骨质疏松性椎体压缩骨折不同时期保守和微创治疗的疗效比较
2016-01-11陈小兵,赵洪普
·论著·
骨质疏松性椎体压缩骨折不同时期保守和微创治疗的疗效比较
陈小兵,赵洪普
作者单位:510150广东省广州市,广州医科大学附属第三医院骨科一区
通信作者:陈小兵,510150广东省广州市,广州医科大学附属第三医院骨科一区;E-mail:xbhd88@163.com
【摘要】背景我国医改逐步实行分级诊疗,老龄化社会中骨质疏松性椎体压缩骨折(OVCF)患者增多。保守治疗和微创治疗是主要治疗方法,治疗方法和时期不同,效果有差异,以此为临床医生选择治疗方法提供参考。目的比较微创治疗和保守治疗对OVCF不同时期患者治疗效果的差异。方法收集2009年1月—2014年1月在广州医科大学附属第三医院骨外科住院治疗的临床资料完整且有随访资料的OVCF患者197例,以受伤到医院接受正规治疗的时间为标准,将患者分为0~7 d治疗组(A组,79例)、8~21 d治疗组(B组,60例)、>21 d治疗组(C组,58例)。再根据住院期间患者所采用的治疗方法,将各组中采用经皮椎体成形术(PVP)或经皮椎体后凸成形术(PKP)治疗者分为微创亚组,将采用体位复位、支具固定、功能锻炼、药物治疗而没有采用PVP或PKP治疗者分为保守亚组。观察不同时期采用不同方法治疗的患者治疗前及治疗后24 h、1周、末次随访的视觉模拟评分(VAS)、Oswestry功能障碍指数问卷(ODI)评分、治疗期间并发症的发生情况。结果A组:两亚组治疗前后VAS、ODI评分时间与组间存在交互作用(P<0.05);时间比较:治疗前后VAS、ODI评分比较,差异有统计学意义(P<0.05);组间比较:治疗后24 h、7 d、末次随访,两亚组VAS、ODI评分比较,差异有统计学意义(P<0.05)。微创亚组并发症发生率为7.1%(3/42),低于保守亚组的37.8%(14/37)(χ2=10.974,P<0.05)。B组:两亚组治疗前后VAS、ODI评分时间与组间存在交互作用(P<0.05);时间比较:治疗前后VAS、ODI评分比较,差异有统计学意义(P<0.05);组间比较:治疗后24 h、7 d、末次随访,两亚组VAS比较,差异有统计学意义(P<0.05);两亚组ODI评分比较,差异无统计学意义(P>0.05)。微创亚组并发症发生率为6.7%(2/30),低于保守亚组的43.3%(13/30)(χ2=10.756,P<0.05)。C组:两亚组治疗前后VAS、ODI评分时间与组间存在交互作用(P<0.05);时间比较:治疗前后VAS、ODI评分比较,差异有统计学意义(P<0.05);组间比较:治疗后24 h、7 d、末次随访,两亚组VAS、ODI评分比较,差异无统计学意义(P>0.05)。微创亚组并发症发生率为7.1%(2/28),低于保守亚组的30.0%(9/30)(χ2=4.923,P<0.05)。结论OVCF患者在损伤后21 d内进行微创治疗的效果优于保守治疗,而超过21 d进行治疗时微创和保守治疗在疼痛缓解和功能恢复方面差异不明显,但微创治疗并发症发生率低于保守治疗。
【关键词】骨质疏松性骨折;骨折,压缩性;微创治疗;保守治疗
【中图分类号】R 683
收稿日期:(2014-11-02;修回日期:2015-08-13)
陈小兵,赵洪普.骨质疏松性椎体压缩骨折不同时期保守和微创治疗的疗效比较[J].中国全科医学,2015,18(35):4320-4324.[www.chinagp.net]
Chen XB,Zhao HP.Efficacy comparison between conservative treatment and minimally invasive treatment in different time periods of osteoporotic vertebral compression fracture[J].Chinese General Practice,2015,18(35):4320-4324.
Efficacy Comparison Between Conservative Treatment and Minimally Invasive Treatment in Different Time Periods of Osteoporotic Vertebral Compression FractureCHENXiao-bing,ZHAOHong-pu.DepartmentofOrthopedics,theThirdAffiliatedHospitalofGuangzhouMedicalUniversity,Guangzhou510150,China
Abstract【】BackgroundThe classification of diagnosis and treatment has been gradually carried out in the medical reform in China.In the aging population of China,the number of patients with osteoporotic vertebral compression fracture(OVCF)has been increasing.Conservative treatment and minimally invasive treatment are the primary treatment methods for the disease,while they have efficacy differences in different time periods,which may provide a reference for clinical doctors.ObjectiveTo compare the therapeutic efficacy of minimally invasive treatment with that of conservative treatment in different periods of OVCF.MethodsWe collected the clinical data and follow-up data of 197 OVCF patients who received hospitalized treatment in the Third Affiliated Hospital of Guangzhou Medical University from January 2009 to January 2014.According to the time range from getting injured to the beginning of formal treatment,the patients were divided into three groups:0-7 d group(group A,n=79),8-21 d group(group B,n=60)and >21 d group(group C,n=58).According to the treatment method used,the patients who received percutaneous vertebroplasty(PVP)or percutaneous kyphoplasty(PKP)were assigned into minimal invasion subgroup,and the patients who received postural reduction,braces fixation,functional exercise and drug therapy instead of PVP or PKP were assigned into conservation subgroup.Data about VAS,ODI score and complications were collected before treatment,24 hours after treatment,1 week after treatment and in the last follow-up visit.ResultsIn group A,interaction effect was found between the two subgroups before and after treatment in VAS and ODI score by temporal comparison and inter-group comparison(P<0.05);by temporal comparison,VAS and ODI score after treatment were significantly different from those before treatment(P<0.05);by inter-group comparison,24 h,7 d after treatment and at last follow-up,the two subgroups were significantly different in VAS and ODI score irrespective of measuring time(P<0.05);the complication incidence of minimally invasive subgroup was 7.1%(3/42),lower than that of conservation group,which was 37.8%(14/37)(χ2=10.974,P<0.05).In group B,interaction effect was found between the two subgroups before and after treatment in VAS and ODI score by temporal comparison and inter-group comparison(P<0.05);by temporal comparison,VAS and ODI score after treatment were significantly different from those before treatment(P<0.05);by inter-group comparison,the two subgroups were significantly different in VAS 24 h,7 d after treatment and at last follow-up(P<0.05) ,and were not significantly in ODI score(P>0.05);the complication incidence of minimal invasion subgroup was 6.7%(2/30),lower than that of conservation group,which was 43.3%(13/30)(χ2=10.756,P<0.05).In group C,interaction effect was found between the two subgroups before and after treatment in VAS and ODI score by temporal comparison and inter-group comparison(P<0.05);by temporal comparison,VAS and ODI score after treatment were significantly different from those before treatment(P<0.05);by inter-group comparison,the two subgroups were not significantly different in VAS and ODI score 24 h,7 d after treatment and at last follow-up(P>0.05);the complication incidence of minimally invasive subgroup was 7.1%(2/28),lower than that of conservation group,which was 30.0%(9/30)(χ2=4.923,P<0.05).ConclusionThe efficacy of minimally invasive treatment within 21 days after injury is better than conservative treatment for osteoporotic vertebral compression fracture,while the two therapies have no obvious differences in relieving pain and restoring function in more than 21 days after injury,yet the complication incidence by minimally invasive treatment is lower than conservative treatment.
【Key words】Osteoporotic fractures;Fractures,compression;Minimally invasive treatment;Conservative treatment
随着我国老年人口增多,骨质疏松性椎体压缩骨折(osteoporotic vertebral compression fractures,OVCF)患病率增高,成为临床常见疾病[1-3],也是影响老年人生活质量的常见病[4-6]。OVCF相对容易诊断,治疗方法主要有保守治疗和以经皮椎体成形术(percutaneous vertebral plasty,PVP)、经皮椎体后凸成形术(percutaneous keratoplasty,PKP)为主的微创治疗,治疗效果有差异[7]。有研究报道微创治疗在OVCF急性期优于保守治疗,而6个月后两者无明显差异[3,8]。也有研究报道在OVCF慢性期行PVP效果优于保守治疗[9]。本研究旨在探讨OVCF不同时期选择不同治疗方法效果有无差异,为临床选择治疗方法提供参考。
1资料与方法
1.1研究对象收集2009年1月—2014年1月在广州医科大学附属第三医院骨外科住院治疗的临床资料完整且有随访资料的OVCF患者197例,其中男71例,女126例;年龄60~95岁,平均年龄(75.7±11.6)岁;病因:跌伤129例,无诱因27例,扭伤11例,高处坠落11例,搬重物7例,他科转入(病因不明确)6例,轻微车祸3例,撞伤(非车祸)2例,电击伤1例;主要临床表现为腰痛;骨折椎体分布:T6~L5;按照Genant分级方法[10]进行骨折椎体分型:依据侧位胸腰椎X线片椎体高度降低百分比,分为轻度压缩(15%~25%)59例,中度压缩(26%~40%)114例和重度压缩(>40%)24例。患者均进行胸腰椎X线片、双能X线骨密度测定等检查,依据WHO标准[11-12]诊断为骨质疏松症。其中骨密度测定采用美国GE公司的GE-Prodigy双能X线新型骨密度测定仪,常规测定L1~4椎体和股骨颈的骨密度,取T值。排除:严重车祸、严重高处坠落伤、脊柱爆裂性骨折压迫脊髓、合并椎管狭窄下肢神经症状明显,需行非微创手术治疗者。
1.2组别以受伤到医院接受正规治疗的时间为依据,将患者分为0~7 d治疗组(A组,79例)、8~21 d治疗组(B组,60例)、>21 d治疗组(C组,58例)。再根据住院期间患者所采用的治疗方法,将各组中采用PVP或PKP治疗者分为微创亚组,将采用体位复位、支具固定、功能锻炼、药物治疗而没有采用PVP或PKP治疗者分为保守亚组。3组中各亚组之间性别、年龄、骨折平面(L1~2)、入院视觉模拟评分(VAS)、骨折椎体分型、T值比较,差异均无统计学意义(P>0.05,见表1~3)。

表1 A组患者两亚组一般资料比较
注:a为χ2值;VAS=视觉模拟评分
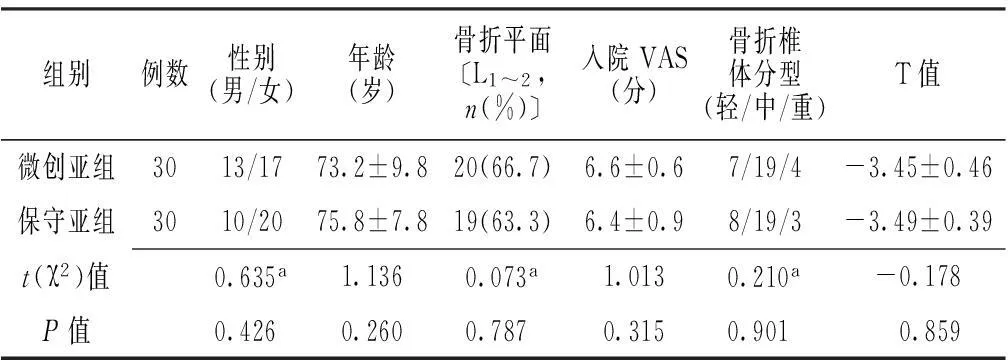
表2 B组患者两亚组一般资料比较
注:a为χ2值
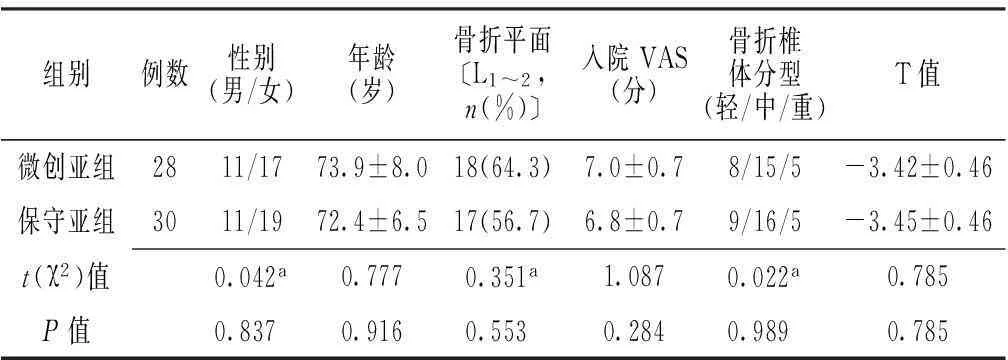
表3 C组患者两亚组一般资料比较
注:a为χ2值
1.3治疗方法入院后完善胸腰椎X线片以及磁共振、CT和双能X线骨密度等检查,明确诊断以及引起此次疼痛的骨折责任椎。保守治疗:(1)体位复位:仰卧硬板床,在背部骨折部垫高度约4 cm软枕并腰围外固定。(2)功能锻炼:入院3~5 d疼痛缓解后开始指导患者挺腹,手足头部支撑锻炼腰背肌;10~14 d后,若患者症状好转,尝试在腰围或支具保护下以及护理人员辅助下开始下地活动。(3)止痛治疗:期间疼痛按照WHO疼痛治疗指南[13]给予相应的镇痛治疗,常用药物:曲马多、依托考昔、塞来昔布胶囊、双氯芬酸软膏等。(4)抗骨质疏松治疗:入院后如无禁忌证,即开始予以药物抗骨质疏松治疗,常选用钙尔奇D片、骨化三醇、阿仑膦酸钠、鲑鱼降钙素等。
手术治疗:一般根据压缩骨折椎体后壁完整性等选择PVP或PKP,后壁完整者常采用PVP,后壁不完整者常采用PKP。手术方法:(1)复位:俯卧于骨科手术床上,肩部及骨盆部垫高,腹部悬空,以责任椎为中心调整手术床行脊柱过伸位复位。(2)定位:C型臂X线机透视下定位,明确责任椎体和两侧椎弓根,并标记。(3)穿刺:常规背部消毒、铺无菌巾。1%利多卡因局部逐层浸润麻醉,在C型臂X线机引导下,行椎弓根入路,置入工作管道,PKP则通过工作管道置入球囊扩张器,加压球囊扩张。(4)骨水泥注射:调制骨水泥成拉丝状,经专用注射器由工作管道注入,过程中透视监视,待骨水泥弥散良好后停止注射,骨水泥凝固后稍旋转拔出穿刺针,无菌敷料覆盖术口。(5)术后治疗:术后常规观察生命体征、术口疼痛和双下肢活动感觉情况。术后6 h可床上翻身坐起,术后1 d可以锻炼腰背肌,术后2 d可在腰围保护下下地活动。抗骨质疏松治疗、止痛治疗方案同保守治疗。
1.4疗效评价方法观察指标:观察不同时期不同方法治疗的患者治疗前及治疗后24 h、7 d、末次随访的VAS,Oswestry功能障碍指数问卷(Oswestry Diability Index,ODI)评分,治疗期间并发症(常见并发症有:尿路感染、压疮、肺部感染、心功能不全、消化性溃疡出血等)。VAS:在纸上划一条10 cm的横线,患者根据自我感觉在横线上划一记号,表示疼痛的程度,据标示分数而评分,评分越高表示疼痛越严重[14]。ODI是由10个问题组成的评分表,表中包含关于疼痛的强度、生活自理、提物、步行、坐位、站立、干扰睡眠、性生活、社会生活、旅游等10个方面,每个问题6个选项,单个问题最高得分为5分,选择第一项得分为0分,选择最后一项得分为5分,中间得分依次递增,假如有10个问题都做了问答,记分方法是:实际得分/50(最高可能得分)×100%,评分越高表明功能障碍越严重[15]。

2结果
2.1A组两亚组治疗前后VAS、ODI评分时间与组间存在交互作用(P<0.05);时间比较:治疗前后VAS、ODI评分比较,差异有统计学意义(P<0.05);组间比较:治疗后24 h、7 d、末次随访,两亚组VAS、ODI评分比较,差异有统计学意义(P<0.05,见表4)。微创亚组并发症发生率为7.1%(3/42),保守亚组为37.8%(14/37),两亚组并发症发生率比较,差异有统计学意义(χ2=10.974,P<0.05)。
2.2B组两亚组治疗前后VAS、ODI评分时间与组间存在交互作用(P<0.05);时间比较:治疗前后VAS、ODI评分比较,差异有统计学意义(P<0.05);组间比较:治疗后24 h、7 d、末次随访,两亚组VAS比较,差异有统计学意义(P<0.05);两亚组ODI评分比较,差异无统计学意义(P>0.05,见表5)。微创亚组并发症发生率为6.7%(2/30),保守亚组为43.3%(13/30),两亚组并发症发生率比较,差异有统计学意义(χ2=10.756,P<0.05)。
2.3C组两亚组治疗前后VAS、ODI评分时间与组间存在交互作用(P<0.05);时间比较:治疗前后VAS、ODI评分比较,差异有统计学意义(P<0.05);组间比较:治疗后24 h、7 d、末次随访,两亚组VAS、ODI评分比较,差异无统计学意义(P>0.05,见表6)。微创亚组并发症发生率为7.1%(2/28),保守亚组为30.0%(9/30),两亚组并发症发生率比较,差异有统计学意义(χ2=4.923,P<0.05)。
3讨论
随着医疗技术的发展和人们生活水平的提高,目前OVCF患者多选择微创治疗[16-17]。本研究结果提示,OVCF损伤后建议早期治疗,在损伤后21 d内治疗效果较好并且并发症发生风险相对较低。而时间较长,超过21 d,微创治疗和保守治疗在疼痛缓解和功能恢复方面差异不明显,但微创治疗并发症发生率低于保守治疗。考虑是损伤后早期患者因为压缩性骨折所引起的症状明显,早期手术治疗,骨折处及时复位和骨水泥较稳固的固定和支撑;并且骨水泥硬化过程中释放的热量对骨折处的感觉神经末梢的变性作用,均可以起到止痛和改善功能的作用,而卧床时间延长,会增加卧床并发症的发生,不利于抗骨质疏松治疗[9,17],所以早期微创治疗,效果相对较好[18-19]。而随着时间延长,患者会自行休息和药物治疗;另外骨折处也在自然生长,相对稳定性好转;并且年龄较大的患者合并有骨质增生症、椎管狭窄等疾病,也会引起腰部疼痛等症状,故而单纯因椎体压缩性骨折所引起的症状有所减少,所以治疗效果在缓解疼痛和改善生活质量方面和保守治疗相比并不是很明显。
本研究的不足之处在于评价指标主要是评分,患者主观性较高,客观性检查资料较少,变异性较大;老年患者常合并有腰椎骨质增生、椎管狭窄等病变,症状不是全由OVCF所引起,研究中没有将这些因素均衡化;

表4 A组两亚组不同时间VAS、ODI评分比较 ,分)
注:ODI=Oswestry功能障碍指数问卷

表5 B组两亚组不同时间VAS、ODI评分比较 ,分)

表6 C组两亚组不同时间VAS、ODI评分比较 ,分)
另外,本研究没有对3个时期,尤其是7 d和8~21 d微创治疗效果的比较。有研究称,在亚急性期进行微创治疗效果较好[20];也有研究称,早期手术效果较好[17]。本研究结果显示:对于OVCF患者来说,在3周前进行治疗,微创治疗较保守治疗效果好;3周后微创治疗和保守治疗在缓解疼痛和改善功能方面差异不显著,但是微创治疗并发症发生率低于保守治疗。
综上所述,OVCF早期积极微创治疗效果较好,因这类骨折常是轻微的跌伤或者是没有明显诱因下而出现的腰背部疼痛,临床医生需要有敏锐的思维,并且需要及时进行胸腰部X线片等检查予以辅助诊断,早期诊断,早期治疗。如果症状较明显,损伤时间较短,建议患者早期到有条件的医院进行微创治疗,而对于损伤时间比较长,特别是合并有骨质增生症、椎管狭窄等多种会引起腰背疼痛疾病的患者,在基层保守治疗,也不失是经济有效的治疗方法,但是需要加强护理和康复治疗,尽量减少卧床并发症的发生。
参考文献
[1]Fang Y,Ding GX,Zhang HM,et al.Risk assessment of osteoporotic fractures among the elderly in community[J].Chinese General Practice,2012,15(9):2900-2992.(in Chinese)
方圆,丁国兴,张慧敏,等.社区中老年人骨质疏松性骨折风险评估研究[J].中国全科医学,2012,15(9):2900-2992.
[2]Huang K,Du XP,Sun YG.Research progress in osteoporosis screening technology and its application in community[J].Chinese General Practice,2013,16(3):836-838.(in Chinese)
黄凯,杜雪平,孙艳格.骨质疏松症社区筛查技术研究进展及其推广应用[J].中国全科医学,2013,16(3):836-838.
[3]Buchbinder R,Osborne RH,Ebeling PR,et al.A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures[J].N Engl J Med,2009,361(6):557-568.
[4]Nielson CM,Marshall LM,Adams AL,et al.BMI and fracture risk in older men:the osteoporotic fractures in men study (MrOS)[J].J Bone Miner Res,2011,26(3):496-502.
[5]Sànchez-Riera L,Wilson N,Kamalaraj N,et al.Osteoporosis and fragility fractures[J].Best Pract Res Clin Rheumatol,2010,24(6):793-810.
[6]Kim HW,Song JW,Kwon A,et al.Extreme multi-level percutaneous vertebroplasty for newly developed multiple adjacent compression fractures[J].J Korean Neurosurg Soc,2009,45(6):378-380.
[7]Du H,Tian XX,Zhang XQ,et al.Comparison of PVP with conservative therapy in treatment of elderly osteoporotic thoracolumbar vertebral compression fracture[J].Chinese General Practice,2013,16(5):1629-1632.(in Chinese)
杜浩,田笑笑,张晓强,等.经皮椎体成形术与保守法治疗老年骨质疏松性胸腰椎压缩骨折的疗效比较研究[J].中国全科医学,2013,16(5):1629-1632.
[8]Eck JC,Nachtigall D,Humphreys SC,et al.Comparison of vertebroplasty and balloon kyphoplasty for treatment of vertebral compression fractures:a meta-analysis of the literature[J].Spine J,2008,8(3):488-497.
[9]Li H,Gu YF,Li YD,et al.Comparison of percutaneous vertebroplasty with conservative measures for chronic painful osteoporotic spinal fractures:a nonrandomized prospective trial[J].Journal of Interventional Radiology,2012,21(11):921-926.(in Chinese)
李卉,顾一峰,李永东,等.比较经皮椎体成形术与保守治疗对慢性疼痛性骨质疏松性椎体骨折患者疗效的非随机前瞻性试验[J].介入放射学杂志,2012,21(11):921-926.
[10]Genant HK,Wu CY,Van Kuijk C,et al.Vertebral fracture assessment using a semiquantitative technique[J].J Bone Miner Res,1993,8(9):1137-1148.
[11]Assessment of fracture risk and its application to screening for postmenopausal osteoporosis.Report of a WHO Study Group[J].World Health Organ Tech Rep Ser,1994,843:1-129.
[12]Kanis JA,Mccloskey EV,Johansson H,et al.A reference standard for the description of osteoporosis[J].Bone,2008,42(3):467-475.
[13]Mchugh GA,Luker KA,Campbell M,et al.A longitudinal study exploring pain control,treatment and service provision for individuals with end-stage lower limb osteoarthritis[J].Rheumatology(Oxford),2007,46(4): 631-637.
[14]Huskisson EC.Measurement of pain[J].Lancet,1974,2(7889):1127-1131.
[15]Fairbank JC.Oswestry disability index[J].J Neurosurg Spine,2014,20(2):239-241.
[16]Zhang L,Li J,Yang H,et al.Histological evaluation of bone biopsy results during PVP or PKP of vertebral compression fractures[J].Oncol Lett,2013,5(1):135-138.
[17]李亮,于学忠,隋海涛,等.不同时期骨质疏松性椎体压缩性骨折行经皮椎体后凸成形术的疗效分析[J].中国医师进修杂志,2013,36(11):58-61.
[18]Liu Y,Zhang HP,Zhao GZ.Observation of clinical curative effect of PKP of osteoporotic vertebral body occult fracture in postmenopausal women[J].Chinese General Practice,2013,14(9):2989-2991.(in Chinese)
刘瑶,张华朋,赵光宗.PKP治疗绝经后妇女骨质疏松性椎体隐匿性骨折的临床疗效观察[J].中国全科医学,2013,14(9):2989-2991.
[19]Xie ZJ,Li SG,Chen GB,et al.Therapeutic effect of percutaneous vertebroplasty and percutaneous kyphoplasty of osteoporotic vertebral compression fractures in old people[J].Chinese Journal of Gerontology,2013,33(13):3200-3201.(in Chinese)
谢振钧,李仕国,陈广滨,等.经皮椎体成形术及经皮椎体后凸成形术治疗老年骨质疏松性椎体压缩骨折的效果[J].中国老年学杂志,2013,33(13):3200-3201.
[20]Oh GS,Kim HS,Ju CI,et al.Comparison of the results of balloon kyphoplasty performed at different times after injury[J].J Korean Neurosurg Soc,2010,47(3):199-202.
(本文编辑:贾萌萌)
