal bovine serum, cells were digested and sub-cultured with 0.25% trypsin after grow ing all over, then they were respectively inoculated in culture bottle and Petri dishes, cells in the culture bottles were used for continuous digestion and passage,cells in the Petri dishes were used for processing, and the methods were as follows: m iR-106a inhibitor, miR-106a mimic, NC inhibitor and NC mimic powder was configured to 20 μmol/L solution, and the proportion of 6 μL Lipofectamine2000 and 3 μL miR inhibitors or m im ics per 1 m L medium was followed for transfection for consecutive 24 h.
2.2.2. Establishment and intervention methods of xenografts mice
SKOV-3 cells transfected with m iR-106a inhibitors or NC inhibitors were taken and digested to get cell suspension, the cell density was adjusted to 107/mL, model group received subcutaneous injection of 0.5 m L SKOV-3 cell suspension transfected with NC inhibitor into the right upper extrem ity axillary lateral side,treatment group received subcutaneous injection of 0.5 m L SKOV-3 cell suspension transfected with m iR-106a inhibitor into the right upper extrem ity axillary lateral side, and after 7 d, those with tumor size more than 3mm3 were successfully established xenografts models and then received the follow ing intervention: on the 7th day after local injection of SKOV-3 cell suspension, model group received intratumoral injection of 5 μL NC inhibitor + 5 μL Lipofectam ine2000 m ixture, treatment group received intratumoral injection of 5 μL m iR-106a inhibitor + 5 μL Lipofectam ine2000 mixture, once every four days, for a total of 10 times.
2.2.3. Assessment of tumor growth
On the 7th day after local injection of SKOV-3 cell suspension as well as the 10th day, 20th day, 30th day and 40th day after local injection of miR-106a inhibitor, vernier caliper was used to measure the maximum major diameter (a) and the maximum transverse diameter (b) of tumor, the maximum transverse diameter referred to the maximum length of the line perpendicular to the maximum major diameter, and tumor tissue volume V=0.5×a×b2. On the 40th day after local injection of m iR-106a inhibitor or NC inhibitor,the volume of tumor tissue was measured, and then the m ice were executed and anatomized to obtain and weigh tumor tissue.
2.2.4. Fluorescence quantitative PCR detection methods
Extraction of RNA in cells was by total RNA extraction kit for cells, extraction of RNA in tumor tissue was by total RNA extraction kit for animal tissue, RNA was obtained and then reverse-transcribed into cDNA by reverse transcription Kit TIANScript Ⅱ RT Kit, then fluorescence quantitative PCR Kit was used to amplify Ki-67 and programmed cell death 4 (PDCD4) genes as well as β-actin, and amplification conditions were as follows: 95 ℃ initial denaturation 5min, 95 ℃ 30 s, specific annealing temperature 30 s, 72 ℃ 30 s and repeating for 40 cycles, and after amplification curve was obtained,2- Ct formula was followed to calculate the relative mRNA levels of Ki-67 and PDCD4.
2.2.5. Elisa detection methods
Treated SKOV3 cells were collected, added in protein lysis buffer,fully broken and centrifuged to get protein suspension; tumor tissue was collected, added in PBS, fully grinded and centrifuged to get protein suspension. Elisa kits for PDCD4 and Ki-67 were used to determine protein content.
2.2.6. Statistical methods
SPSS20.0 softw are w as used to input and analyze data,measurement data comparison between two groups was by t test and P<0.05 indicated statistical significance in differences.
3. Results
3.1. Tumor tissue growth
On the 7th day after local injection of SKOV-3 cell suspension (the time of tumor formation), tumor tissue volume in treatment group was significantly lower than that in the model group; on the 10thday, 20th day, 30th day and 40th day after treatment, tumor volume of both groups gradually increased, and tumor tissue volume in treatment group at various points in time were significantly lower than those in the model group; m ice were executed and anatom ized to get tumor tissue, and tumor tissue weight in treatment group was significantly lower than that in the model group, shown in Table 1.
3.2. Ki-67 expression in tumor tissue
Detection of Ki-67 mRNA expression in tumor tissue of model group and treatment group by fluorescence quantitative PCR showed that mRNA level of Ki-67 in tumor tissue of treatment group was (0.26±0.05) vs. (1.00±0.17) and significantly lower than that of the model group; detection of Ki-67 protein expression in tumor tissue of model group and treatment group by Elisa showed that protein level of Ki-67 in tumor tissue of treatment group was (35.96±6.13)vs. (127.75±21.45) μg/mg total protein and significantly lower than that of the model group.
3.3. PDCD4 expression in tumor tissue
Detection of PDCD4 mRNA expression in tumor tissue of model group and treatment group by fluorescence quantitative PCR showed that mRNA level of PDCD4 in tumor tissue of treatment group was (2.86±0.61) vs. (1.00±0.19) and significantly higher than that of the model group; detection of PDCD4 protein expression in tumor tissue of model group and treatment group by Elisa showed that protein level of PDCD4 in tumor tissue of treatment group was (186.36±31.56) vs. (42.84±7.12) μg/mg total protein and significantly higher than that of the model group.
3.4. PDCD4 expression in SKOV-3 cells
A fter transfection of m iR-106a m im ic and NC m imic, analysis of PDCD4 expression in SKOV-3 cells was as follows: compared with cells transfected with NC m im ic, mRNA content of PDCD4 (0.48±0.08) vs. (1.00±0.11) and protein content of PDCD4 (15.61±2.32) vs. (34.47±5.28) μg/mg total protein significantly decreased in cells transfected with m iR-106a m im ic. A fter transfection of m iR-106a inhibitor and NC inhibitor, analysis of PDCD4 expression in SKOV-3 cells was as follows: compared with cells transfected with NC inhibitor, mRNA content of PDCD4 (2.52±0.42) vs. (1.00±0.14) and protein content of PDCD4 (70.25±10.38) vs. (37.23±6.13) μg/mg total protein significantly increased in cells transfected with miR-106a inhibitor.
4. Discussion
Metastasis, recurrence rate and mortality rate are high in ovarian cancer patients after cytoreductive surgery and adjuvant chemotherapy, and the inactivation of tumor suppressor genes and the activation of proto-oncogene as well as abnormal expression of apoptosis-related genes and invasion-related genes are all closely related to the recurrence and metastasis of ovarian cancer. m iRNA is a class of small non-coding RNA with length of (22-25) bp, and can be combined with target gene mRNA 3’UTR region to lead to mRNA degradation or inhibit mRNA translation[10,11]. In the occurrence and development of malignant tumor, some fragile area in chromosomes can change, and more than 50% of the m iRNA genes are in the fragile area of chromosomes and with abnormal expression, resulting in changes in the expression of a variety of downstream target genes and causing corresponding changes in cell biological behavior[12,13].
m iR-106a is a class of miRNA with proto-oncogene properties found in recent years, and it shows the trend of high expression in lung cancer[7], gastric cancer[8], colon cancer[9] and many other malignant tumor tissues. Experimental cell research of domestic LI Min and others[14] confirms that miR-106 is highly expressed in metastatic ovarian cancer cells SKOV-3 and m iR-106a m im ic can promote ovarian cancer cell m igration and invasion in vitro. So it was speculated that miR-106a had promoting effect on the occurrence and development of ovarian cancer, and antagonizing the biological function of m iR-106a in cells could inhibit the development of ovarian cancer. But relevant study in vivo on the relationship between miR-106a and the occurrence and development of ovarian cancer is still scarce at present.
In this study, transfection of m iR-106a inhibitor was adopted to antagonize the biological effect of m iR-106a in ovarian cancer cells,and after subcutaneous injection of ovarian cancer cells transfected with miR-106a inhibitor and NC inhibitor, observation of the tumor formation showed that at the time of tumor formation, tumor tissue volume of treatment group was significantly less than that of model group. That means that after subcutaneous injection of ovarian cancer cells transfected with m iR-106a inhibitor into mice, tumor volume is smaller at the time of tumor formation. In the process of tumor grow th, continuous intratumoral injection of m iR-106a inhibitor can further inhibit tumor grow th, and tumor tissue volume of treatment group on the 10th day, 20th day, 30th day and 40th day after injection were significantly less than those of model group and the weight of tumor tissue from anatom izing executed m ice was significantly lower than that of model group. Ki-67 is a nuclear antigen located in the nucleus and can reflect the cell proliferationactivity, and analysis of Ki-67 expression in tumor tissue in the research confirmed that mRNA expression and protein expression of Ki-67 in tumor tissue of treatment group were significantly lower than those of the model group. Thus it further confirms that transfection of m iR-106a inhibitor can inhibit the grow th of ovarian cancer, reduce tumor volume and reduce tumor weight.
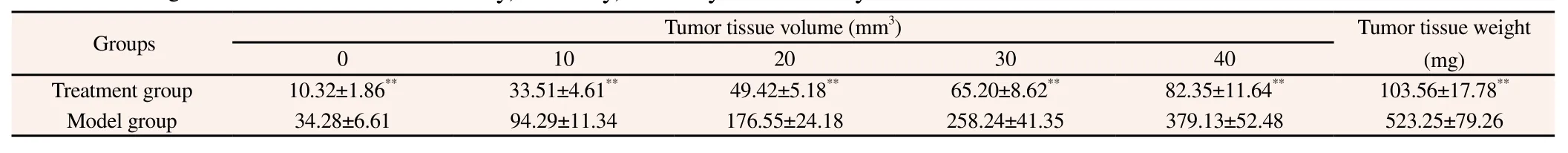
Table 1 Volume and weight of tumor tissue on the 10th day, 20th day, 30th day and 40th day after treatment.
The way for miRNA to regulate gene expression is to be combined with target gene mRNA 3’UTR to induce mRNA degradation and inhibit mRNA translation. Studies have reported that PDCD4 is an important tumor suppressor gene in the body[15-17] and also a target gene regulated by miR-106a[18]. Protein encoded by PDCD4 contains two highly conserved α-helical MA-3 domains, can interact with RNA helicase and eIF4A protein, and can also adjust the phosphorylation status of a variety of downstream signaling molecules, thus inhibiting cell proliferation and invasion[19,20]. Research of Wei N[21] shows that PDCD4 expression decreases significantly and anticancer activity is lost in ovarian cancer tissue. In the research, analysis of PDCD4 expression in tumor tissue confirmed that after transfection of m iR-106a inhibitor,PDCD4 expression in tumor tissue increased significantly. Thus it demonstrates that m iR-106a can adjust the expression of PDCD4 in ovarian cancer tissue, thereby affecting the grow th of tumor. In order to further define whether miR-106a directly regulated PDCD4 expression, miR-106a m imic and inhibitor were transfected into ovarian cancer cells respectively in the study, and analysis of mRNA and protein expression of PDCD4 showed that m iR-106a m im ic could inhibit PDCD4 expression and the inhibitor could increase PDCD4 expression. It indicates that m iR-106a can target and regulate PDCD4 expression in ovarian cancer cells.
To sum up, transfection of m iR-106a inhibitor can inhibit the grow th of tumor in ovarian cancer xenografts m ice through increasing the expression of PDCD4.
Conflict of interest statement
We declare that we have no conflict of interest.
References
[1] Nasioudis D, Sisti G, Kanninen TT, Holcomb K, Di Tommaso M,Fambrini M, et al. Epidem iology and outcomes of squamous ovarian carcinoma; a population-based study. Gynecol Oncol 2016; 141(1): 128-133.
[2] Tanaka YO, Okada S, Satoh T, Matsumoto K, Oki A, Saida T, et al. Differentiation of epithelial ovarian cancer subtypes by use of imaging and clinical data: a detailed analysis. Cancer Imaging 2016; 16(1): 3.
[3] Javadi S, Ganeshan DM, Qayyum A, Iyer RB, Bhosale P. Ovarian Cancer,the Revised FIGO Staging System, and the Role of Imaging. AJR Am J Roentgenol 2016; 4: 1-10.
[4] Hemm inki K, Sundquist K, Sundquist J, Hemm inki A, Ji J. Location of metastases in cancer of unknown primary are not random and signal familial clustering. Sci Rep 2016; 9(6): 22891.
[5] Seviour EG, Sehgal V, Lu Y, Luo Z, Moss T, Zhang F, et al. Functional proteomics identifies miRNAs to target a p27/Myc/phospho-Rb signature in breast and ovarian cancer. Oncogene 2016; 35(6): 801.
[6] Wu RL, A li S, Bandyopadhyay S, A losh B, Hayek K, Daaboul MF, et al. Comparative analysis of differentially expressed m irnas and their downstream m rnas in ovarian cancer and its associated endometriosis. J Cancer Sci Ther 2015; 7(7): 258-265.
[7] Xie X, Liu HT, Mei J, Ding FB, Xiao HB, Hu FQ, et al. m iR-106a promotes grow th and metastasis of non-small cell lung cancer by targeting PTEN. Int J Clin Exp Pathol 2015; 8(4): 3827-3834.
[8] Hou X, Zhang M, Qiao H. Diagnostic significance of m iR-106a in gastric cancer. Int J Clin Exp Pathol 2015; 8(10): 13096-13101.
[9] Catela Ivkovic T, Aralica G, Cacev T, Loncar B, Kapitanovic S. miR-106a overexpression and pRB downregulation in sporadic colorectal cancer. Exp Mol Pathol 2013; 94(1): 148-154.
[10] Nagaraj AB, Joseph P, DiFeo A. miRNAs as prognostic and therapeutic tools in epithelial ovarian cancer. Biomark Med 2015; 9(3): 241-257.
[11] Zhang S, Lu Z, Unruh AK, Ivan C, Baggerly KA, Calin GA, et al. Clinically relevant m icroRNAs in ovarian cancer. Mol Cancer Res 2015;13(3): 393-401.
[12] Zhao S, Wen Z, Liu S, Liu Y, Li X, Ge Y, et al. MicroRNA-148a inhibits the proliferation and promotes the paclitaxel-induced apoptosis of ovarian cancer cells by targeting PDIA3. Mol Med Rep 2015; 12(3): 3923-3929.
[13] Zhao HM, Wei W, Sun YH, Gao JH, Wang Q, Zheng JH. MicroRNA-9 promotes tumorigenesis and mediates sensitivity to cisplatin in primary epithelial ovarian cancer cells. Tumour Biol 2015; 36(9): 6867-6873.
[14] LI M, Zhang XN, Wei Y, Yang C, Dong TT, Li J. m icroRNA-106a promotes the migration and invasion of epithelial ovarian cancer cell lines. Prog Obstet Gynecol 2015; 24(11): 809-814.
[15] Chen Z, Yuan YC, Wang Y, Liu Z, Chan HJ, Chen S. Down-regulation of programmed cell death 4 (PDCD4) is associated with aromatase inhibitor resistance and a poor prognosis in estrogen receptor-positive breast cancer. Breast Cancer Res Treat 2015; 152(1): 29-39.
[16] Vikhreva PN, Korobko IV. Expression of Pdcd4 tumor suppressor in human melanoma cells. Anticancer Res 2014; 34(5): 2315-2318.
[17] Biyanee A, Ohnheiser J, Singh P, Klempnauer KH. A novel mechanism for the control of translation of specific mRNAs by tumor suppressor protein Pdcd4: inhibition of translation elongation. Oncogene 2015;34(11): 1384-1392.
[18] Li H, Xu H, Shen H, Li H. m icroRNA-106a modulates cisplatin sensitivity by targeting PDCD4 in human ovarian cancer cells. Oncol Lett 2014; 7(1): 183-188.
[19] Singh P, Marikkannu R, Bitomsky N, Klempnauer KH. Disruption of the Pdcd4 tumor suppressor gene in chicken DT40 cells reveals its role in the DNA-damage response. Oncogene 2009; 28(42): 3758-3764.
[20] Modelska A, Turro E, Russell R, Beaton J, Sbarrato T, Spriggs K, et al. The malignant phenotype in breast cancer is driven by eIF4A1-mediated changes in the translational landscape. Cell Death Dis 2015; 22(6): e1603. [21] Wei N, Liu SS, Chan KK, Ngan HY. Tumour suppressive function and modulation of programmed cell death 4 (PDCD4) in ovarian cancer. PLoS One 2012; 7(1): e30311.
doi:Document heading 10.1016/j.apjtm.2016.05.008
*Corresponding author:Li-Min Chen, Gynecology Department, A ffiliated Hospital of Hebei University, Yuhua East Road, Baoding City, Hebei Province
杂志排行
Asian Pacific Journal of Tropical Medicine的其它文章
- Effects of scallop shell extract on scopolam ine-induced memory impairment and MK801-induced locomotor activity
- Predicted pattern of Zika virus infection distribution with reference to rainfall in Thailand
- H igh seroprevalence of asymptomatic viral haemoparasites among prospective blood donors in N igeria
- Evaluation of hypoxia inducible factor targeting pharmacological drugs as antileishmanial agents
- Molecular epidem iology and phylogeny of N ipah virus infection: A m ini review
- Green coffee bean extract improves obesity by decreasing body fat in high-fat diet-induced obese m ice
