75岁及以上老年患者经皮冠状动脉介入治疗术后远期预后的性别差异
2015-12-16王玉珏高展杨进刚袁晋青徐波杨跃进陈珏陈纪林乔树宾吴永健颜红兵高润霖
王玉珏,高展,杨进刚,袁晋青,徐波,杨跃进,陈珏,陈纪林,乔树宾,吴永健,颜红兵,高润霖
临床研究
75岁及以上老年患者经皮冠状动脉介入治疗术后远期预后的性别差异
王玉珏,高展,杨进刚,袁晋青,徐波,杨跃进,陈珏,陈纪林,乔树宾,吴永健,颜红兵,高润霖
目的:评价75岁及以上老年患者在经皮冠状动脉介入治疗(PCI)术后远期预后是否存在性别差异。
方法:连续入选2004-04至2010-11期间在我院行PCI的29 211例冠心病患者,分为:≥75岁女性组(521例)、<75岁女性组(5 666例)、≥75岁男性组(1 098例)和<75岁男性组(21 926例)。比较各组患者PCI术后住院期和远期预后。
结果:住院期间,≥75岁女性组心原性死亡发生率明显高于其他三组。COX比例风险模型分析显示:与<75岁女性及<75岁男性比,≥75岁女性是心原性死亡(HR=2.53,95% CI:1.15~5.59;HR=2.22,95% CI:1.26~3.91)和心原性死亡/心肌梗死(HR=2.26,95% CI:1.27~4.03;HR=2.25,95% CI:1.44~3.51)的独立危险因素。但与≥75岁男性相比,≥75岁女性不是心原性死亡(HR=1.30)和心原性死亡/心肌梗死(HR=1.21)的独立危险因素。
结论:与其他人群相比,75岁及以上老年女性PCI术后住院期和远期预后较差,但其不是PCI术后预后不佳的独立危险因素。
经皮冠状动脉介入治疗;老年女性;随访
(Chinese Circulation Journal, 2015,30:438.)
与男性冠心病患者相比,导致女性患者预后不良的危险因素更多,例如:体型小、动脉内径小、激素水平不同、冠状动脉(冠脉)反应异常(内皮功能障碍)[1]、微血管障碍[2]、斑块形态不同[3,4],这些因素在理论上可导致女性患者预后较差,但既往大量关于女性是否为经皮冠状动脉介入治疗(PCI)后独立危险因素的研究未得出一致的结论[5-16],而有研究证实年龄为一个独立危险因素[17]。因此,或许是老年女性,而非女性作为一个整体,是PCI预后不良的独立危险因素。本研究旨在通过比较75岁及以上老年女性与其他人群PCI后住院期和远期预后,分析75岁及以上老年患者PCI术后远期预后是否存在性别差异。
1 资料和方法
研究对象:连续入选2004-04至2010-11在我院行PCI的29 211例冠心病患者。≥75岁女性组521例、<75岁女性组5 666例、≥75岁男性组1 098例和<75岁男性组21 926例。
PCI及术后用药:PCI治疗策略和支架类型选用由术者决定。≥75岁女性组患者共848个病变, <75岁女性组患者共9 476个病变, ≥75岁男性组患者共1 892个病变,<75岁男性组共38 442个病变。对于没有禁忌的患者,术前至少24 h口服阿司匹林 300 mg/d,同时服用氯吡格雷300 mg负荷量。术中经动脉鞘管根据体重给予肝素100 U/kg,由术者决定是否使用血小板糖蛋白Ⅱb/Ⅲa受体拮抗剂。术后继续口服阿司匹林100 mg/d,氯吡格雷75 mg/d:置入裸金属支架患者至少口服3个月、药物洗脱支架患者至少服用1年。
随访:住院期间及出院1、3、6个月和1、2、3年进行门诊和电话随访,记录心原性死亡、非致死性心肌梗死、靶血管血运重建(TVR)和主要不良心血管事件(MACE)。如患者有心肌缺血症状或临床证据,建议其复查冠状动脉造影,用定量冠状动脉造影(QCA)进行评价。
相关定义:(1)介入成功:手术结束时,血管内残余狭窄小于30%,前向血流心肌梗死溶栓治疗临床试验(TIMI)3级。(2)心肌梗死:缺血性症状合并心电图变化和(或)肌酸激酶同工酶(CK-MB)的动态演变(CK-MB升高大于正常高限的3倍及以上)。(3)TVR:对曾行支架治疗的血管再次行PCI或冠状动脉旁路移植术治疗。(4)心原性死亡:不能找到非心原性病因的死亡。(5)MACE:包括心原性死亡、心肌梗死和TVR。(6)参照血管:病变近端或远端的正常血管。
2 结果
患者基线特点(表1、2):基线临床特点方面,与其他三组患者相比,≥75岁女性组糖尿病、高血压患者的比例较高,吸烟者的比例较低。在病变特点方面,≥75岁女性组多支血管病变、钙化和闭塞病变的比例较高,而参照血管直径小于其他三组。在介入操作特点上,≥75岁女性组急诊PCI的比例较高,而经桡动脉路径双球囊对吻技术、分叉病变双支架技术的比例较低。
随访期间临床疗效:本研究平均随访时间15个月,失访共4 323例,失访率14.8%,其中3 308例多次打电话未通,981例拒绝或无法提供患者情况,34例死亡,但家属拒绝说明死亡原因。
住院期间,≥75岁女性组的MACE发生率明显高于<75岁女性组和<75岁男性组(P<0.05),差异有统计学意义;而与≥75岁男性组相比差异无统计学意义。其中≥75岁女性组的心原性死亡发生率明显高于其他三组患者(P<0.05)。≥75岁女性组的心肌梗死发生率明显高于<75岁女性组和<75岁男性组(P<0.05),差异均有统计学意义,而与≥75岁男性组相比差异无统计学意义。≥75岁女性组的TVR与其他三组相比差异无统计学意义(表3)。
COX比例风险模型分析在调整潜在的混杂因素(包括陈旧性心肌梗死、既往PCI、既往冠状动脉旁路移植术、糖尿病、高血压、不稳定性心绞痛、左主干病变、支架数量、病变数量、药物洗脱支架比例、支架直径、支架长度、后扩张和血管内超声)后显示:与<75岁女性和<75岁男性比,≥75岁女性是心原性死亡(HR=2.53,95% CI:1.15~5.59;HR=2.22,95% CI:1.26~3.91)和心原性死亡/心肌梗死(HR=2.26,95% CI:1.27~4.03;HR=2.25,95% CI:1.44~3.51)的独立危险因素。但与≥75岁男性相比,≥75岁女性不是心原性死亡(HR=1.30,95%CI:0.97~1.71)和心原性死亡/心肌梗死(HR=1.21,95%CI:0.94~1.55)的独立危险因素。
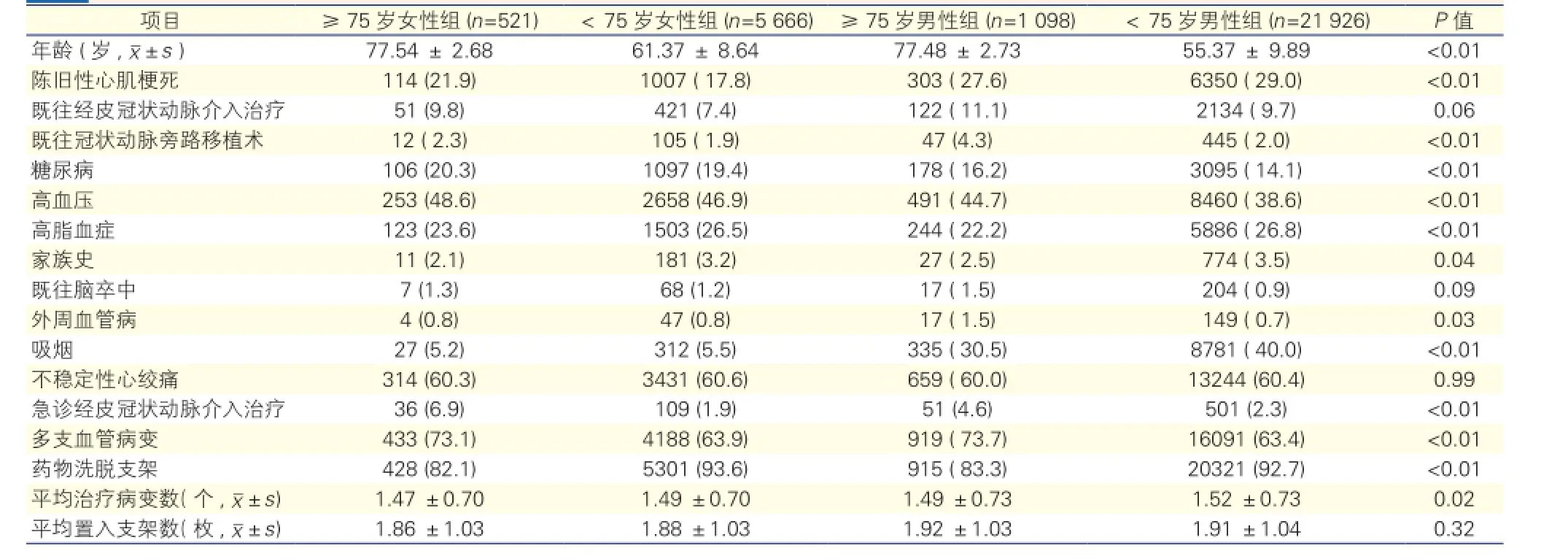
表1 4组患者基线资料比较[例(%)]
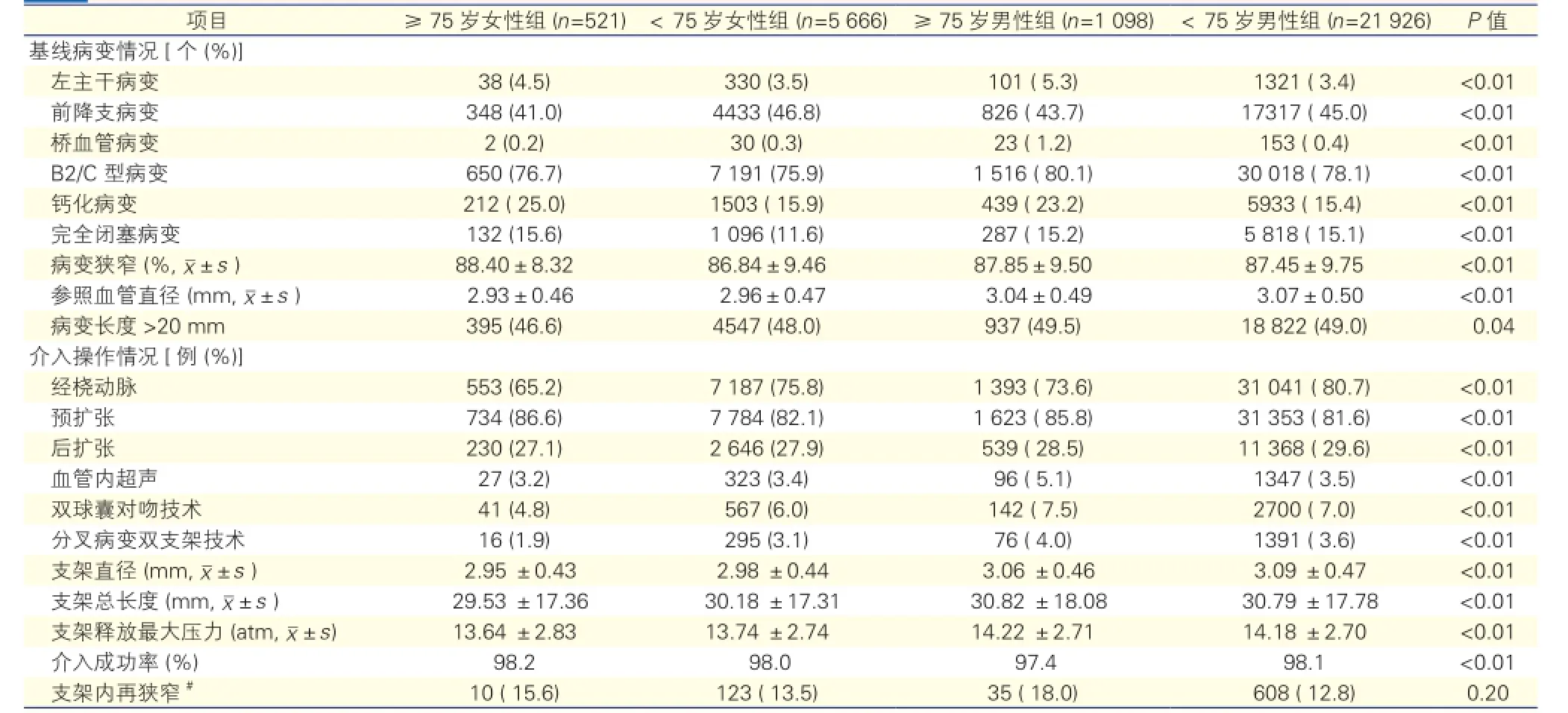
表2 4组患者基线病变特点和介入操作参数

表3 住院期间4组临床事件的发生情况[例(%)]
3 讨论
与男性冠心病患者相比,引起女性冠心病患者预后不良的危险因素更多,且这些危险因素随着年龄增长变得更加明显。与既往有关女性患者的报道一致[5-16],本研究中≥75岁女性组糖尿病、高血压的比例更高,一些研究显示糖尿病患者更易发生三支病变[18],高血压患者更易发生分叉病变[19],这些均可导致预后不良。此外,本研究中≥75岁女性组急诊PCI 、多支血管病变、钙化病变和完全闭塞病变的比例较高,参照血管直径较小,这些因素均可导致预后不良。
本研究中≥75岁女性组MACE发生率高于<75岁男性组和<75岁女性组,其中心原性死亡发生率明显高于其他三组,心肌梗死发生率高于<75岁男性组和<75岁女性组,TVR发生率与其他三组相比无明显差异。但调整混杂因素后,虽然≥75岁女性的心原性死亡和心肌梗死的发生风险仍明显高于<75岁男性和<75岁女性,却与≥75岁男性相比无明显差异。因此,≥75岁女性不是PCI术后预后不良的独立危险因素。
研究显示,女性患者预后不良只是暂时的,女性PCI术后30天内MACE的发生率比男性高,但1年时临床结局却与男性相当或优于男性[20-25]。而本研究中,老年女性不良事件的发生情况并未随时间推移而有所好转,长期随访及住院期的结局均较差。
本研究发现75岁及以上老年女性PCI术后住院期和长期结局较差,但75岁及以上老年女性不是预后不良的独立危险因素。由于本研究样本量大、随访时间长且来源于临床“真实世界”,也许能为临床选择治疗策略和预测此类患者预后提供一定的指导作用。本研究的不足之处在于为单中心、非随机对照研究,存在一定的选择偏倚和混杂性偏倚,需要开展进一步的研究来证实。另外,本研究失访率较高,且对失访中出现的34例原因不明的死亡事件未能进行进一步分析,这些因素可能对研究结果造成一定的影响。
[1] von Mering GO, Arant CB, Wessel TR, et al. Abnormal coronary vasomotion as a prognostic indicator of cardiovascular events in women: results from the national heart, lung, and blood institute-sponsored women’s ischemia syndrome evaluation (WISE). Circulation, 2004, 109: 722-725.
[2] Wong TY, Klein R, Sharrett AR, et al. Retinal arteriolar narrowing and risk of coronary heart disease in men and women. The atherosclerosis risk in communities study. J Am Med Assoc, 2002, 287: 1153-1159.
[3] Burke AP, Farb A, Malcom GT, et al. Effect of risk factors on the mechanism of acute thrombosis and sudden coronary death in women. Circulation, 1998, 97: 2110-2116.
[4] Burke AP, Virmani R, Galis Z, et al. 34th Bethesda conference: task force #2-what is the pathologic basis for new atherosclerosis imaging techniques? J Am Coll Cardiol, 2003, 41: 1874-1886.
[5] Cowley MJ, Mullin SM, Kelsey SF, et al. Sex differences in early and long term results of coronary angioplasty in the NHLBI PTCA Registry. Circulation, 1985, 71: 90-97.
[6] Peterson ED, Lansky AJ, Kramer J, et al. Effect of gender on the outcomes of contemporary percutaneous coronary intervention. Am J Cardiol, 2001, 88: 359-364.
[7] Bell MR, Holmes DR Jr, Berger PB, et al. The changing in-hospital mortality of women undergoing percutaneous transluminal coronary angioplasty. J Am Med Assoc, 1993, 269: 2091-2095.
[8] Ellis SG, Myler RK, King SB, et al. Causes and correlates of death after unsupported coronary angioplasty: Implications for use of angioplasty and advanced support techniques in high-risk settings. Am J Cardiol, 1991, 68: 1447-1451.
[9] Ellis SG, Roubin GS, King SB, et al. Angiographic and clinical predictors of acute closure after native vessel coronary angioplasty. Circulation, 1988, 77: 372-379.
[10] Lansky AJ, Ng VG, Mutlu H, et al. Gender-based evaluation of the XIENCE V everolimus-eluting coronary stent system: Clinical and angiographic results from the SPIRITⅢ randomized trial. Catheter Cardiovasc Interv, 2009, 74: 719-727.
[11] Watanabe CT, Maynard C, Ritchie JL. Comparison of short term outcomes following coronary artery stenting in men versus women. Am J Cardiol, 2001, 88: 848-852.
[12] Peterson ED, Dai D, DeLong ER, et al. Contemporary mortality risk prediction for percutaneous coronary intervention: Results from 588,398 procedures in the National Cardiovascular Data Registry. J Am Coll Cardiol, 2010, 55: 1923-1932.
[13] Singh M, Rihal CS, Gersh BJ, et al. Mortality differences between men and women after percutaneous coronary interventions . a 25-year, single-center experience. J Am Coll Cardiol, 2008, 51: 2313-2320.
[14] Woo JS, Kim W, Ha SJ, et al. Impactof gender differences on longterm outcomes after successful percutaneous coronary intervention in patients with acute myocardial infarction. Int J Cardiol, 2010, 145: 516-518.
[15] Berger JS, Sanborn TA, Sherman W, et al. Influence of sex on in-hospital outcomes and long-term survival after contemporary percutaneous coronary intervention. Am Heart J, 2006, 151: 1026-1031.
[16] Kovacic JC, Mehran R, Karajgikar R, et al. Female gender and mortality after percutaneous coronary intervention: results from a large registry. Catheter Cardiovasc Interv, 2012, 80: 514-521.
[17] Farooq V, Brugaletta S, Serruys PW. Contemporary and evolving risk scoring algorithms for percutaneous coronary intervention. Heart, 2011, 97: 1902-1913.
[18] 安辰鸿. 冠心病并发2型糖尿病患者冠状动脉病变特点及护理对策. 中国循环杂志, 2013, 29(z1): 233.
[19] 梅佳杰, 曲鹏. 合并高血压的冠心病患者冠状动脉病变特点的分析. 中国循环杂志, 2013, 29(z1): 128.
[20] Arnold AM, Mick MJ, Piedmonte MR, et al. Gender differences for coronary angioplasty. Am J Cardiol, 1994, 74: 18-21.
[21] Robertson T, Kennard ED, Mehta S, et al. Influence of gender on inhospital clinical and angiographic outcomes and on one year follow-up in the new approaches to coronary intervention(NACI) registry. Am J Cardiol, 1997, 80: 26K-39K.
[22] Mehilli J, Kastrati A, Bollwein H, et al. Gender and restenosis after coronary artery stenting. Eur Heart J, 2003, 24: 1523-1530.
[23] Heidland UE, Heintzen MP, Klimek WJ, et al. Acute complications and restenosis in women undergoing percutaneous transluminal coronary angioplasty. Is it possible to define sex differences and to determine risk factors? J Cardiovasc Risk, 1998, 5: 297-302.
[24] Kelsey SF, James M, Holubkov AL, et al. Results of percutaneous transluminal coronary angioplasty in women:1985-1986 national heart, lung, and blood institute’s coronary angioplasty registry. Circulation, 1993, 87: 720-727.
[25] Lansky AJ. Outcomes of percutaneous and surgical revascularization in women. Prog Cardiovasc Dis, 2004, 46: 305-319.
Gender Difference of Long-term Clinical Outcomes in Patients at 75 Years or Elder After Percutaneous Coronary Intervention Treatment
WANG Yu-jue, GAO Zhan, YANG Jin-gang, YUAN Jin-qing, XU Bo, YANG Yue-jin, CHEN Jue, CHEN Ji-lin, QIAO Shu-bin, WU Yong-jian, YAN Hong-bing, GAO Run-lin.
Department of Cardiology, Cardiovascular Institute and Fu Wai Hospital, CAMS and PUMC, Beijing (100037), China
Objective: To explore the gender differences of long term outcomes in patients at 75 years or elder after percutaneous coronary intervention (PCI) treatment.Methods: A total of 29211 consecutive patients who received PCI in our hospital from 2004-04 to 2010-11 were retrospectively studied. The patients were divided into 4 group: Group① Female ≥ 75 years of age, n=521, Group②Female < 7 5 years, n=5666 and Group③ Male ≥75 years, n=1098, Group④ Male < 75 years group, n= 21926. The inhospital and long-term clinical outcomes after PCI treatment were compared among different groups.Results: The in-hospital cardiac death in Group① was higher than the other 3 groups, P<0.05. Cox proportional hazard model analysis indicated that compared with Group② and Group④, the female ≥ 75 years was the independent risk factor for cardiac death (HR=2.53, 95% CI 1.15-5.59; HR=2.22, 95% CI 1.26-3.91) and cardiac death/MI (HR=2.26, 95% CI 1.27-4.03; HR=2.25, 95% CI 1.44-3.51). While compared with the male ≥75 years, the female ≥ 75 years was not an independent risk factor for cardiac death (HR=1.30) and cardiac death/MI (HR=1.21).Conclusion: Compared with other age groups, female patients at the age ≥ 75 years could have worse in-hospital and long-term outcomes after PCI, while it was not the independent risk factor for cardiac death and cardiac death/MI in patients after PCI treatment.
Percutaneous coronary intervention ; Elder female; Follow-up
2014-12-12)
(编辑:许 菁)
国家卫生和计划生育委员会公益性行业专项(201402001)
100037 北京市,北京协和医学院 中国医学科学院 国家心血管病中心 阜外心血管病医院 冠心病诊治中心
王玉珏 硕士研究生 研究方向:冠心病学研究 Email:805573802@qq.com 通讯作者:高展 Emai1:gaowangjia@163.com
R54
A
1000-3614(2015)05-0438-04
10.3969/j.issn.1000-3614.2015.05.007