A case of giant prostatic hyperplasia
2016-04-27LukeWngPulDvisKevinMcMillnb
Luke Wng*,Pul DvisKevin McMillnb
aDepartment of Urology,Eastern Health,Nelson St,Box Hill,Victoria,Australia
bMonash University,Eastern Health Clinical School,Arnold St,Box Hill,Victoria,Australia
CASE REPORT
A case of giant prostatic hyperplasia
Luke Wanga,*,Paul Davisa,Kevin McMillana,b
aDepartment of Urology,Eastern Health,Nelson St,Box Hill,Victoria,Australia
bMonash University,Eastern Health Clinical School,Arnold St,Box Hill,Victoria,Australia
Prostate;
Prostatic hyperplasia;
Urology;
Haematuria;
Indwelling catheters
Benign prostatic hyperplasia(BPH)is one of the most common conditions experienced by aging males and a frequent cause of bladder outlet obstruction and macroscopic haematuria.Giant prostatic hyperplasia(GPH)is an extremely rare form of prostatic hyperplasia. We present a case of a patient with GPH of 800 mL.To our knowledge,this is the fourth largest prostatic hyperplasia ever reported in the literature.
ⓒ2016 Editorial Office of Asian Journal of Urology.Production and hosting by Elsevier B.V.This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/ licenses/by-nc-nd/4.0/).
1.Introduction
Benign prostate hyperplasia(BPH)is a common condition that produces progressive lower urinary tract symptoms in aging males.Giant prostate hyperplasia(GPH)is a rare entity and defined as massive prostate hyperplasia weighing more than 500 g[1].We present a case of a 94-year-old man with conservatively managed GPH of 800 mL,which is the fourth largest recorded prostate enlargement in literature.
2.Case report
A 94-year-old male presented with 24 h of macroscopic haematuria complicated by clot retention.Clinical examination revealed a tender dull mass in the suprapubic region.Digital rectal examination revealed a very large prostate with no malignant features.In the emergency department,bladder scan revealed a residual volume of 400 mL.A 3-way urinary catheter was inserted and continuous bladder washout was commenced.Laboratory examinations revealed haemoglobin of 113 g/L,serum creatinine of 111 μmol/L and normal coagulation studies. Urine analysis showed a large amount of red blood cells.A computer tomography(CT)scan was performed to investigate the cause of macroscopic haematuria and it highlighted a grossly enlarged prostate.By obtaining the maximum organ dimensions in the anterior-posterior, lateral and longitudinal planes,the radiologist calculated the prostate volume to be at 800 mL.So large was the prostate that the tip and balloon of the indwelling catheter was seen to just reach beyond the end of the gland(Figs. 1-3).
Upon further review,the patient described longstanding lower urinary tract symptoms of slow stream,incomplete emptying and urinary frequency.Two years earlier he hadanother episode of macroscopic haematuria and the renal tract ultrasound highlighted gross prostatomegaly with a volume of 420 mL.Flexible cystoscopy confirmed the ultrasound findings of the enormous prostate.He refused surgical intervention at that time and was commenced on combination therapy,tamsulosin 400 mcg and dutasteride 500 mcg.This gentleman also had medical co-morbidities including ischaemic heart disease,chronic obstructive pulmonary disease,chronic lymphocytic leukaemia and gout.
Whilst his haematuria settled on continuous bladder irrigation,he developed bilateral lower limb swelling and Doppler ultrasound identified bilateral deep vein thrombosis(DVT).He was commenced on low-molecular weight heparin to prevent clot propagation.Unfortunately this contributed to ongoing haematuria and required packed red cell transfusions.
The treatment options for this gross prostatic enlargement were limited by his comorbidities,age and bilateral DVTs.He was not suitable for endoscopic resection due to its enormous size.Open prostatectomy was considered but the patient and his family declined due to the risks associated with major surgery and his significant comorbidities.Suprapubic catheterisation was not viable due to the fact that patient’s entire bladder was filled by intravesical prostate tissue as depicted in Fig.1.
Repeat lower leg Doppler ultrasound imaging revealed DVT resolution and anticoagulation therapy was ceased. Haematuria subsequently resolved and the patient was discharged with a long-term indwelling catheter in situ.At the time of submission,patient had no further episodes of haematuria and is coping well with the urinary catheter.

Figure 1Coronal CT image showing giant prostate occupying majority of the bladder.
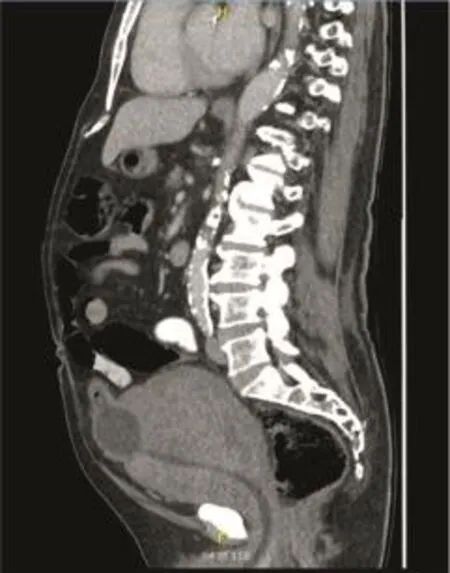
Figure 2Sagittal CT image showing tip and balloon of indwelling catheter barely above the giant prostate.

Figure 3Axial CT image showing the bladder filled by prostate tissue with the catheter traversing the prostatic tissue.
3.Discussion
BPH is a frequent cause of bladder outlet obstruction and can cause macroscopic haematuria.It is one of the most common diseases experienced by aging males and histological evidence of the disease is present in up to 60%of men at age 60[2].GPH is defined as a prostate weighing more than 500 g[1].In the current literature,there are few cases of BPH with volumes greater than 500 g,and only nine reported cases of giant prostate enlargement exceeding 700 g[1,3-10].Our case represents the fourth largest prostate reported in the literature.
The pathophysiology of GPH is not fully understood. Hypotheses suggest a combination of disruption in normal stromal-epithelial paracrine signalling,an imbalance between androgenic,cytokine and peptide growth signalling, a reduction in apoptosis and a proliferation in stromal and epithelial cells which result in significant prostate enlargement[1].Specifically,mutations of protooncogenes such as Ras and c-erbB2,as well as the downregulation of the p53 suppressor gene,can lead to the abnormal and continuous cellular proliferation[1].
Surgical intervention is indicated in BPH when patients have acute or chronic urinary retention,recurrent gross haematuria,urinary tract infections,renal insufficiency, bladder stones or severe lower urinary tract symptoms refractory to medical treatment[2].Transurethral resection of prostate(TURP),transurethral incision of the prostate(TUIP),and laser vaporisation or enucleation techniques are surgical options for small and medium-sized prostates [2].Open prostatectomy is utilised for large prostates not amendable to sequential endoscopic procedures,and those with coexistent pathology like bladder stones[2].This gentleman would have best been treated by open prostatectomy,however his age and comorbidities precluded this approach.
Conflicts of interest
The authors declare no conflict of interest.
[1]Maliakal J,Mousa EE,Menon V.Giant prostatic hyperplasia: fourth largest prostate reported in medical literature.Sultan Qaboos Univ Med J 2014;14:e253-6.
[2]Thorpe A,Neal D.Benign prostatic hyperplasia.Lancet 2003; 361:1359-67.
[3]Gilbert J.One-stage suprapubic prostatectomy for a gland weighing 713 grams(one and one-half pounds).Urol Cutan Rev 1939:309-10.
[4]Lantzius-Beninga F.A prostate of world record size.Z Urol Nephrol 1966;59:77-9[in German].
[5]Medina Pe´rez M,Valero Puerta J,Valpuesta Ferna´ndez I, Sa´nchez Gonza´lez M.Giant hypertrophy of the prostate:2,410 grams of weight and 24 cm in diameter.Arch Esp Urol 1997;50: 795-7[in Spanish].
[6]Nelson OA.Largest recorded prostate.Urol Cutan Rev 1940; 44:454-5.
[7]Ockerblad NF.Giant prostate;the largest recorded.J Urol 1946;56:81.
[8]Tolley DA,English PJ,Grigor KM.Massive benign prostatic hyperplasia.J R Soc Med 1987;80:777-8.
[9]U¨c¸er O,Baser O¨,Gu¨mu¨s‚B.Giant prostatic hyperplasia:case report and literature review.Dicle Med J 2011;38:489-91.
[10]Wadstein T.The largest surgically removed hypertrophied prostate.JAMA 1938;110:509.
Received 28 September 2015;received in revised form 12 October 2015;accepted 16 October 2015
Available online 3 November 2015
*Corresponding author.
E-mail address:drlukewang@gmail.com(L.Wang).
Peer review under responsibility of Shanghai Medical Association and SMMU.
http://dx.doi.org/10.1016/j.ajur.2015.10.004
2214-3882/ⓒ2016 Editorial Office of Asian Journal of Urology.Production and hosting by Elsevier B.V.This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
杂志排行
Asian Journal of Urology的其它文章
- Unusual case of nephrocutaneous fistula-Our experience
- Tumour lysis syndrome:A rare acute presentation of locally advanced testicular cancer-Case report and review of literature
- Who needs further evaluations to diagnose upper urinary tract urothelial cancers among patients with abnormal findings by enhanced CT?
- Can intravesical prostatic protrusion predict bladder outlet obstruction even in men with good flow?
- Zoledronic acid combined with androgendeprivation therapy may prolong time to castration-resistant prostate cancer in hormone-naïve metastatic prostate cancer patients-A propensity scoring approach
- Prostate cancer volume associates with preoperative plasma levels of testosterone that independently predicts high grade tumours which show low densities(quotient testosterone/tumour volume)
