椎间隙入路行病灶清除、植骨及内固定治疗腰骶椎结核的疗效探讨
2015-11-24邱南海王力苗瑞瑞薛海滨
邱南海,王力,苗瑞瑞,薛海滨
椎间隙入路行病灶清除、植骨及内固定治疗腰骶椎结核的疗效探讨
邱南海1,王力1,苗瑞瑞1,薛海滨2
目的探讨后路经椎间隙入路行病灶清除、植骨及椎弓根钉系统内固定治疗单节段及多节段腰骶椎结核的疗效。方法37例以单节段及多节段椎体破坏的腰骶椎结核患者均行后路经椎间隙病灶清除,椎弓根钉系统内固定,椎间隙内植骨治疗腰骶椎结核。术后行X线片、CT、MRI观察病灶愈合进程,下腰椎曲度,植骨融合情况和内固定稳定性情况。结果34例患者均一期愈合,其中4例术中神经根牵拉伤,术后3个月恢复尚好,症状消失。另3例患者伤口出现窦道,其中有2例经过调整抗结核药物治疗及换药后均愈合,1例出现窦道后调整抗结核药清创后二期愈合,术后X线、CT及MRI示植骨处骨性融合尚好,椎体高度恢复,无后凸畸形,无内固定松动、断钉等。结论后路椎间隙入路行病灶清除、植骨及内固定治疗单节段及多节段椎体破坏较轻,手术创伤小,植骨融合尚好,内固定牢固,治疗效果满意。
手术后并发症;椎间隙入路;腰骶椎结核;预后
脊柱结核是骨结核的好发部位,而腰骶椎结核更多见,由于腰骶部位解剖结构及生物力学的特殊性,前后路手术一直存在着争议[1-2]。有学者主张前入路,认为前入路视野好,病灶容易清除干净[3];有的学者主张前路和后路联合,先后路内固定达到有效稳定脊柱的效果后再行前路病灶清除[4]。本研究采取从后路椎间隙入路行病灶清除术治疗腰骶椎结核37例,效果较好,报告如下。
1 资料与方法
1.1 一般资料选取2008年10月—2013年12月于本院和中国人民解放军309医院骨科就诊的腰骶椎结核患者37
例,男28例,女9例,年龄22~68岁,平均(35±5)岁,病程4~12个月,平均(5±1)个月。临床表现为下腰痛,不同程度下肢疼痛,间歇性跛行,部分患者胫前肌力及趾背伸肌减弱,部分患者髋关节屈曲畸形。37例均行X线、CT及MRI检查示患者每个椎体间均少于1/2程度的破坏,下腰椎曲度变直,30例单椎体受累,7例为2个及多个椎体受累。所有患者腰大肌均无明显脓肿。
1.2 方法患者术前均给予三联或四联抗结核治疗2周左右,结核中毒症状减轻后,红细胞沉降率(血沉)明显好转,在患者能耐受手术情况下行手术准备。手术:患者在全身麻醉下取俯卧位,常规后侧入路显露病体及相邻椎体,正常椎体内植入椎弓根螺钉,如骶椎受累时,可植入髂骨钉加强固定,咬除病灶椎体椎板,将咬下的正常椎板的骨质咬碎以备植骨用,暴露硬脊膜,从破坏严重一侧入路暴露神经根,将神经根牵拉到一侧后,从椎体间隙进入清理坏死组织、死骨和破坏的椎间盘,尽可能刮到正常的骨组织渗血为止,最后用盐水反复冲洗椎间隙,并把备用碎骨块从间隙中植入,用凝胶海绵放置于间隙伤口,防止碎骨块突入椎管内,根据腰骶部曲度预弯连接棒,利用内固定器的加压作用恢复下腰椎曲度。多个椎体破坏用同样的方法,从两椎体间隙清除坏死组织,并植骨融合,置引流管接负压引流。
1.3 术后处理及疗效判断患者术后2~3d拔引流管,1周左右在支具保护下活动,带支具时间持续3~6个月,术后继续抗结核治疗9~18个月。术后1周行X线腰椎正侧位片,术后6个月CT、MRI观察病灶愈合进程,下腰椎曲度,植骨融合情况和内固定稳定性情况。
2 结果
2.1 术中及术后随访情况37例术后随访18~32个月,平均(24±3)个月。34例患者术后腰部疼痛消失,2~3个月植骨处骨性融合,椎体高度恢复,后凸畸形矫正良好,无内固定松动、断钉,椎体稳定性好;34例中有4例患者因手术操作时牵拉神经根造成术后下肢局部麻木,经过术后营养神经对症治疗,1~2个月症状逐渐消失。另外3例术后2个月左右切口处出现窦道形成,其中2例调整抗痨药物,原来口服利福平0.45g/次,1次/d,异烟肼0.3 g/次,1次/d,盐酸乙胺丁醇0.75 g/次,1次/d,口服利福平改为利福喷丁0.6 g/次,2次/周,其余2种口服药不变,1个月左右伤口全部愈合;1例术后2个月后伤口出现窦道,伤口内固定外露,并有少量分泌物,用药方式更改同前2例,并将伤口窦道进行清创并缝合,2周后拆线,伤口二期完全愈合。
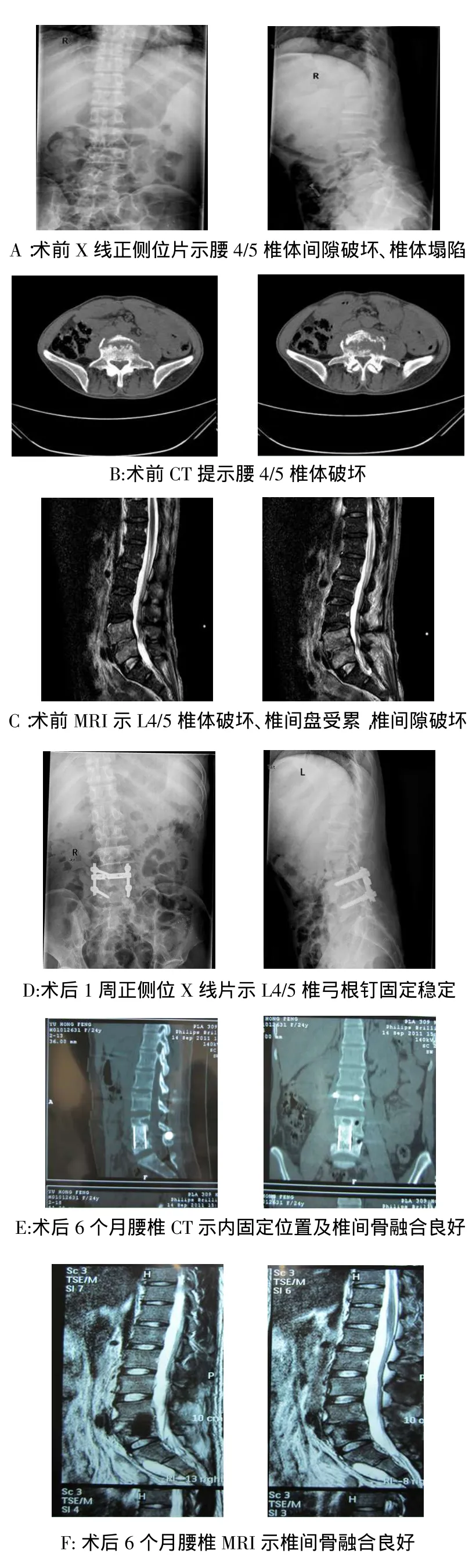
Fig.1Preoperative and postoperative X-ray,CT and MRI imaging of classic patient图1 典型患者术前与术后的X线片、CT及MRI影像
2.2 典型病例患者男,43岁,腰部疼痛6个月。见图1。入院查体:体温37.8℃,腰部有压痛叩击痛,腰部活动受限,直腿抬高试验和加强实验均呈阴性,感觉正常,无其他既往病史,诊断为腰4、5椎体结核,术前X线片示腰4/5间隙变窄,椎体塌陷;
CT示腰4/5椎体破坏,部分死骨形成;MRI示腰4/5椎体密度减低,椎体、间盘破坏。术后1周正侧位X线片示L4/5椎弓根钉固定稳定。术后6个月CT及MRI示腰4/5椎弓根钉固定稳定及骨融合尚好。
3 讨论
3.1 腰骶椎结核的术式选择腰骶椎结核手术治疗的目的为彻底清除病灶,解除神经压迫,重建脊柱的稳定性,尽早恢复脊柱功能[5-6]。目前,脊柱内固定的应用使脊柱结核的治疗有了很大进步,但具体手术方式仍存争议。前路手术优势在于直视下操作有利于病灶清除,同时进行植骨内固定,但该术式增加了血管、神经的损伤风险,技术操作难度大。前后联合入路术式采取从前路进行清除病灶、植骨,后路行内固定的术式增加了手术时间和患者的创伤风险[4,7]。本研究采用后路椎弓根单间隙内固定,经椎间隙入路病灶清除植骨术。相关研究认为,此术式对患者创伤小,可单节段及多节段固定脊柱,同时达到病灶清除、植骨的目的[3,8]。
3.2 本术式的优缺点本术式的优点为:(1)通过一个切口完成病灶清除植骨内固定,不需要再增加伤口,减少了患者再次创伤。(2)植骨块为小碎骨块,病椎间容易被小骨块填塞结实、无间隙,骨块小容易融合,可形成牢固病椎间的骨性融合,从而达到长期椎体稳定,并且骨块小融合时间短,新的毛细血管易生成,也易与椎体融合一体。术后笔者通常在植骨间隙处塞入一块泰陵包裹的明胶海绵以促其整合。有研究认为,此术式可以防止小骨块脱入椎管,也可以局部起到压迫止血效果[9]。本术式的缺点:(1)病变椎间隙视野显露较差,对技术要求高。(2)病灶清除时需牵拉神经,存在神经损伤风险。本组4例患者因牵拉神经根造成术后下肢局部麻木,经神经营养治疗后恢复。(3)病椎前方及腰大肌有大量脓性分泌物的患者不适合这种方法,病灶内不易彻底清干净,并且也容易造成伤口,形成窦道。
3.3 影像学评估综合本组经验,笔者认为:(1)术前需对患者进行影像学评估以判断是否适合采取本术式,本术式适用于以椎间盘和对应终板破坏为主、椎体破坏少的单节段及多节段腰骶椎结核者,若椎体前方缺损较大,并且有大量脓液的患者不适合本术式。(2)后路椎弓根植入病椎椎体时,若病椎破坏不超过50%,可以选择固定病椎[10]。(3)宜选择破坏较重一侧进入,有利于病灶清除干净,部分骶骨有破坏者可植入合适的髂骨钉以重建腰骶椎的稳定性。(4)少数患者因对抗结核药不敏感或产生耐药而使伤口形成窦道,经过调整抗结核治疗及对症处理等均能痊愈,考虑原因主要是患者内固定后及术中创伤小,有利于患者较快进行下地功能锻炼和康复,减少并发症的发生。
综上所述,单纯后路经椎间隙入路病灶清除植骨内固定对患者创伤较小,手术操作相对简单,如果适应证选择得当,可获得良好的治疗效果。
[1]Pappou IP,Papadopoulos EC,Swanson AN,et al.Pott disease in the thoracolumbar spine with marked kyphosis and progressive paraplegia necessitating posterior vertebral column resection and anterior reconstruction with a cage[J].Spine,2006,31(4):123-127.
[2]Ozdemir HM,Us AK,Oğün T.The role of anterior spinal instrumentation and allograft fibula for the treatment of pott disease[J].Spine,2003,28(5):474-479.
[3]Xiao LP,Jiang Y,Tian YG,et al.One stage debridement combined with bone graft fusion and internal fixation by anterior approach through abdomen for treating lumbosacral spinal tuberculosis[J]. China reconstruction surg,2009,23(8):913-916.[肖联平,江毅,田永刚,等.前路经腹腔一期病灶清除植骨融合内固定术治疗腰骶段脊柱结核[J].中国修复重建外科杂志,2009,23(8):913-916].
[4]Deng Q,Guo HL,Sheng WB,et al.Screw rod system internal fixation combined with focal debridement to treat elders’thoracolumbosacral vertebral tuberculosis[J].Chinese journal of tissue engineering,2013(13):2463-2470.[邓强,郭海龙,盛伟斌,等.钉棒系统置入内固定结合病灶清除治疗老年胸腰骶椎结核[J].中国组织工程杂志,2013,17(13):2463-2470].
[5]Jain AK,Jain S.Instrumented stabilization in spinal tuberculosis[J].Int Orthop,2012,36(2):285-292.doi:10.1007/s00264-011-1296-5.
[6]Yu M,Qiu NH.Posterior pedicle internal fixation system combined with iliac bone graft to repair segmental lumbosacral vertebral tuberculosis:reconstruction of the stability of the lumbosacral segment[J].Chinese journal of tissue engineering,2015,19(9):1377-1381.[余铭,邱南海.后路椎弓根系统内固定并髂骨植骨修复多节段腰骶椎结核:重建稳定的腰骶段[J].中国组织工程杂志,2015,19(9):1377-1381].
[7]Talu U,Gogus A,Ozturk C,et al.The role of posterior instrumentation and fusion after anterior radical debridement and fusion in the surgical treatment of spinal tuberculosis:experience of 127 cases[J].J Spinal Disord Tech,2006,19(8):554-559.
[8]Xiao R,Li TX,Luo WH,et al.Anterior approach lesion clearance and bone graft combined with posterior approach fixation in the treatment of lumbosacral vertebral tuberculosis[J].Journal of western medicine,2010,25(2):285-287.[肖睿,李同相,罗武华,等.前路病灶清除植骨和后路固定治疗腰骶椎结核[J].华西医学,2010,25(2):285-287].
[9]Kang J,Jia WD,Zhang YK,et al.Posterior bone graft combined with short segmental fixation and focus debridement in the treatment of spinal tuberculosis[J].Chinese journal of orthopaedic sur-
gery,2001,6:614-615.[康锦,贾卫斗,张英魁,等.后路植骨短节段内固定同期病灶清除治疗脊柱结核[J].中国矫形外科杂志,2001,6:614-615].
[10]Wang Q,Jin WD,Wang ZL,et al.Clinical research of stability reconstruction of intervertebral short pedicle screws fixation in the treatment of a single segment lumbosacral vertebral tuberculosis[J]. Journal of spine surgery,2015,13(1):1-6.[王骞,金卫东,王自立,等.患椎间短椎弓根螺钉在单节段腰骶椎结核稳定性重建中的临床研究[J].脊柱外科杂志,2015,13(1):1-6].
(2015-03-02收稿 2015-06-07修回)
(本文编辑 陆荣展)
Clinical pedicle internal fixation combined with debridement and bone graft through intervertebral approach as treatment of segmental lumbosacral vertebral tuberculosis
QIU Nanhai1,WANG Li1,MIAO Ruirui1,XUE Haibin2
1 Department of Orthopaedics,Tianjin Haihe Hospital,Tianjin 300350,China;2 Department of Orthopaedics,PLA NO.309 Hospital
ObjectiveTo discuss and observe the clinical effect of intervertebral pedicle internal fixation and debridement combined with bone graft through posterior approach/trans-intervertebral space approach on the treatment of uni/multisegmental lumbosacral vertebral tuberculosis(TB).MethodsA cohort of 37 patients,with single or multiple segmental vertebral destruction due to TB,were treated by trans-intervertebral debridement,posterior pedicle screw system internal fixation and intervertebral bone graft.All patients underwent X-ray,CT and MRI examination to observe the combination treatment effect.ResultsMost patients(n=34)enjoyed primary healing,in which include only 4 cases that presented symptom of nerve root stretch injury during operation but all recovered after 3 months.Other 3 patients underwent secondary healing due to sinus but two were rectifying with anti-TB therapy and wound dressing.The other 1 case suffered from sinus tract was healed through second debridement and rectifying therapy.X-ray,CT and MR at 6 months after operation indicated that all patients present great graft osseous fusion,good recovering of height of vertebral body without kyphosis deformity nor internal fixation loosening nor screw breakage.ConclusionIntervertebral pedicle internal fixation and debridement combined with bone graft through posterior approach/trans-intervertebral space approach is with minimum invasion but good graft fusion effects,harderfixationandsatisfactoryclinicaleffectsinthetreatmentofuni/multi-segmentallumbosacralvertebraltuberculosis.
postoperative complications;intervertebral space approach;lumbosacral tuberculosis;prognosis
R529.2;R681.53
A
10.11958/j.issn.0253-9896.2015.12.025
天津市卫生局局级课题(2014KZ037)
1天津市海河医院骨科(邮编300350);2中国人民解放军第309医院骨科
邱南海(1970),男,硕士研究生,副主任医师,主要从事骨科创伤及骨结核研究