Surgically induced changes in retinal vessel diameter, retinal nerve fiber layer thickness, and the optic disc after 23-gauge vitreoretinal surgical procedures
2016-05-17SeungUkLeeSuJinKimSangJoonLee
Seung Uk Lee, Su Jin Kim, Sang Joon Lee
1Department of Ophthalmology, College of Medicine, Kosin University, Busan 49267, Korea
2Department of Ophthalmology, College of Medicine, Gyeongsang National University, Gyeongsangnamdo 52727, Korea
Correspondence to:Sang Joon Lee. Department of Ophthalmology, College of Medicine, Kosin University, #34 Amnam-dong, Suh-ku, Busan 49267, Korea. hhiatus@gmail.com
Received: 2015-09-11 Accepted: 2016-03-02
23G玻璃体视网膜手术后视网膜血管直径与神经纤维层厚度及视盘的变化
Seung Uk Lee1, Su Jin Kim2, Sang Joon Lee1
(作者单位:1韩国,釜山 49267,高神大学,医学院,眼科;2韩国,慶尙南道 52727,慶尙大学,医学院,眼科)
Surgically induced changes in retinal vessel diameter, retinal nerve fiber layer thickness, and the optic disc after 23-gauge vitreoretinal surgical procedures
Seung Uk Lee1, Su Jin Kim2, Sang Joon Lee1
1Department of Ophthalmology, College of Medicine, Kosin University, Busan 49267, Korea
2Department of Ophthalmology, College of Medicine, Gyeongsang National University, Gyeongsangnamdo 52727, Korea
Correspondence to:Sang Joon Lee. Department of Ophthalmology, College of Medicine, Kosin University, #34 Amnam-dong, Suh-ku, Busan 49267, Korea. hhiatus@gmail.com
Received: 2015-09-11Accepted: 2016-03-02
23G玻璃体视网膜手术后视网膜血管直径与神经纤维层厚度及视盘的变化
Seung Uk Lee1, Su Jin Kim2, Sang Joon Lee1
(作者单位:1韩国,釜山 49267,高神大学,医学院,眼科;2韩国,慶尙南道 52727,慶尙大学,医学院,眼科)
Abstract
•AIM:To investigate the retinal vascular caliber, retinal nerve fiber layer(RNFL) thickness, and optic disc changes in patients after pars plana vitrectomy and adjunctive intraoperative procedures.
•METHODS:We examined 40 eyes in 40 patients who had undergone unilateral pars plana vitrectomy and adjunctive intraoperative procedure at three time points:prior to surgery, and at 3mo and 6mo after the operation. The diameters of central retinal arteries and veins were measured using retinal photographs. The central retinal arteriolar equivalent(CRAE) and central retinal venular equivalent(CRVE) were calculated using the revised Parr-Hubbard formula. RNFL thickness was obtained using Stratus optical coherence tomography. The cup-to-disc vertical ratio of the optic disc was evaluated using stereo optic disc photography.
•RESULTS:There were no significant differences between the eyes of individual patients before the operation. Cup-to-disc vertical ratios of the optic disc were significantly increased 3mo and 6mo postoperatively(P<0.01,P<0.01), and there was a significant difference between the operative eye and fellow eye at the same time points(P<0.01,P<0.01). Changes in CRAE and CRVE in the operative eyes were significantly larger than the fellow eyes 6mo post-operatively(P<0.01,P<0.01). The RNFL thickness showed no significant changes.
•CONCLUSION:Whereas there were no changes in RNFL thickness, vitrectomy and adjunctive intraoperative procedures induced changes in the cup-to-disc vertical ratio of the optic disc and retinal vessel diameter for at least 6mo after surgery.
KEYWORDS:•retinal vessel diameter;retinal nerve fiber layer thickness;optic disc;vitrectomy
Citation:Lee SU, Kim SJ, Lee SJ. Surgically induced changes in retinal vessel diameter, retinal nerve fiber layer thickness, and the optic disc after 23-gauge vitreoretinal surgical procedures.GuojiYankeZazhi(IntEyeSci) 2016;16(5):801-806
INTRODUCTION
Advancements in both vitreoretinal surgical techniques and instruments have expanded the indications for vitrectomy, making this surgical procedure more popular. The introduction of 23-gauge pars plana vitrectomy in particular as an early surgical intervention has become more widely accepted. Some previous studies have indicated that after vitrectomy, histopathologic and chemical changes around the retina and postoperative complications including retinal injury, visual field loss, and retinal nerve fiber damage can occur[1-5].
Unrecognized glaucoma may result in irreversible blindness. As the average life expectancy continues to extend, the prevalence of glaucoma has increased. Some cross-sectional epidemiologic studies have shown that prevalence rates range from 0.5% to 7.0% in subjects who are over 40y of age[6]. The diagnosis of glaucoma is based on intraocular pressure(IOP), the presence of optic disc damage, visual field examination, and the thickness of the retinal nerve fiber layer(RNFL) on optical coherence tomography(OCT). Additionally, in areas with a high prevalence of normal-tension glaucoma, homodynamic values are also considered to be important factors for diagnosis[3,7-8].
Therefore we hypothesize that vitrectomy and adjunctive intraoperative procedures can result in changes in the factors used for the diagnosis of glaucoma as well as detection of disease progression. The aim of this study is to investigate the effects of vitrectomy and adjunctive intraoperative procedures in patients with various retinal diseases on retinal vessel diameter, RNFL thickness and the optic disc, and determine whether any of these ocular factors have changed, and if so how these changes impact evaluation of that patient.
SUBJECTS AND METHODS
We conducted a retrospective review of the medical records of 40 consecutive patients who had undergone 23-gauge pars plana vitrectomy at Kosin University Gospel Hospital, Busan, Korea. Informed consent was obtained from all patients. The study was followed the principles of the Declaration of Helsinki(2008). We included 40 eyes in 40 patients who underwent pars plana vitrectomy(PPV) of one eye by a single surgeon(Lee SJ) using a similar surgical technique, identical instrument gauge(ACCURUS®23 Gauge Combined Procedure Pak, Alcon, Fort Worth, TX, USA), and the same surgical machinery(ACCURUS®Surgical System, Alcon, Fort Worth, TX, USA). The fellow non-vitrectomized eyes of the 40 selected patients served as the control group, and did not undergo any other procedures. Patients were excluded based on the following criteria:1) an inadequate follow-up period of ≤6mo;2) history of previous intraocular surgery;3) history of intraocular surgery during follow-up period;4) history of prior panretinal photocoagulation;5) history of ocular disease that affects the morphology of the optic disc including glaucoma;6) high myopia lower than -6 diopters or hyperopia higher than +3 diopters;7) presence of peripapillary atrophy.
Standardized examinations were performed of both eyes by a trained ophthalmologist just before vitrectomy and at 3mo and 6mo after surgery. IOP was measured using Goldmann applanation tonometry(Haag-Streit, Koniz, Switzerland) before pupil dilation. The vertical cup-to-disc ratio was determined using 30-degree stereoscopic photographs. Measurement of the RNFL thickness was performed using a Stratus OCT(Carl Zeiss Meditec, Dublin, CA, USA). RNFL thickness was measured using RNFL thickness serial analysis consisting of 512 scans centered on the disc. Peripapillary RNFL thickness parameters calculated with a 3.4 mm diameter circle using the RNFL thickness serial analysis protocol included the average RNFL thickness, superior and inferior maximum thicknesses, and superior and inferior average thicknesses.
To measure the retinal vessel caliber, digital retinal photographs centered on each optic disc were obtained through dilated pupils using standardized settings on a Kowa nonmyd 7 fundus camera(Kowa Company, Ltd. Japan). Two retinal images were obtained:one centered on the optic disc and the other centered on the fovea[Early Treatment for Diabetic Retinopathy Study(ETDRS) standard fields 1 and 2]. Methods used to measure retinal arteriolar and venular calibers from digital photographs of the fundus using computer-assisted software(lVAN, University of Wisconsin, Madison, USA) according to a standardized protocol have been described in detail elsewhere. A trained grader blinded to participant characteristics retrieved the optic disc-centered images of the right and left eyes and identified each vessel as either an arteriole or venule using the original color photographs for reference. All arterioles and venules within a specified area [0.5-1 disc diameter surrounding the optic disc(zone B)] were measured in micrometers and combined into summary measurements [referred to as the central retinal arteriolar equivalent(CRAE) and the central retinal venular equivalent(CRVE)] sing modified Parr and Hubbard formulas as previously described. For comparing changes in vessel caliber, differences were calculated as percentages of postoperative values when preoperative baseline values were set at 100 percent in both eyes. This method was employed to compensate for interpersonal differences in retinal vessel measurements due to ocular magnification and to better compare the changes in these values.
Statistical AnalysisStatistical analyses were conducted using SPSS Software 18.0(SPSS;Chicago;IL, USA). Demographic characteristics and differences in study variables between vitrectomized eyes and fellow non-vitrectomized eyes were compared usingt-tests. In the subgroup analyses, ANOVA was used for comparisons.P<0.05 were regarded as statistically significant.
RESULTS
A total of 14 male and 26 female patients with a mean age of 58.83±13.18y were included in this study. Pre-operative indications for pars plana vitrectomy included complications of diabetic retinopathy (10 eyes), retinal detachment (9 eyes), macular hole (7 eyes), macular pucker (5 eyes), and vitreomacular traction syndrome (3 eyes). The adjunctive intraoperative procedures were depended on the disease and condition of eye including induction of posterior vitreous detachment (PVD) in 36 eyes (90%), fluid-air exchange in
Table 1Clinical characteristics of the study group
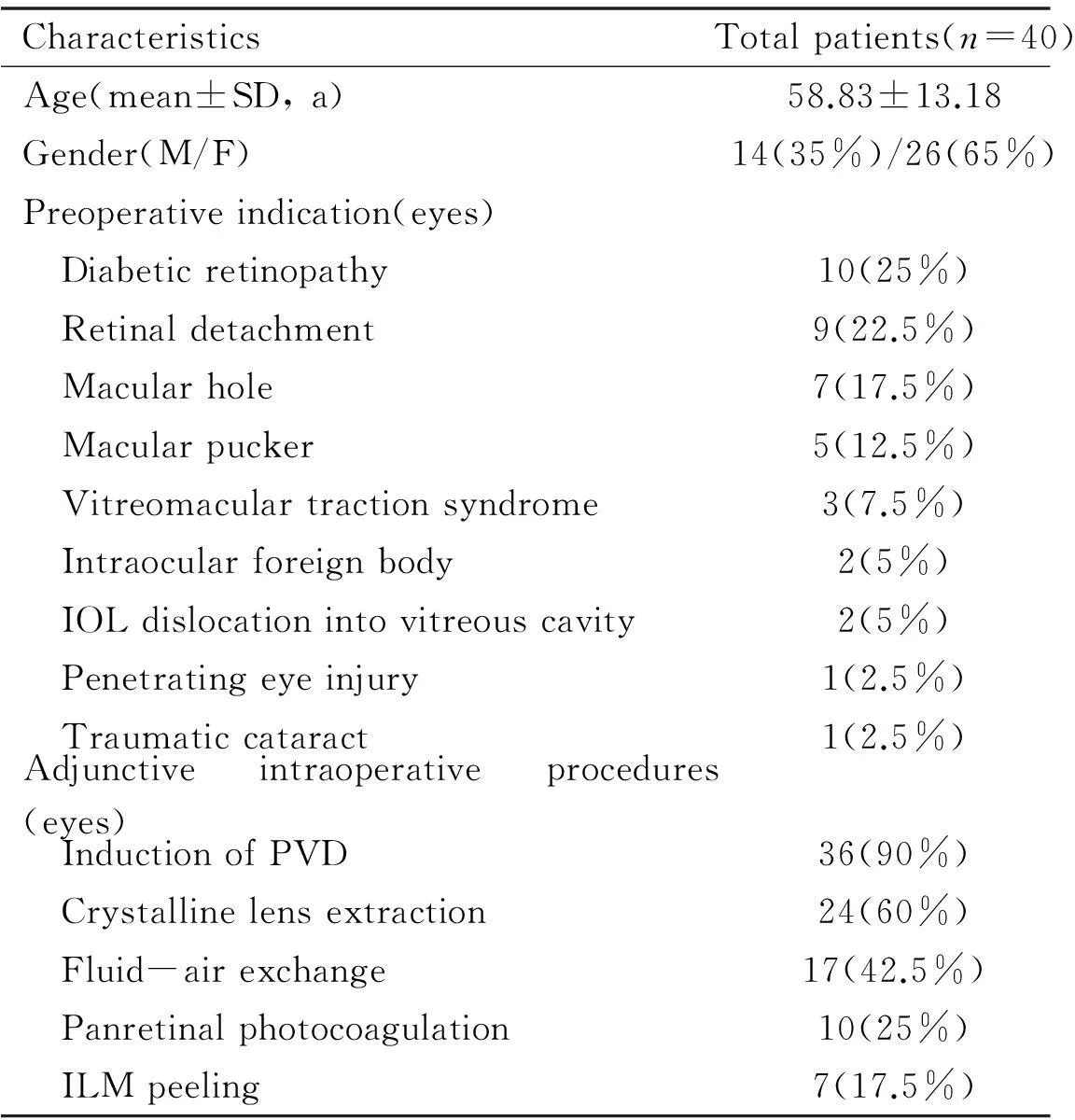
CharacteristicsTotalpatients(n=40)Age(mean±SD,a)58.83±13.18Gender(M/F)14(35%)/26(65%)Preoperativeindication(eyes) Diabeticretinopathy10(25%) Retinaldetachment9(22.5%) Macularhole7(17.5%) Macularpucker5(12.5%) Vitreomaculartractionsyndrome3(7.5%) Intraocularforeignbody2(5%) IOLdislocationintovitreouscavity2(5%) Penetratingeyeinjury1(2.5%) Traumaticcataract1(2.5%)Adjunctiveintraoperativeprocedures(eyes) InductionofPVD36(90%) Crystallinelensextraction24(60%) Fluid-airexchange17(42.5%) Panretinalphotocoagulation10(25%) ILMpeeling7(17.5%)
PVD:Posterior vitreous detachment;SD:Standard deviation;ILM:Internal limiting membrane.
Table 2Peripapillary retinal nerve fiber layer thickness measured using OCT

ParameterOperativeeyesFelloweyesSavg(mean±SD) Baseline133.6±37.2128.4±38.2 3mo126.5±29.0122.5±28.2 6mo127.1±33.5127.1±34.4Iavg(mean±SD) Baseline134.3±29.3130.3±33.9 3mo132.4±37.5131.9±29.4 6mo132.9±38.9132.6±30.5Smax(mean±SD) Baseline167.9±32.3157.1±34.4 3mo164.3±26.7153.8±27.5 6mo158.1±29.5158.6±30.2Imax(mean±SD) Baseline175.1±25.4164.2±27.9 3mo176.3±28.6171.7±23.9 6mo170.3±33.7171.7±27.7
Savg:Superior average peripapillary retinal nerve fiber thickness;Iavg:Inferior average peripapillary retinal nerve fiber thickness;Smax:Superior maximum peripapillary retinal nerve fiber thickness;Imax:Inferior maximum peripapillary retinal nerve fiber thickness;SD:Standard deviation;OCT:Optical coherence tomography. There were no significant differences in parameters produced by OCT in operative eyes and fellow eyes at any of the time points examined.
17 eyes(42.5%), lens extraction in 24 eyes(60%), panretinal photocoagulation in 10 eyes(25%) and internal limiting membrane peeling in 7 eyes(17.5%)(Table 1).
The mean baseline IOP was 15.5±3.1mm Hg, and postoperative values were 15.9±2.6 and 15.8±2.6 mm Hg in operative eyes 3mo and 6mo after surgery, respectively. There were no significant differences in IOP at any of the time points examined in affected eye compared with baseline(P=0.498 and 0.569 at 3mo and 6mo, respectively) and compared with fellow eye(P=0.110, 0.384 and 0.329 at baseline, 3mo and 6mo, respectively)(Figure 1).
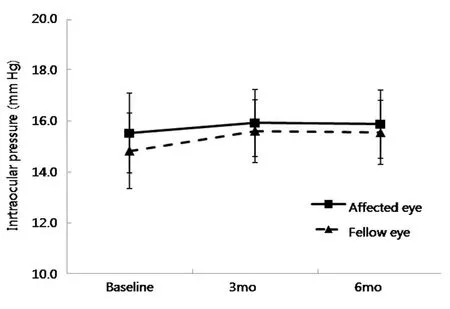
Figure 1The effect of 23-gauge pars plana vitrectomy on intraocular pressure in operative eyes versus changes in fellow eyes. There is no significant difference between the groups at any of the time points examined.
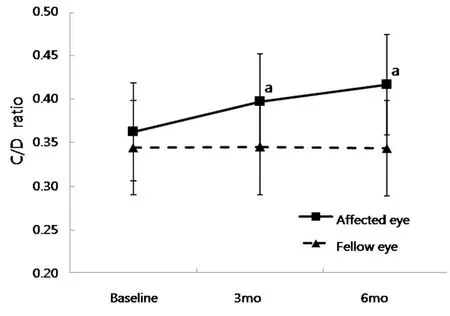
Figure 2The effect of 23-gauge pars plana vitrectomy on vertical cup-to-disc ratio in operative eyes versus changes in fellow eyes. There were statistically significant differences at both 3mo and 6mo postoperatively(P=0.038 and 0.005, respectively).aP<0.05.
The cup-to-disc ratio in eyes that underwent vitrectomy was 0.36±0.11 at baseline, and was increased to 0.40±0.11 and 0.41±0.12 at 3mo and 6mo after vitrectomy. These differences were statistically significant for both postoperative periods in affected eye compared with baseline(P=0.038 and 0.005 at 3mo and 6mo, respectively) and compared with fellow eye(P=0.035 and 0.004 at 3mo and 6mo, respectively)(Figure 2).
The peripapillary RNFL thickness was measured using OCT, as listed in Table 2. None of the parameters were significantly altered by OCT in the operative or fellow eyes at any time point examined.
The mean percent change in CRAE 6mo postoperatively was -5.01±1.50. This value was significantly different in the vitrectomized eyes compared with the fellow eyes(P=0.009,Figure 3). The mean percent change in CRVE 6mo postoperatively was -5.87±1.35. This value also significantly narrowed in the operative eyes compared with the control eyes(P=0.004,Figure 4). However, the mean percent changes in central retinal vessel diameter(CRAE and CRVE) 3mo after vitrectomy were not statistically different between the two eyes(P=0.314 and 0.134 in CRAE and CRVE, respectively).

Figure 3The effect of 23-gauge pars plana vitrectomy on the percent change in the mean central retinal arteriolar diameter in operative eyes versus changes in fellow eyes. There were statistically significant differences postoperatively in the vitrectomized eyes compared with the fellow eyes(P=0.009),aP<0.05.

Figure 4The effect of 23-gauge pars plana vitrectomy on the percent change in mean central retinal venular diameter in operative eyes versus changes in fellow eyes. There were statistically significant differences postoperatively in the vitrectomized eyes compared with the fellow eyes(P=0.004),aP<0.05.
In the subgroup analysis that was conducted according to adjunctive intraoperative procedures including fluid-air exchange and lens extraction, there were no statistically significant differences(P=0.194 and 0.579 in fluid-air exchange group and lens extraction group, respectively). In another subgroup analysis, the number of subgroup cases is too small to obtain statistical result.
DISCUSSION
Careful observation of changes in the optic nerve head(ONH) and peripapillary RNFL is of great importance in the diagnosis and monitoring of glaucoma. The association between central retinal vessel diameter and open angle glaucoma(OAG), especially in normal-tension glaucoma, have been reported by several previous studies[7-9]. It is unclear, however, whether vitreoretinal procedures increase the risk of OAG or ocular hypertension[10-12]. It was previously suggested that there is an increased risk of OAG after vitrectomy[10]. On the other hand, it was also reported that vitrectomy does not appear to increase IOP[11], and it is concluded in recent study that after long-term follow-up, there is no increased incidence of late onset OAG or ocular hypertension[12]. However, the parameters directly related to the diagnosis and monitoring of the progression of glaucoma may have been altered by pars plana vitrectomy[11,13-16].
Evaluating the ONH is an essential step in the diagnosis of glaucoma. Changes in cup-to-disc ratio after vitrectomy have been well established. One study reported a slightly increased cup-to-disc ratio that was not significantly different from baseline 3mo after surgery[16]. Another study found a statistically significant decrease in the cup-to-disc area ratio at 1, 3, and 6mo after vitrectomy using a Heidelberg retina tomograph[15]. In our study, the postoperative cup-to-disc ratio was significantly increased at 3mo and 6mo post-operatively on stereoscopic photography, which differed from previous results. This was possibly due to different methods of measurement and surgical technique. We utilized stereoscopic photographs of the optic disc in the present study, which may have more reliable reproducibility than single photography. Additionally, unlike other studies, we used the same vitreoretinal surgical instrument for all patients, and all operations were performed by a single surgeon using a unitary surgical style for 23-gauge pars plana vitrectomy on a single vitreoretinal surgical machine. Depending on the characteristics of the instrument used including the gauge, aspiration power, and cutting rates, the flow dynamics can differ, thereby altering the surgical outcome. Therefore, our data representing surgically induced changes in the optic disc is likely more consistent and reliable.
Another possible reason for these discrepant results is the different operative procedures performed in vitreoretinal practices. Induction of posterior vitreous detachment during surgery has been reported to bring about mechanical injury to the posterior fundus[3,17]. In monkeys, surgical induction of posterior vitreous detachment has also been shown to cause substantial damage to the optic disc[17]. Additionally, the shearing of peripapillary axons during vitrectomy can cause visual field loss[4-5]. In this study, 90% of patients underwent posterior vitreous detachment during vitrectomy, though no significant differences were observed. Additionally, on the subgroup analysis conducted according to the operative procedure performed, no significant differences were observed.
It was reported that routine kinetic perimetry-detectable visual field defects could be indicative of 12-63% loss of optic nerve fibers and a 10% or greater change in peripapillary RNFL thickness, which are thought to be reliable indicators of glaucoma[18]. Previous studies have shown that changes in peripapillary RNFL thickness measured using OCT after vitrectomy are variable depending on the region and postoperative period. It was suggested that temporal RNFL thickness was increased in eyes after removal of the epiretinal membrane 3mo after vitrectomy, and Kim and colleagues reported that the mean postoperative RNFL thickness was decreased in the superior quadrant[14,16]. Our data on changes in RNFL thickness 3mo and 6mo after vitrectomy show no statistically significant differences when compared with fellow eyes and preoperative data. The fluctuation in RNFL thickness indicates damage to the inner surface of the retina that occurred during the operation or the postoperative period. The mechanism of injury is either mechanical or vascular. The closer the manipulation is to the retina and/or the more variation in blood flow in the central retinal vessels brings about higher risk of inner retinal injury.
The prevalence of primary open angle glaucoma(POAG) shows broad regional and racial variations. In populations with a high prevalence of POAG with normal IOP, vascular mechanisms are suggested to play a major role in the disease process. Previous reports produced evidence regarding the relationship between POAG and retinal vessel diameter[7-9]. Vitrectomy can also alter ocular hemodynamics. In rabbits, removal of the vitreous has resulted in increased oxygen tension within the vitreous cavity, and can last for weeks[13]. In humans, who have previously undergone vitrectomy, increased oxygen tension levels and improved blood flow have been recorded compared with patients with vitreousinsitu[1,19-20]. Park and colleagues have proposed that in patients with diffuse diabetic macular edema, vitrectomy improves retinal oxygenation and reduces the accumulation of vasoactive cytokines, which are positively correlated with vasodilation and vascular permeability, and induces vasoconstriction[2]. In this study, changes in central retinal vessel diameter are significantly narrower compared with fellow eyes 6mo after vitrectomy. Although an understanding of the hemodynamics of the eye is not possible with information about central retinal vessel diameter alone, the elevated oxygen tension of the inner retinal region may be suggested as a reason for central vessel narrowing.
This study has some limitations. First, because of retrospective observational design, this study cannot control the variations such as systemic hypertension, diabetes, age and glaucoma family history that may have concerned to the vessel caliber and optic nerve cup. So, to overcome this problem, we set the baseline measured value as 100 percent in each individual eye and use percent change compared to baseline instead of the postoperative measured absolute value in vessel caliber, and we also compared the affect eye with the fellow eye in vessel caliber and cup-to-disc ratio. Second, because there are many different operative conditions even in same disease, adjunctive intraoperative procedures of pars plana vitrectomy are not unified in detail. We cannot investigate the effect of each separate procedure which has been done adjunctive to vitrectomy according to vitreoretinal disease intraoperatively by separate group or intergroup analysis. In this study, we can only identify the effects of whole vitreoretinal surgical procedures including 23G pars plana vitrectomy and adjunctive intraoperative procedure.
In this study, 23-gauge pars plana vitrectomy and adjunctive intraoperative procedure induced an increased cup-to-disc ratio and narrowed central retinal vessels, implying that mechanical and chemical alterations of the optic disc and inner retina occurred after surgical intervention. In particular, changes in the cup-to-disc ratio without variation in the peripapillary RNFL thickness could indicate damage to the connective tissue around the optic disc, or of the optic disc itself.
In conclusion, for the exact diagnosis and monitoring of POAG, physicians should consider the effects of vitreoretinal surgical procedures on cup-to-disc ratio and central retinal vessel diameter.
REFERENCES
1 Sullu Y, Hamidova R, Beden U, Yakupov K, Canbaz S, Danaci M. Effects of pars plana vitrectomy on retrobulbar haemodynamics in diabetic retinopathy.ClinExperimentOphthalmol2005;33(3):246-251
2 Park JH, Woo SJ, Ha YJ, Yu HG. Effect of vitrectomy on macular microcirculation in patients with diffuse diabetic macular edema.GraefesArchClinExpOphthalmol2009;247(8):1009-1017
3 Mayer WJ, Vogel M, Neubauer A, Kernt M, Kampik A, Wolf A, Haritoglou C. Pars plana vitrectomy and internal limiting membrane peeling in epimacular membranes:correlation of function and morphology across the macula.Ophthalmologica2013;230(1):9-17
4 Jain N, McCuen BW 2nd, Mruthyunjaya P. Unanticipated vision loss after pars plana vitrectomy.SurvOphthalmol2012,57(2):91-104
5 Uchida A, Shinoda K, Matsumoto CS, Kawai M, Kawai S, Ohde H, Ozawa Y, Ishida S, Inoue M, Mizota A, Tsubota K. Acute Visual Field Defect following Vitrectomy Determined to Originate from Optic Nerve by Electrophysiological Tests.CaseRepOphthalmol2012;3(3):396-405
6 Rudnicka AR, Mt-Isa S, Owen CG, Cook DG, Ashby D. Variations in primary open-angle glaucoma prevalence by age, gender, and race:a Bayesian meta-analysis.InvestOphthalmolVisSci2006;47(10):4254-4261
7 Lee JY, Yoo C, Park JH, Kim YY. Retinal vessel diameter in young patients with open-angle glaucoma:comparison between high-tension and normal-tension glaucoma.ActaOphthalmol2012;90(7):e570-e571
8 Gao J, Liang Y, Wang F, Shen R, Wong T, Peng Y, Friedman DS, Wang N. Retinal vessels change in primary angle-closure glaucoma:the Handan Eye Study.SciRep2015;5:9585
9 Chang M, Yoo C, Kim SW, Kim YY. Retinal vessel diameter, retinal nerve fiber layer thickness, and intraocular pressure in korean patients with normal-tension glaucoma.AmJOphthalmol2011;151(1):100-105.e1
10 Chang S. LXII Edward Jackson lecture:open angle glaucoma after vitrectomy.AmJOphthalmol2006;141(6):1033-1043
11 Lalezary M, Kim SJ, Jiramongkolchai K, Recchia FM, Agarwal A, Sternberg P Jr. Long-term trends in intraocular pressure after parsplana vitrectomy.Retina2011;31(4):679-685
12 Yu AL, Brummeisl W, Schaumberger M, Kampik A, Welge-Lussen U. Vitrectomy does not increase the risk of open-angle glaucoma or ocular hypertension--a 5-year follow-up.GraefesArchClinExpOphthalmol2010;248(10):1407-1414
13 Barbazetto IA, Liang J, Chang S, Zheng L, Spector A, Dillon JP. Oxygen tension in the rabbit lens and vitreous before and after vitrectomy.ExpEyeRes2004;78(5):917-924
14 Kim KY, Yu SY, Kim MS, Kim ES, Kwak HW. Changes of parafoveal retinal nerve fiber layer thickness analyzed by spectral-domain optical coherence tomography after pars plana vitrectomy.Retina2013;33(4):776-784
15 Ohashi H, Kasuga Y, Hata N, Manabe S, Takashima Y, Lee S, Yamakawa R. Morphological changes in the optic disc after vitrectomy and fluid-air exchange.GraefesArchClinExpOphthalmol2004;242(6):484-488
16 Reddy RK, Lalezary M, Kim SJ, Kammer JA, Kuchtey RW, Cherney EF, Recchia FM, Joos KM, Agarwal A, Law JC. Prospective Retinal and Optic Nerve Vitrectomy Evaluation(PROVE) study:findings at 3mo.ClinOphthalmol2013;7:1761-1769
17 Russell SR, Hageman GS. Optic disc, foveal, and extrafoveal damage due to surgical separation of the vitreous.ArchOphthalmol2001;119(11):1653-1658
18 Quigley HA, Sommer A. How to use nerve fiber layer examination in the management of glaucoma.TransAmOphthalmolSoc1987;85:254-272
19 Lim LS, Tan L, Perera S. Retinal vessel oxygen saturation increases after vitrectomy.InvestOphthalmolVisSci2014;55(6):3851-3856
20 Sín M, Sínová I, Chrapek O, Pracharová Z, Karhanová M, Langová K, Rehák J. The effect of pars plan vitrectomy on oxygen saturation in retinal vessels--a pilot study.ActaOphthalmol2014;92(4):328-331
摘要
关键词:视网膜血管直径;视网膜神经纤维厚度;视盘;玻璃体切割术
DOI:10.3980/j.issn.1672-5123.2016.5.03
通讯作者:Sang Joon Lee. hhiatus@gmail.com
目的:调查接受睫状体平坦部玻璃体切割术及术中辅助治疗患者的视网膜血管直径,视网膜神经纤维层厚度和视盘改变。
方法:共40例(40眼)接受单侧睫状体平坦部玻璃体切割术及术中辅助治疗患者纳入研究,分别于术前、术后3mo及6mo行视网膜照相检测视网膜中央动脉和静脉的直径,应用修正Parr-Hubbard公式计算视网膜中央动脉当量和视网膜中央静脉当量。运用Stratus OCT检测视神经纤维层厚度。立体视盘摄影检测视盘的垂直杯盘比。
结果:术前患者的双眼视网膜血管直径与神经纤维层厚度及视盘检查无统计学差异。垂直杯盘比在3mo和6mo较术前明显增加(P<0.01,P<0.01),且手术眼与对侧眼显著不同(P<0.01,P<0.01)。术后6mo术眼视网膜中央动脉当量与视网膜中央静脉当量的改变明显大于对侧眼(P<0.01,P<0.01)。视神经纤维层厚度无显著变化。
结论:玻璃体切割术及术中辅助治疗在术后6mo会引起视盘的垂直杯盘比及视网膜血管直径的改变,而视网膜神经纤维层厚度变化不明显。
引用:Lee SU, Kim SJ, Lee SJ. 23G玻璃体视网膜手术后视网膜血管直径与神经纤维层厚度及视盘的变化.国际眼科杂志2016;16(5):801-806
·Original article·
