Tumour lysis syndrome:A rare acute presentation of locally advanced testicular cancer-Case report and review of literature
2016-04-27MarcusChowAriantoYuwonoRonnyTan
Marcus Chow*,Arianto Yuwono,Ronny Tan
Department of Urology,Tan Tock Seng Hospital,Singapore
CASE REPORT
Tumour lysis syndrome:A rare acute presentation of locally advanced testicular cancer-Case report and review of literature
Marcus Chow*,Arianto Yuwono,Ronny Tan
Department of Urology,Tan Tock Seng Hospital,Singapore
Tumour lysis
Tumour lysis syndrome(TLS)is a potentially fatal complication of malignancy or its treatment.This uncommon syndrome comprises laboratory findings of hyperuricaemia,hypocalcaemia,hyperkalaemia and hyperphosphataemia.A literature search revealed a total of eight patients,with testicular cancer,who had TLS.All these patients had metastatic disease. We present a unique case of a 47-year-old gentleman we saw in clinic,who presented with a rapidly growing right groin mass and acute breathlessness,and discuss the diagnosis and management of TLS.TLS is extremely rare in testicular cancer but necessitates the awareness of urologists.TLS can occur spontaneously in testicular malignancy.Cell lysis in a rapidly proliferating germ cell tumour is a possible mechanism.The prompt identification and institution of management for TLS is crucial to improve clinical outcomes.
ⓒ2016 Editorial Office of Asian Journal of Urology.Production and hosting by Elsevier B.V.This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/ licenses/by-nc-nd/4.0/).
1.Introduction
Tumour lysis syndrome(TLS)is an oncological emergency, which is characterized by the derangement of cellular metabolism that can lead to acute renal impairment, metabolic acidosis,cardiac rhythm disturbances,seizures and death[1].Massive cell lysis results in the release of large amounts of uric acid,potassium and phosphate into the systemic circulation.Hyperkalaemia,if untreated,may cause muscle weakness or paralysis and more significantly, cardiac arrhythmias and ultimately death[1].Hyperphosphataemia is often associated with hypocalcaemia due to the precipitation of phosphate with the calcium in tissues.The resultant secondary hypocalcaemia may result inneuromuscular symptoms such as tetany,laryngospasm and cardiac arrhythmias.Both hyperuricaemia and hyperphosphataemia potentiate the risk of acute kidney injury by way of uric acid precipitation and calcium phosphate deposition in the renal tubules,further aggravating the electrolyte imbalance[2].Additionally,the products of cell lysis trigger the release of cytokines,resulting in a systemic inflammatory response syndrome and frequently multiorgan failure[1].
TLS most commonly occurs after the initiation of cytotoxic therapy in patients with aggressive lymphoma or leukaemia.However,it may also occur spontaneously with other types of tumours that have a high proliferative rate, tumour burden or sensitivity to cytotoxic agents.In the setting of testicular cancer,a literature search only revealed eight incidences of TLS in testicular tumours,of which seven were metastatic and one had nodal involvement[3,4].TLS occurred spontaneously in three patients, all of who had metastatic testicular seminomas[3].The presence of metastatic disease would be compatible with an increased tumour burden which consequentially increases the risk of TLS occurring,either spontaneously or after the initiation of chemotherapy.
We present the case of a 47-year-old gentleman who was referred for a right groin swelling.
2.Case report
The patient was referred for progressive right groin swelling of 1-year duration,which had recently rapidly increased in size over the past 2 weeks.He reported a history of an undescended right testis,for which he underwent no previous surgical intervention.He reported good appetite and denied any weight loss.Physical examination revealed a 15 cm×10 cm firm right groin lump,not extending into the scrotum.The right testis was not palpable in his scrotum.A CT abdomen/pelvis scan done prior to the clinic consultation revealed a 15 cm×11 cm×16 cm right groin solid mass,which was partly cystic with septations and calcif ication,suggestive of gonadal malignancy.There was no lymphadenopathy,metastasis or ascites in the abdomen. The right testis was not seen within the scrotum(Fig.1). During the consultation,he was noted to be dyspnoeic and tachypnoeic but able to speak in full sentences.Upon further probing,he reported decreased effort tolerance, breathlessness and bilateral lower limb swelling for the past 2 days.He was admitted for an urgent CT pulmonary angiogram(CTPA).The CTPA performed excluded pulmonary embolism and lung metastases.
After admission,he was noted to be more tachypnoeic and struggling to speak in full sentences on the ward.An arterial blood gas(ABG)performed on 4 L/min of oxygen revealed severe metabolic acidosis with a pH of 7.08 and a lactate>10.9 mmol/L.He was promptly transferred to the intensive care unit(ICU)and intubated to provide mechanical ventilatory support.TLS was provisionally diagnosed and subsequently confirmed on laboratory findings. His blood results revealed hyperuricaemia,hyperphosphataemia,hyperkalaemia and an elevated creatinine and urea.Testicular tumour markers revealed a raised lactate dehydrogenase(LDH)>3800 U/L,and β subunit of human chorionic gonadotropin(β-hCG)37 IU/L,with a normal α-fetoprotein(AFP)3 μg/L.Post-intubation,he had a decreased level of consciousness,with a Glasgow coma scale score of 3 out of 15 despite receiving no intravenous sedation.
His electrolyte abnormalities were addressed systematically.For the hyperkalaemia,he received intravenous insulin,calcium gluconate and calcium resonium.For the hyperuricaemia,oral allopurinol via a nasogastric tube and intravenous rasburicase were administered.In view of the refractory hyperkalaemia and worsening metabolic acidosis despite intravenous sodium bicarbonate and multiple fluid challenges,a vascular catheter was inserted in his right internal jugular vein;he was started on continuous renal replacement therapy(CRRT).His systolic blood pressure dropped to 40-60 mmHg during CRRT, from approximately 110 mmHg.It was refractory to intravenous 5%albumin boluses as well as intravenous noradrenaline.CRRT was discontinued after 60 min as the persistently low blood pressure resulted in the formation blood clots in the vascular catheter.Additional inotropic support in the form of intravenous adrenaline was started. Despite the best treatment,the patient had a cardiac arrest and died.
3.Discussion
3.1.Incidence
This case illustrates a rare presentation of a testicular malignancy.To our knowledge,this is the first case of a non-metatstatic testicular malignancy,with no nodal involvement to present with spontaneous TLS.TLS most
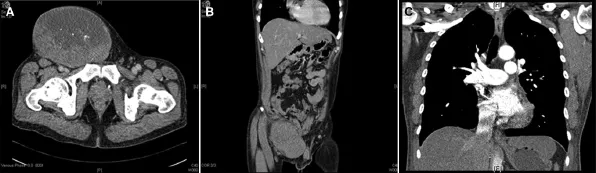
Figure 1(A)(B)CT abdomen/pelvis revealed a 15 cm×11 cm×16 cm right groin mass.There was no lymphadenopathy or metastasis present.(C)CT pulmonary angiogram revealed no pulmonary embolism or lung metastasis.
commonly occurs after initiation of cytotoxic therapy.In the testicular malignancy setting,spontaneous occurrence of TLS is even rarer.In particular,this patient’s CT scans showed no regional lymphadenopathy or distant metastasis, unlike previous reported cases where patients with TLS had metastatic testicular malignancy.Of the eight reported cases of TLS resulting from testicular malignancy,there were four patients who had seminomas[5-8].All the patients with seminomas had evidence of metastatic disease, either nodal or distant organ metastases.The other tumours reported included testicular choriocarcinoma[5], germ cell tumour and non seminomatous tumour[7],all of which were metastatic.Spontaneous TLS was reported in three of the cases,of which all were seminomas with metastatic disease[6,8].Interestingly,a retrospective study done by Kattan et al.[9]failed to show the presence of TLS in 46 cases of germ cell tumours receiving aggressive cisplatin based chemotherapy.Despite not having any evidence of metastasis,factors contributing to our patient’s occurrence of TLS would be the size of his tumour and recent rapid rate of growth,favouring a highly proliferative malignancy.
3.2.Diagnosis
We arrived at the provisional diagnosis of TLS after taking into account his unique presentation of acute breathlessness,rapidly growing right groin mass,negative findings from CTPA and ABG showing severe metabolic acidosis. Despite the prompt recognition of TLS from the time he was found to be in severe metabolic acidosis and institution of relevant management,he deteriorated and died,less than 24 h after his clinic consultation.The circumstances of his demise necessitated that his case had to be referred to the coroner’s office.After reviewing the clinical case and evidence,the coroner’s office established that the cause of his death was“Locally Advanced Testicular Malignancy”.A post-mortem was not performed.The history of an undescended right testis,radiological findings of a solid,partly cystic groin mass with septation and calcifications in conjunction with a raised β-hCG point strongly towards a testicular germ-cell tumour.In this case,the most probable diagnosis was a rapidly proliferating testicular germ cell tumour.Testicular lymphoma remains a distant possibility, however it is extremely unlikely as there was no evidence of lymphadenopathy in the chest,abdomen or pelvis.The intravenous contrast from the CT abdomen,pelvis and pulmonary angiogram may have further contributed to renal insult hence aggravating the TLS.Unfortunately,not all of the published case reports described the process in which the diagnosis of TLS was made in these patients with testicular malignancy.A common presentation was progressive dyspnoea that led on to further investigations being performed.Most of them had documented evidence of elevated creatinine,LDH and uric acid.
3.3.Management
The occurrence of TLS is multifactorial;attributes such as age,LDH levels,white cell count,baseline creatinine,comorbidities and cancer type and stage are risk factors[10]. The ideal treatment of TLS is prevention.Risk stratification and initiation of TLS prophylaxis is crucial.Risk stratification for TLS based on the above-mentioned risk factors was developed by Cairo et al.[10]to help indicate which patients required prophylaxis in the form of close monitoring with accurate fluid balance charting,intravenous hydration and medication such as allopurinol or rasburicase.Testicular malignancy,which belongs to the subgroup of solid tumours are classified as low risk and prophylaxis includes close monitoring and intravenous hydration with or without the administration of allopurinol.For patients receiving cytotoxic agents,those at high risk for developing TLS should be assessed for clinical signs and biochemical markers,such as LDH,serum creatinine,uric acid and electrolytes,every 4-6 h after commencement[11].The most important prophylaxis is the hyperhydration with intravenous fluids.This helps improve renal perfusion and glomerular filtration and minimizes acidosis(which promotes the precipitation of uric acid crystals)[1].Fluid administration also improves urine output which facilitates the elimination of urates and phosphates[11].The aim should be to maintain a urine output of greater than 100 mL/h[12].Secondly,hypouricaemic agents like allopurinol and rasburicase that reduce the level of uric acid are valuable in the prevention of TLS.However,it is important to note that while allopurinol prevents the formation of new uric acid by inhibiting xanthine oxidase, existing uric acid still has to be excreted.Rasburicase is a recombinant urate oxidase enzyme that metabolises uric acid to allantoin,hence reducing high levels of uric acid in addition to preventing hyperuricaemia[1].Rasburicase is indicated for patients at higher risk of developing TLS.
Despite appropriate prophylactic measures,about 3%-5% of patients receiving cytotoxic chemotherapy will develop TLS[13].In addition to accurate fluid balance charting,patients should also receive continuous cardiac monitoring together with 4-6 hourly biochemical testing of creatinine, uric acid and electrolytes.Hyperkalaemia is the most dangerous element of TLS as it may cause sudden death secondary to a cardiac arrhythmia.Hyperkalaemia may be corrected with intravenous hydration,sodium polystyrene, sabutamol and intravenous insulin and dextrose.Haemodialysis or hemofiltration to remove the excess potassium is the last resort.Hypocalcaemia may also result in lifethreatening dysarrhythmias and neuromuscular irritability. Ensuring that serumphosphate levels are corrected may help avoid hypocalcaemia.If required,symptomatic hypocalcaemia may be treated calcium supplementation at the lowest dose possible to relieve symptoms.Regardless of optimal treatment,severe acute kidney injury may still occur in some patients.Worsening acidosis,severe acute kidney injury and refractory electrolyte abnormalities are indications for renal replacement therapy[14].
Prompt recognition and timely intervention remain the most crucial elements in the successful management of patients with TLS.A case report of a patient with metastatic testicular choriocarcinoma with seminoma,who developed TLS after receiving adjuvant chemotherapy illustrated that aggressive intensive care and prompt intervention led to the prevention of a fatal outcome secondary to TLS[15].
3.4.Learning point
In the case of our patient,it was unfortunate that medical attention was sought so late in the course of his disease. Despite arriving at the diagnosis of TLS shortly after hospital admission,the prompt measures we initiated were unable prevent a fatal outcome.His outcome might have improved with earlier surgical intervention such as an orchidectomy,to reduce the tumour burden.
4.Conclusion
In conclusion,TLS is extremely rare in untreated,nonmetastatic testicular cancer but necessitates the awareness of urologists.It is important to note that TLS can occur spontaneously in malignancy;cell lysis in a rapidly proliferating germ cell tumour is a possible mechanism.The prompt identification and institution of management for TLS is crucial to improve clinical outcomes.
Conflicts of interest
The authors declare no conflict of interest.
[1]Howard SC,Jones DP,Pui CH.The tumor lysis syndrome.Engl J Med 2011;364:1844-54.
[2]Baeksgaard L,Sørensen JB.Acute tumor lysis syndrome in solid tumors-a case report and review of the literature. Cancer Chemother Pharmacol 2003;51:187-92.
[3]Mirrakhimov AE,Ali AM,Khan M,Barbaryan A.Tumor lysis syndrome in solid tumors:an up to date review of the literature.Rare Tumors 2014;6:5389.
[4]Kobatake K,Kato M,Mita K.Advanced testicular cancer associated with life-threatening tumour lysis syndrome and choriocarcinoma syndrome.Can Urol Assoc J 2015;9:62-4.
[5]Blanke CD,Hemmer MP,Witte RS.Acute tumor lysis syndrome with choriocarcinoma.South Med J 2000;93:916-9.
[6]Pentheroudakis G,O’Neill VJ,Vasey P,Kaye SB.Spontaneous acute tumour lysis syndrome in patients with metastatic germ cell tumours.Support Care Cancer 2001;9:554-7.
[7]Feres GA,Salluh JI,Ferreira CG,Soares M.Severe acute tumor lysis syndrome in patients with germ-cell tumors.Indian J Urol 2008;24:555-7.
[8]D’Alessandro V,Greco A,Clemente C,Sperandeo M,De Cata A,Di Micco C,et al.Severe spontaneous acute tumor lysis syndrome and hypoglycemia in patient with germ cell tumor.Tumori 2010;96:1040-3.
[9]Kattan J,Culine S,Tavakoli-Razavi T,Kramar A,Droz JP.Acute tumor lysis syndrome in poor-risk germ cell tumors:does it exist?Support Care Cancer 1994;2:128-31.
[10]Cairo MS,Coiffier B,Reiter A,Younes A.TLS expert panel. Recommendations for the evaluation of risk and prophylaxis of tumour lysis syndrome(TLS)in adults and children with malignant diseases:an expert TLS panel consensus.Br J Haematol 2010;149:578-86.
[11]Coiffier B,Altman A,Pui CH,Younes A,Cairo MS.Guidelines for the management of pediatric and adult tumor lysis syndrome:an evidence-based review.J Clin Oncol 2008;26: 2767-78.
[12]Pession A,Masetti R,Gaidano G,Tosi P,Rosti G,Aglietta M, et al.Risk evaluation,prophylaxis,and treatment of tumor lysis syndrome:consensus of an Italian expert panel.Adv Ther 2011;28:684-97.
[13]Sarno J.Prevention and management of tumor lysis syndrome in adults with malignancy.J Adv Pract Oncol 2013;4:101-6.
[14]Cairo MS,Bishop M.Tumour lysis syndrome:new therapeutic strategies and classification.Br J Haematol 2004;127:3-11.
[15]Kawai K,Takaoka E,Naoi M,Mori K,Minami M,Shimazui T, et al.A case of metastatic testicular cancer complicated by tumour lysis syndrome and choriocarcinoma syndrome.Jpn J Clin Oncol 2006;36:665-7.
Received 1 July 2015;received in revised form 17 September 2015;accepted 28 September 2015
Available online 24 October 2015
*Corresponding author.
E-mail address:marcus.chow@mohh.com.sg(M.Chow).
Peer review under responsibility of Shanghai Medical Association and SMMU.
http://dx.doi.org/10.1016/j.ajur.2015.09.005
2214-3882/ⓒ2016 Editorial Office of Asian Journal of Urology.Production and hosting by Elsevier B.V.This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
syndrome;
Testicular cancer;
Testicular malignancy
杂志排行
Asian Journal of Urology的其它文章
- PMEPA1 guards against TGF-β-mediated prostate cancer bone metastasis
- Relationship between urodynamic patterns and lower urinary tract symptoms in Chinese women with a non-neurogenic bladder
- Elevated preoperative neutrophil-tolymphocyte ratio may be associated with decreased overall survival in patients with metastatic clear cell renal cell carcinoma undergoing cytoreductive nephrectomy
- Prostate cancer volume associates with preoperative plasma levels of testosterone that independently predicts high grade tumours which show low densities(quotient testosterone/tumour volume)
- Zoledronic acid combined with androgendeprivation therapy may prolong time to castration-resistant prostate cancer in hormone-naïve metastatic prostate cancer patients-A propensity scoring approach
- Can intravesical prostatic protrusion predict bladder outlet obstruction even in men with good flow?
