Utilization patterns of benzodiazepines in psychiatric patients in a tertiary care teaching hospital
2016-04-10UdayVenkatMatetiPramithaPrabhakaranSanalTS
Uday Venkat Mateti, Pramitha Prabhakaran Sanal TS
1 Department of Pharmacy Practice, NGSM Institute of Pharmaceutical Sciences, Nitte University, Mangalore, Karnataka, India
2 Department of Biostatistics, K. S. Hegde Medical Academy, Nitte University, Mangalore, Karnataka, India
INTRODUCTION
Over the years, treatments for psychiatric disorders are emerging as an important public health priority and is recognized as one of the major causes of morbidity. Nowadays, a wide array of drugs are available for the treatment of psychiatric disorders. Several drug utilization studies on psychiatric drugs have been conducted and addressed certain major issues: drug use patterns, prescribing behaviour, gaps between guidelines and actual utilization and factors responsible for polypharmacy. Such studies are helpful in optimizing usage level in a given clinical setting(Jayaprakash, 2014). Benzodiazepines are an important class of drugs used in psychiatry and prescribed for various conditions such as stress and anxiety, sleeping problem,muscle tension, as an anaesthetic before surgery as well as treatment for epilepsy and alcohol withdrawal. They are also prescribed in panic disorders and catatonia. Benzodiazepines are known as “minor tranquilizers” (Sachdeva and Patel, 2010), and act on the central nervous system.They induce relaxation and calmness by its depressive action. Benzodiazepines work by increasing the efficiency of GABA (a natural brain chemical) leading to a decrease in the excitability of neurons and thereby reducing the communication between neurons. Therefore, benzodiazepines produce a calming effect on many brain functions (Shalini et al., 2010). Benzodiazepines are the treatment of choice for the management of alcohol withdrawal symptoms. They reduce the signs and symptoms of alcohol withdrawal and also incidents of delirium and seizures (Sachdeva and Patel,2010). In delirium and seizures, lorazepam is the excellent one for the same effects because of its intermediate half-life, absence of active metabolite and high bioavailability (Rosenbloom et al., 1988). Benzodiazepines have disadvantages of being associated with drug dependence or benzodiazepine addiction. Dependence is known to develop with long-term use even at low therapeutic doses. Based on studies (Brett and Murnion, 2015; Airagnes et al., 2016),dependence and misuse of benzodiazepines have been of concern. The signs and symptoms of benzodiazepine dependence are feeling unable to manage without the drug,unsuccessful to stop benzodiazepine use, tolerance to benzodiazepines, and withdrawal symptoms when not taking the drug. Some prominent withdrawal symptoms that may appear include anxiety, depressed mood, depersonalization,sleep disturbance, hypersensitivity to touch and pain, tremors, muscular pains, twitches and headache (Jayaprakash,2014). Long-term use of benzodiazepines leads to physical and mental problems, so it is recommended for short-term use only. These factors lead to non-compliance in patients.It is therefore important to perform a study investigating the utilization patterns of benzodiazepines in different diseases in a given clinical setting. The present study aimed to assess the utilization patterns of benzodiazepines in psychiatric patients in a tertiary care teaching hospital.
SUBJECTS/METHODS
This is a prospective observational study involving patients admitted to the psychiatric department of a tertiary care teaching hospital. The study duration was 8 months (from July 2015 to February 2016). Before starting the study,the protocol was approved by the Nitte University Central Human Ethical Committee (approval number: REF: NU/CEC/ P.G.-10/2015).
Patients aged above 18 years, both genders, admitted in psychiatric wards, and prescribed with benzodiazepines were included in the study. In contrast, patients who were pregnant, lactating, mentally retarded and unconscious were excluded from the study.
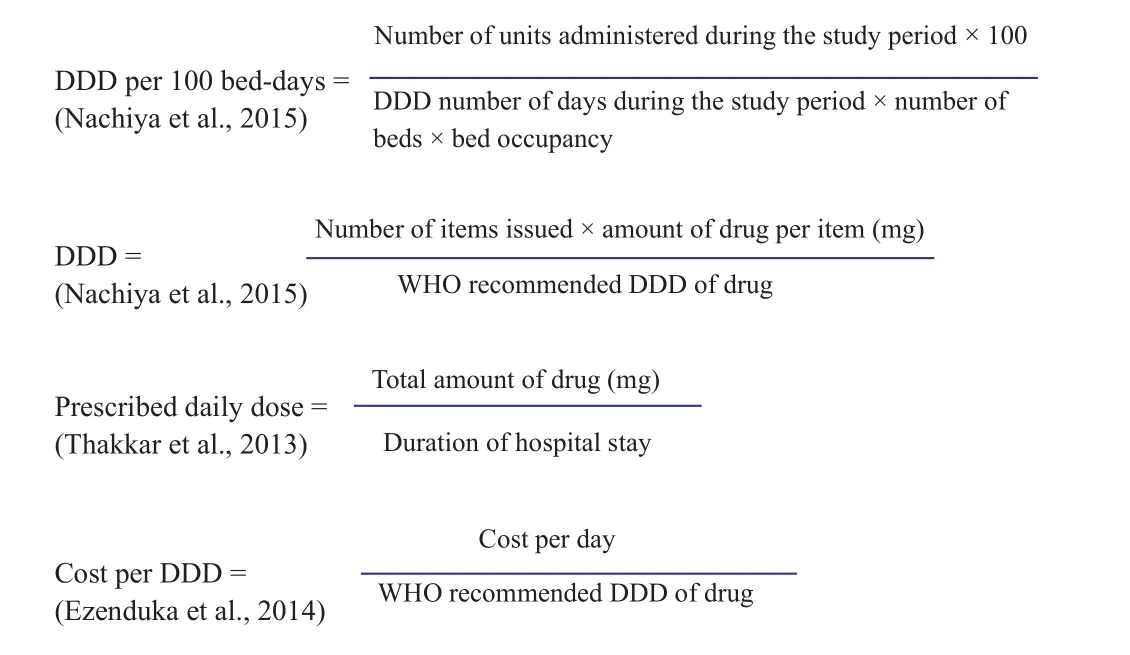
Patient data collection form was designed as per need of study. Patients receiving benzodiazepines were reviewed once daily and patient’s details including age, gender,past medical history, family history and social habits were recorded. Details of drug therapy such as name of drug,dosage, frequency, route of administration, duration of treatment, length of hospital stay, and number of drugs per prescription were recorded. In addition to that, the unit price of benzodiazepines was also recorded. Benzodiazepines were classified using Anatomical and Therapeutic Classification (ATC) system (WHO-ATC, 2016) and the consumption of benzodiazepines measured by defined daily dose (DDD) per 100 bed-days. The prescribed daily dose(PDD) and DDD of benzodiazepines were calculated by using the following formulas.
The number and percentages of benzodiazepines prescribed from National List of Essential Medicines of India(NLEM) 2011 and WHO Model List of Essential Medicine 2015 were calculated (WHO-NLEM, 2011; WHO-Essential Medicine, 2015). The cost analysis was calculated on the basis of cost per DDD. First, the cost per tablet was obtained and depending on the number of tablets per day, the total cost of tablets per day was calculated. Cost per DDD was then obtained by dividing total cost per day and DDD.
Sample size
Sample size was calculated by using the formula as below:
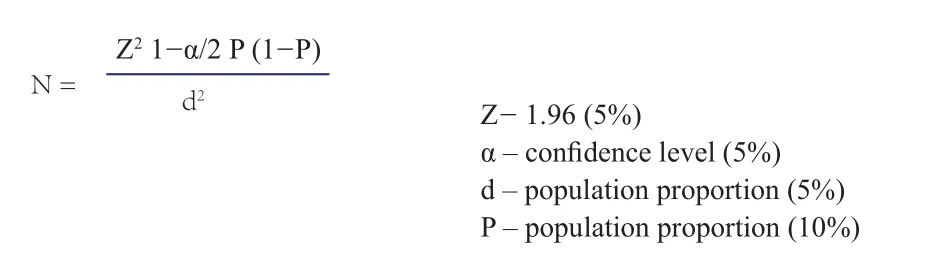
The minimum sample size required for this study was 138 patients.
Statistical analysis
Descriptive statistics was applied for analyzing the collected data. Data analysis was carried out using SPSS 16.0 software (SPSS, Chicago, IL, USA).
RESULTS
Patient demographic information
A total of 160 psychiatric patients receiving benzodiazepine therapy were included in the study. Most of the patients were aged 30-39 years (n = 53, 33.1%) followed by 40-49 years (n = 40, 25%). Age distributions of patients treatedwith benzodiazepines are summarized in the Table 1. Male patients (n = 142, 88.8%) outnumbered female patients (n= 18, 11.2%).
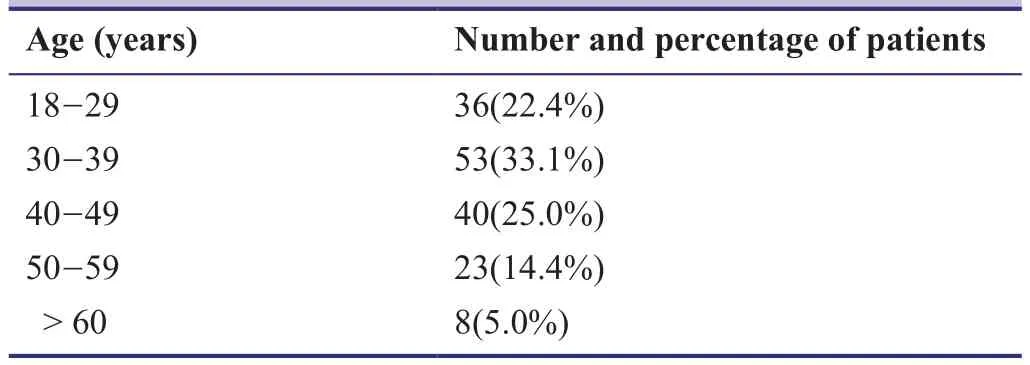
Table 1: Age group-wise distribution of patients treated with benzodiazepines
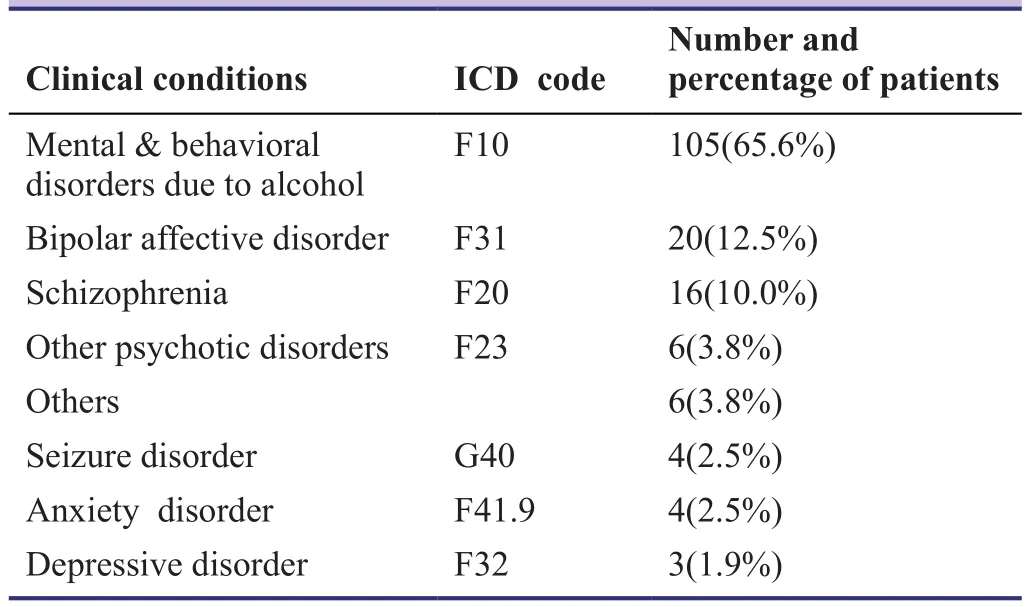
Table 2: Distribution pattern of patients according to clinical conditions
Distribution pattern of patients according to clinical conditions
During the study period, the most common clinical conditions of patients treated with benzodiazepines were mental and behavioural disorders due to alcohol (n = 105, 65.6%)followed by bipolar affective disorder (n = 20, 12.5%). The details of various clinical conditions of patients treated with benzodiazepines are summarized in Table 2.
Prescribing pattern of benzodiazepines
The majority of patients were prescribed lorazepam (n =133, 83.1%) followed by clonazepam (n = 23, 14.4%). The overall prescribing patterns of benzodiazepines in the study population are summarized in Table 3.
The ATC codes and DDD per 100 bed-days of benzodiazepines prescribed
The usage of benzodiazepine were calculated in termsof DDD per 100 bed-days. The DDD per 100 bed-days for benzodiazepines were 0.98. Lorazepam was the most commonly prescribed benzodiazepine (0.83 DDD per 100 bed-days) followed by diazepam (0.09 DDD per 100 beddays). The ATC codes and the DDD per 100 bed-days of the prescribed benzodiazepines are summarized in Table 4.
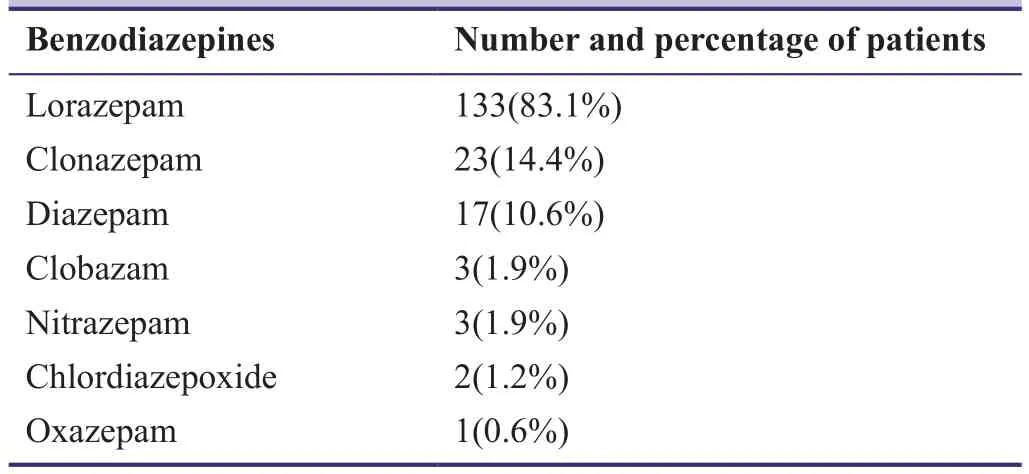
Table 3: Prescribing pattern of benzodiazepines
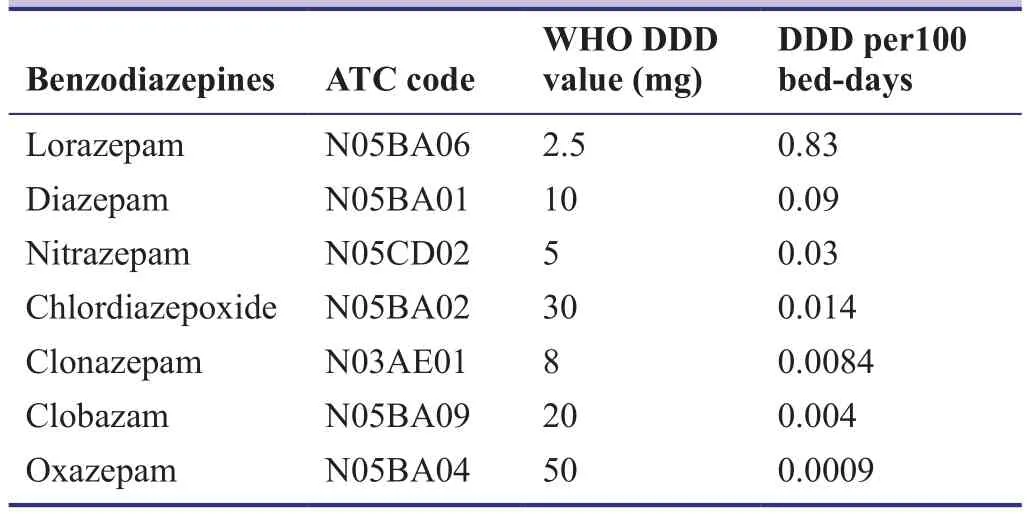
Table 4: ATC codes and DDD per 100 bed-days of benzodiazepines prescribed
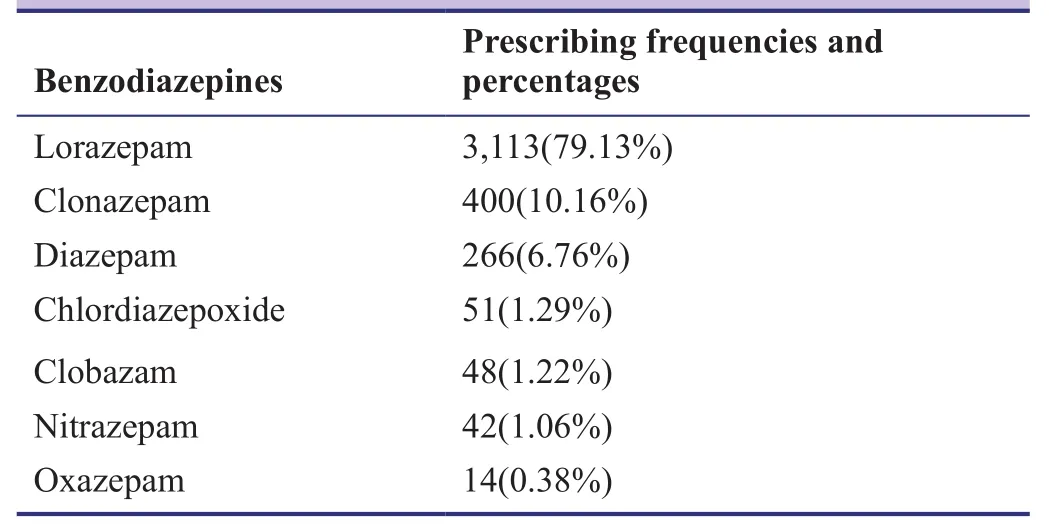
Table 5: Prescribing frequency by different benzodiazepines
Prescribing frequency for benzodiazepines
The most commonly prescribed benzodiazepines in dif-ferent psychiatric conditions during the study period was lorazepam (79.1%) followed by clonazepam (10.16%). The prescribing frequencies for different benzodiazepines are summarized in Table 5.
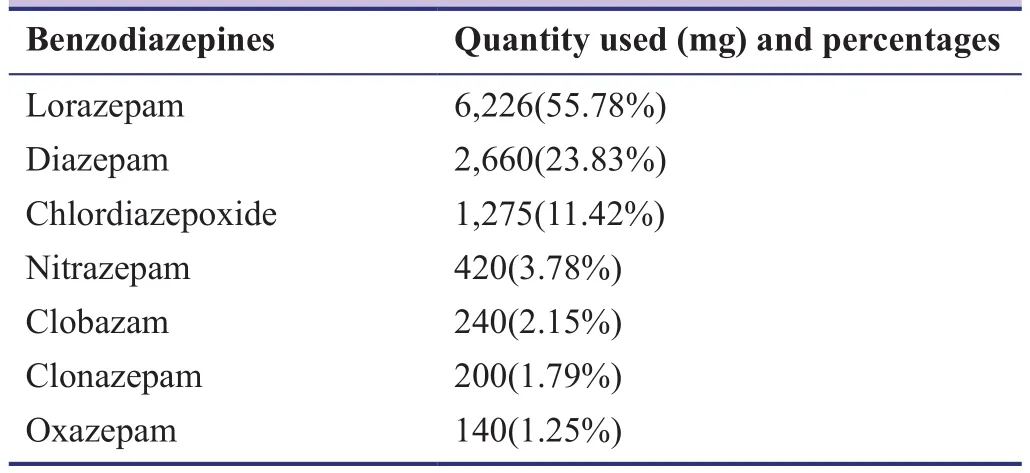
Table 6: Utilization of benzodiazepines in different psychiatric conditions
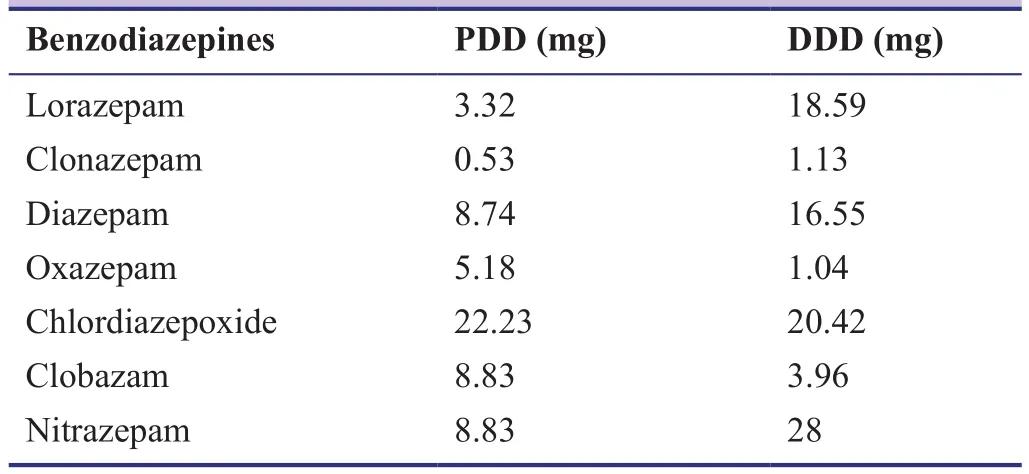
Table 7: Prescribled daily dose (PDD) and defined daily dose (DDD) of benzodiazepines during the hospitalization
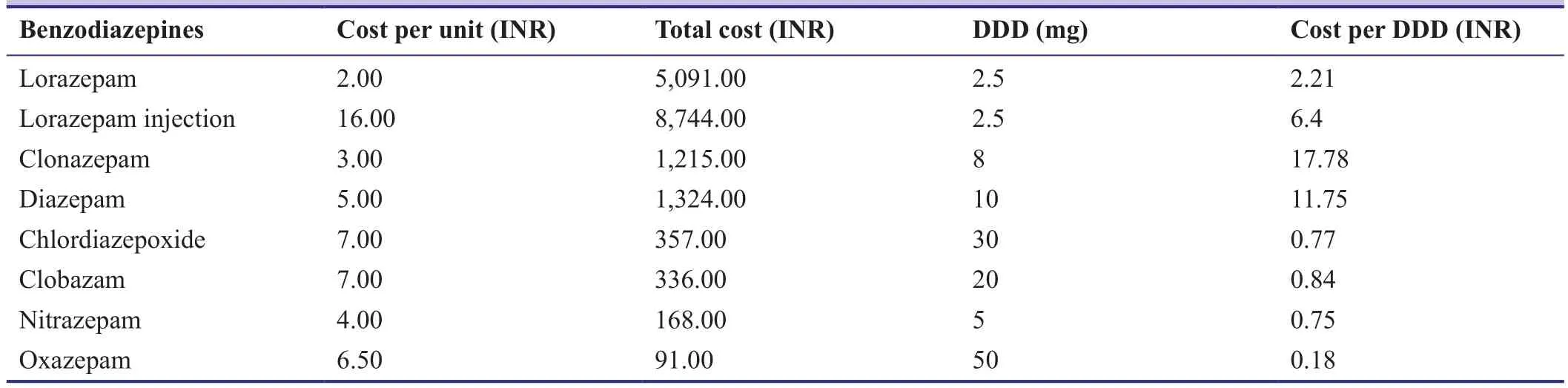
Table 8: Cost per defined daily dose (DDD)
Utilization of benzodiazepines in different psychiatric conditions
Out of 160 patients, the most commonly utilized benzodiazepines were lorazepam (55.5%) followed by diazepam(23.8%). Psychiatric conditions such as mental and behavioural disorders due to alcohol, bipolar affective disorder,anxiety disorder, seizure disorder, depressive disorder and schizophrenia were observed in the study. The utilization of benzodiazepines in different psychiatric conditions are summarized in Table 6.
PDD and DDD of benzodiazepine use during the hospitalization
PDD and DDD of benzodiazepines were calculated as per WHO collaborating centre for drug statistics methodology(ATC/DDD Index 2015). The mean and standard deviation of PDD and DDD of benzodiazepines were 57.16 ± 27.03 and 89.69 ± 39.16, respectively. The PDD and DDD of lorazepam were 3.32 and 18.59, respectively and clonazepam 0.53 and 1.13, respectively. PDD and DDD of benzodiazepines are summarized in Table 7.
Cost per DDD
Cost analysis was assessed by cost per unit and cost per DDD. The total cost of benzodiazepines in the prescription was 17,330 Indian Rupees (INR). Average cost per DDD of lorazepam was 2.21 INR followed by clonazepam 17.78 INR. Details on cost per DDD of benzodiazepines are summarized in Table 8.
DISCUSSION
The present study was conducted to find out the utilization of benzodiazepines in psychiatric inpatients. In this study,the majority of the patients were admitted in the age group of 30-39 years. Whereas in a study conducted by Jayaprakash(2014), the majority of patients were in the age group of 18-30 years. The proportion of male patients admitted to the psychiatric department was more than female patients.Similar findings were reported by Jayaprakash (2014) and Bodke and Bhosle (2014), where it was reported that male and female patients were 63% and 56.7%, respectively.
Mental and behavioral disorders due to use of alcohol was the most common (65.6%) clinical conditions in this study. Whereas the study results from Patel and Bhosle.(2013) showed that benzodiazepine utilization was more in both cardiovascular and infectious conditions (26%).While categorizing benzodiazepine prescriptions, it was observed that lorazepam (55.78%) was the most commonly prescribed drug in the psychiatric department. Similar results were reported by Sahana et al. (2010), where the most commonly used benzodiazepine was lorazepam and the overall percentage of benzodiazepines used was 73.1%and the similar results were also observed in the study conducted by Bodke and Bhosle (2014). A contradictory result was shown in a study carried out by Groeneweyen et al. (1999), where they found diazepam (23%) was the most commonly prescribed drug.
The present study showed that the most commonly prescribed benzodiazepine for treatment of alcohol withdrawal syndrome was lorazepam (55.5%). The similar findings were observed in the studies conducted by Rosenblom and Bhosle(1988) and Bird and Makela (1994). The studies conducted by Ozdemir et al. (1994) and Lejoyeux et al. (1998) also found that lorazepam was the drug of choice for the treatment of alcohol withdrawal syndrome. Our results indicated that the highest utilization drug among benzodiazepines was lorazepam. Similarly, Rathinavelu et al. (2015) and Juno et al. (2015) found DDD per 100 bed-days for antimicrobials and antipsychotics were 0.06 and 2.83687, respectively.
The PDD and DDD of lorazepam were higher than the results shown by Thakkar et al. (2013). The mean cost per DDD of lorazepam was 2.21 INR, which is lower than the study conducted by Stimac et al. (2009), where the cost per DDD of lorazepam was 0.1 INR. Ezenduka et al. (2014) also obtained a similar result (the total cost per DDD of lorazepam was 16 INR).
In conclusion, the present study evaluated the utilization of benzodiazepines in psychiatric patients. The majority of the patients admitted in the psychiatric department were suffering from mental and behavioural disorders due to alcohol. During the study period, the most commonly prescribed benzodiazepine was lorazepam. Clinical pharmacist in a health care team has an inevitable role for the essential and rational use of benzodiazepines by providing related information to the prescribers. This will definitely help to optimize the drug therapy, improve the quality of care and reduce the negative outcomes in the usage of benzodiazepines.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest
None declared.
Author contributions
UVM and PP designed the protocol. PP collected data. STS analyzed the data. UVM and PP wrote the paper. All authors approved the final version of the paper before publication.
We would like to thank Dr. Aneesh S Bhat from Department of Psychiatry, KSHEMA and Dr. D.S. Puranik, Former Head from the Department of Pharmacy Practice, NGSM Institute of Pharmaceutical Sciences for their valuable suggestions and guidance.We would also like to express our sincere gratitude to Dr. C.S.Shastry, Principal from Nitte Gulabi Shetty Memorial Institute of Pharmaceutical Sciences (NGSMIPS), Nitte University for providing necessary facilities to carry out this research.
Plagiarism check
This paper was screened twice using CrossCheck to verify originality before publication.
Peer review
This paper was double-blinded and stringently reviewed by international expert reviewers.
Airagnes G, Pelissolo A, Lavallée M, Flament M, Limosin F (2016)Benzodiazepine Misuse in the Elderly: Risk Factors, Consequences, and Management. Curr Psychiatry Rep 18:89.
Brett J, Murnion B (2015) Management of benzodiazepine misuse and dependence. Aust Prescr. 38:152-5.
Bird RD, Makela EH (1994) Alcohol withdrawal: What is the benzodiazepine of choice?. Ann Pharmacother 28:67-71.
Bodke P, Bhosle R (2014) Psychotropic drugs utilization pattern at tertiary care institute- a retrospective analysis. IJRTSAT 11:400-403.
Ezenduka CC, Ubochi VN, Ogbonna BO (2014) The utilization pattern and costs analysis of psychotropic drugs at a neuropsychiatric hospital in Nigeria. BJPR 4:325-337.
Groenewegen PP, Leufkens HG, Spreeuwenberg P, Worm W (1999)Neighbourhood characteristics and use of benzodiazepines in The Netherlands. Soc Sci Med 48:1701-1711.
Jayaprakash K (2014) Study of utilization pattern of benzodiazepines at a private corporate hospital. IJRPNS 3:357-361.
Juno JJ, Shastry CS, Satheesh R (2015) Evaluation of antipsychotic drug prescriptions in hospitalized schizophrenic patients. IJPRBS 4:353-363.
Lejoyeux M, Solomon J, Ades J (1998) Benzodiazepine treatment for alcohol-dependent patients. Alcohol Alcohol 33:563-575.
Nachiya J, Parimalakrishnan S, Ramakrishna RM (2015) Study on drug utilization pattern of antihypertensive medications on outpatients and inpatients in a tertiary care teaching hospital; A cross sectional study. Afr J Pharm Pharmacol 9:383-396.
Ozdemir V, Bremner KE, Naranjo CA (1994) Treatment of alcohol withdrawal syndrome. Ann Med 26:101-105.
Patel MJ, Syed AH, Qureshi AW (2013) Benzodiazepine use in medical out-patient clinics: a study from a developing country. J Pak Med Assoc 63:717-720.
Rathinavelu M, Satyagama S, Reddy R, Reddy YP (2015) Drug use evaluation of Antimicrobials in healthcare resource limited settings of India. IJOPP 8:191-195.
Rosenbloom A (1988) Emerging treatment options in the alcohol withdrawal syndrome. J Clin Psychiatry 49:28-32.
Sachdeva PD, Patel BG (2010) Drug Utilization studies-Scope and future perspectives. IJPBR 1:11-17.
Sahana DA, Keshava P, Rajeshwari S, Ullal S, Rathnakar UP, Jayakumar JS (2010) Pattern of psychotropic drug usage in psychiatric illness among elderly. J Med Use Dev Countries 2:3-10.
Shalini S, Ravichandran V, Mohanty BK, Dhanaraj SK, Saraswathy R (2010) Drug utilization studies- An overview. IJPSN 3:803-810.
Stimac D, Culig J (2009) Outpatient utilization of psychopharmaceuticals in the city of Zagreb 2001-2006. Psychiatria Danubina 21:56-64.
Thakkar KB, Jain MM, Billa G, Joshi A, Khobragade AA (2013) A drug utilization study of psychotropic drugs prescribed in the psychiatry out-patient department of a tertiary care hospital. J Clin Diagn Res 7:2759-2764.
WHO - Anatomical and Therapeutic Classification (ATC) system.Available from: http://www.whocc.no/atc_ddd_index/. (Last accessed on 10 Jan 2016)
WHO - National List of Essential Medicines (NLEM). Available from: http://www.who.int/selection_medicines/country_lists/India_NLME_2011.pdf. (Last accessed on 10 Jan 2016)
WHO Model List of Essential Medicine 2015. Available from:http://www.who.int/medicines/publications/essentialmedicines/EML2015_8-May-15.pdf. (Last accessed on 10 Jan 2016)
杂志排行
Asia Pacific Journal of Clinical Trials:Nervous System Diseases的其它文章
- Homeopathic prophylaxis for recurrent urinary tract infections following spinal cord injury: study protocol for a randomized controlled trial
- Effectiveness of cerebellar repetitive transcranial magnetic stimulation in essential tremor: study protocol for a randomized, sham-controlled trial
- Bispectral index-guided fast track anesthesia by sevoflurane infusion combined with dexmedetomidine for intracranial aneurysm embolization: study protocol for a multi-center parallel randomized controlled trial
- Cognitive function and biomarkers after traumatic brain injury:protocol for a prospective inception cohort study
- Electroencephalographic changes following trigeminal nerve stimulation for major depressive disorder: study protocol for a randomized sham-controlled trial
- Effect of intravenous acetaminophen on post-operative opioidrelated complications: study protocol for a randomized,placebo-controlled trial