中性粒细胞与淋巴细胞的比值在早期糖尿病肾病患者中的变化及意义
2015-08-22黄婉静刘清杏廖永康黄金华曾振华何志豪何雷
黄婉静,刘清杏,廖永康,黄金华,曾振华,何志豪,何雷
中性粒细胞与淋巴细胞的比值在早期糖尿病肾病患者中的变化及意义
黄婉静,刘清杏,廖永康,黄金华,曾振华,何志豪,何雷△
目的探讨中性粒细胞与淋巴细胞的比值(NLR)在早期糖尿病肾病(DN)患者中的变化及意义。方法选取91例确诊为早期DN的患者为DN组,54例正常健康人为对照组,比较2组的中性粒细胞、淋巴细胞、NLR及生化指标水平,采用Logistic回归分析早期DN的影响因素。结果DN组的肌酐(Cr)、总胆固醇(TC)、三酰甘油(TG)、低密度脂蛋白胆固醇(LDL-C)、中性粒细胞、C反应蛋白(CRP)高于对照组,淋巴细胞数低于对照组(均P<0.05);DN组的NLR水平高于对照组(2.52±0.57 vs 1.82±0.60,t=6.997,P<0.01)。Logistic回归分析表明,NLR、TG、TC升高均是DN的危险因素。结论NLR升高是早期DN的高危因素,可预测早期DN的发生。
糖尿病肾病;炎症;糖尿病,2型;中性粒细胞与淋巴细胞的比值
2型糖尿病绝大多数起病隐匿,常引发炎症反应并导致微血管病变,心血管、肾脏为主要受累的靶器官,糖尿病肾病(DN)是糖尿病常见的严重慢性并发症之一,往往伴有炎细胞浸润,细胞因子和炎症介质水平上升[1]。DN早期(微量白蛋白尿期)肾脏的病理改变多数是可逆转的,如能早期诊断与治疗,可阻止病情向不可逆的终末期肾病发展。中性粒细胞与淋巴细胞的比值(NLR)是近来发现的、可较为稳定反映机体炎症状态的指标。目前国外已有大量研究表明NLR与肿瘤预后、冠心病和心脏功能衰竭(心衰)的发生等有密切联系。随着近年来对NLR认知的深入,NLR在糖尿病、代谢综合征等疾病中的作用也逐渐得到重视。Azab等[2]和Afsar等[3]分别于2012年、2014年研究发现NLR对DN有预测作用,而国内目前鲜见相关研究报道。本研究通过对比分析早期DN患者和正常人的NLR,旨在探究NLR在诊断早期DN中的意义。
1 对象与方法
1.1研究对象选取2013年1月—2014年1月在南方医科大学珠江医院和顺德明景糖尿病医院内分泌科收治的2型糖尿病合并早期DN患者91例(DN组),其中男43例,女48例;另选取54例年龄、性别构成、体质量都与DN组相匹配的正常人为对照组,其中男30例,女24例。采用Mo⁃gensen的DN分期方法诊断早期DN:6个月内连续查尿微量蛋白排泄率(UAER)2次以上,UAER增加,且尿微量白蛋白达20~200 μg/min或30~300 mg/24 h。排除标准:(1)有冠状动脉疾病。(2)心衰、心脏自律异常。(3)肾动脉狭窄、肾病综合征、肾炎。(4)甲状腺功能亢进、甲状腺功能减退。(5)肝功能不全。(6)尿路感染、尿路结石。(7)急性感染、创伤或手术后2周以内。(8)其他可能引起尿微量白蛋白增加的原因和泌尿系统感染、原发性高血压、心衰、酮症酸中毒等。
1.2方法收集静脉血10 mL,用日本Sysmex公司生产的XE-5000全自动血液分析仪测定白细胞(WBC)总数和分类数;肌酐(Cr)、血尿酸(UA)、总胆固醇(TC)和三酰甘油(TG)均用酶法测定;高密度脂蛋白胆固醇(HDL-C)和低密度脂蛋白胆固醇(LDL-C)均用一步清除法测定。UAER测定:所有受试者正常饮食,避免剧烈运动,留取24 h尿,记录尿量,西门子BN-prospec全自动特定蛋白分析仪(免疫散射比浊法)测尿白蛋白,计算UAER,测定2次并取平均值。
1.3统计学方法数据用SPSS 20.0统计软件处理完成。资料以均数±标准差(±s)表示,计量资料比较采用t检验,计数资料比较采用χ2检验,糖尿病肾病影响因素分析采用二分类Logistic回归。以P<0.05为差异有统计学意义。
2 结果
2.1一般临床资料及生化指标比较2组间年龄、性别、BMI、UA、HDL-C比较差异无统计学意义,DN组的Cr、TG、TC和LDL-C水平高于对照组(P<0.05),见表1。
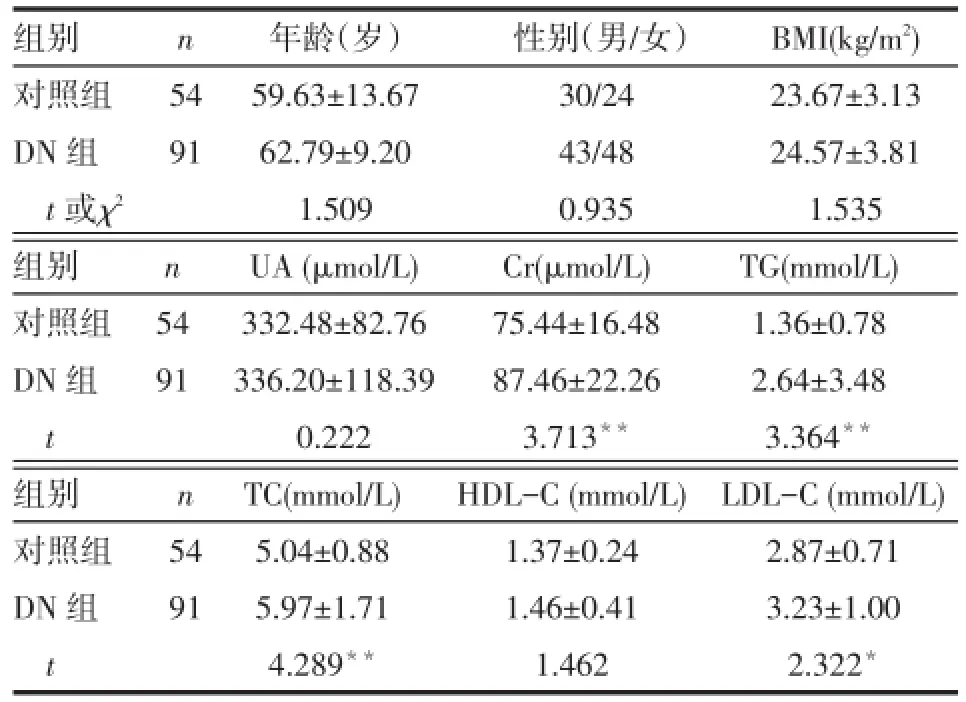
Tab.1 Comparison of clinical data between two groups表1 2组一般临床资料及生化指标比较
2.22组外周血细胞指数比较与对照组相比,DN组的中性粒细胞、C反应蛋白(CRP)和NLR水平增高,淋巴细胞数降低(P<0.05)。2组间WBC总数、血小板和单核细胞数比较差异无统计学意义,见表2。
Tab.2 Comparison of blood index between two groups表2 2组外周血细胞指数比较 (±s)
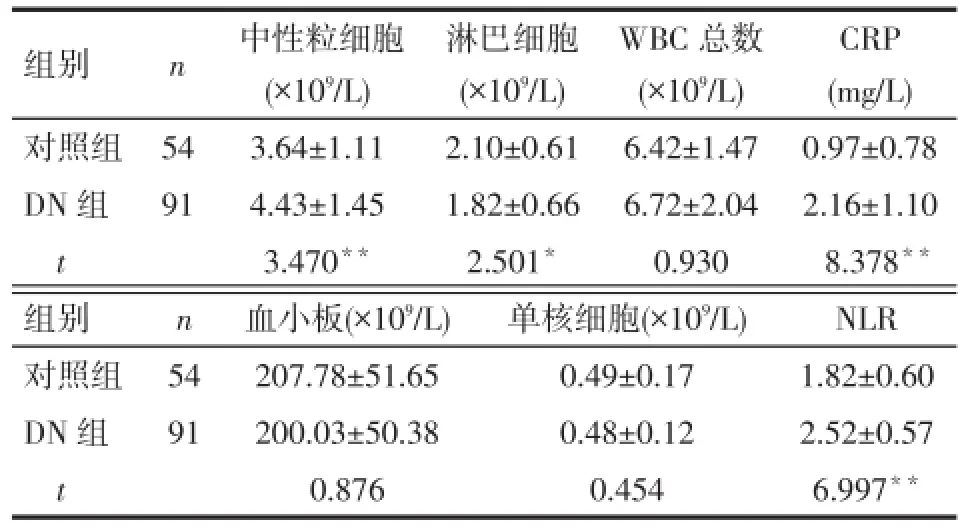
Tab.2 Comparison of blood index between two groups表2 2组外周血细胞指数比较 (±s)
*P<0.05,**P<0.01
组别对照组DN组t n 54 91中性粒细胞(×109/L)3.64±1.11 4.43±1.45 3.470**淋巴细胞(×109/L)2.10±0.61 1.82±0.66 2.501*WBC总数(×109/L)6.42±1.47 6.72±2.04 0.930 CRP (mg/L)0.97±0.78 2.16±1.10 8.378**组别对照组DN组t n 54 91血小板(×109/L)207.78±51.65 200.03±50.38 0.876单核细胞(×109/L)0.49±0.17 0.48±0.12 0.454 NLR 1.82±0.60 2.52±0.57 6.997**
2.3糖尿病肾病影响因素分析以有无DN为因变量(有=1,无=0),年龄、Cr、TC、NLR等因素为自变量行二分类logistic回归分析表明:TG、TC、NLR升高为DN的危险因素,见表3。
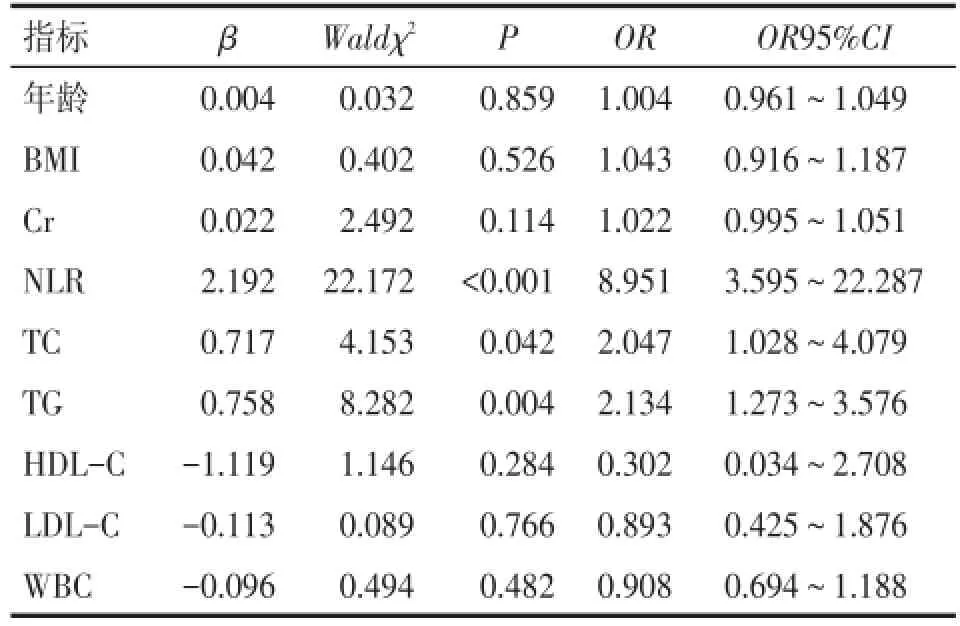
Tab.3 Result of logistic regression analysis on influence factors of diabetic nephropathy表3 糖尿病肾病影响因素的Logistic回归分析结果
3 讨论
DN是糖尿病严重的微血管并发症之一,与血管内皮细胞活性改变以及白细胞黏附浸润和激活[4]、生化代谢紊乱、氧化应激、细胞因子表达异常等多种因素有关。炎症反应是DN发生发展的重要环节,炎症常损伤微血管,引起肾小球病变、视网膜病变[5]、神经病变[6]等。DN患者血管内白细胞黏附增多[7],产生大量的过氧化物以及蛋白水解酶[8],导致肾脏内皮细胞功能障碍、灌注异常和血管通透性改变,影响肾小球的滤过功能。有研究表明抗炎治疗能减慢进展性肾病的发展[9]。另有研究表明外周血WBC总数和分类数与DN相关,但机制尚不明了[10]。中性粒细胞是炎症反应中重要的炎性细胞,具有趋化、黏附、吞噬和杀菌等作用,DN患者的中性粒细胞被激活,分泌抗凋亡蛋白A1、Bcl-xl增多,中性粒细胞凋亡延迟,使得血液中中性粒细胞增多。DN患者也存在淋巴细胞改变,文献报道,2型糖尿病患者淋巴细胞总数降低且T淋巴细胞亚群比例严重失调,CD4/ CD8比值明显下降,提示糖尿病患者存在淋巴细胞免疫功能紊乱[11]。
NLR是近来发现的反映机体炎症状态的炎症指标,不仅较中性粒细胞能更稳定地反映机体炎症状态,而且对多种疾病都有其独特的预测作用。研究发现升高的NLR是反映肝癌、胃癌、肾细胞癌和鼻咽癌患者预后的重要指标[12-15]。明显升高的NLR也是冠心病患者死亡的独立危险因素[16]。本研究发现:与对照组相比,DN组外周血的NLR、中性粒细胞、CRP水平增高,淋巴细胞总数降低。NLR是DN的独立危险因素:NLR每升高1个单位,患DN的风险就升高8.951倍。提示NLR对于DN的发生、发展具有重要指导作用。
目前早期DN的诊断主要依靠尿液中尿微量白蛋白含量,但英国有研究表明单纯用尿微量白蛋白作为诊断标准不能早期有效地发现早期DN[17]。张耀平等[18]研究表明肾小球滤过率(GFR)是早期DN敏感的监测指标,且比UAER更具实用性和科学性。但GFR又有其变化相对缓慢的特点,用于疾病疗效的判定不够敏感。本研究发现DN患者中NLR显著增高,且NLR为DN的独立危险因素,如能把尿微量白蛋白、肾小球滤过率和NLR的变化结合起来综合考虑,可能有利于更好地筛查早期DN,争取早诊断早治疗,早期逆转肾小球损害,延缓DN的进展。
[1]Duran-Salgado MB,Rubio-Guerra AF.Diabetic nephropathy and inflammation[J].WorldJDiabetes,2014,5(3):393-398.doi: 10.4239/wjd.v5.i3.393.
[2]Azab B,Daoud J,Naeem FB,et al.Neutrophil-to-lymphocyte ratio as a predictor of worsening renal function in diabetic patients(3-year follow-up study).[J].Ren Fail,2012,34(5):571-576.doi: 10.3109/0886022X.2012.668741.
[3]Afsar B.The relationship between neutrophil lymphocyte ratio with urinary protein and albumin excretion in newly diagnosed patients with type 2 diabetes[J].Am J Med Sci,2014,347(3):217-220.doi: 10.1097/MAJ.0b013e31828365cc.
[4]An Y,Li JF,Wu F,et al.Correlation between renal artery resistive index and vascular endothelial growth factor in patients with early diabetes nephropathy[J].Journal of Chinese Practical Diagnosis and Therapy,2014(7):51-53.[安勇,李建锋,吴芳,等.早期糖尿病肾病患者肾动脉血流阻力指数与血管内皮生长因子相关性分析[J].中华实用诊断与治疗杂志,2014(7):51-53].
[5]Ulu SM,Dogan M,Ahsen A,et al.Neutrophil-to-lymphocyte ratio as a quick and reliable predictive marker to diagnose the severity of diabetic retinopathy[J].Diabetes Technol Ther,2013,15(11):942-947.doi:10.1089/dia.2013.0097.
[6]Liu X.Advances on the mechanism of diabetic neuropathy[J].For⁃eign Medical Sciences(Section On Neurology&Neurosurgery,2001,28(3):201-204.[刘欣.糖尿病神经病变发生机制研究的若干进展[J].国外医学·神经病学神经外科学分册,2001,28(3):201-204].
[7]Kamiuchi K,Hasegawa G,Obayashi H,et al.Leukocyte-endotheli⁃al cell adhesion molecule 1(LECAM-1)polymorphism is associat⁃ed with diabetic nephropathy in type 2 diabetes mellitus[J].J Diabe⁃tes Complications,2002,16(5):333-337.
[8]Navarro-Gonzalez JF,Mora-Fernandez C,Muros DFM,et al.In⁃flammatory molecules and pathways in the pathogenesis of diabetic nephropathy[J].Nat Rev Nephrol,2011,7(6):327-340.doi:10.1038/ nrneph.2011.51.
[9]Marion RW.Genetic drift.Erin,before I knew her[J].Am J Med Genet,2000,90(2):95-97.
[10]Vozarova B,Weyer C,Lindsay R S,et al.High white blood cell count is associated with a worsening of insulin sensitivity and pre⁃dicts the development of type 2 diabetes[J].Diabetes,2002,51(2): 455-461.
[11]Navarro JF,Mora C,Maca M,et al.Inflammatory parameters are in⁃dependently associated with urinary albumin in type 2 diabetes mel⁃litus[J].Am J Kidney Dis,2003,42(1):53-61.
[12]An X,Ding PR,Wang FH,et al.Elevated neutrophil to lymphocyte ratio predicts poor prognosis in nasopharyngeal carcinoma[J].Tumour Biol,2011,32(2):317-324.doi:10.1007/s13277-010-0124-7.
[13]Shimada H,Takiguchi N,Kainuma O,et al.High preoperative neu⁃trophil-lymphocyte ratio predicts poor survival in patients with gas⁃tric cancer[J].Gastric Cancer,2010,13(3):170-176.doi:10.1007/ s10120-010-0554-3.
[14]Halazun KJ,Hardy MA,Rana AA,et al.Negative impact of neutro⁃phil-lymphocyte ratio on outcome after liver transplantation for he⁃patocellular carcinoma[J].Ann Surg,2009,250(1):141-151.doi: 10.1097/SLA.0b013e3181a77e59.
[15]Ohno Y,Nakashima J,Ohori M,et al.Pretreatment neutrophil-tolymphocyte ratio as an independent predictor of recurrence in pa⁃tients with nonmetastatic renal cell carcinoma[J].J Urol,2010,184 (3):873-878.doi:10.1007/s13277-010-0124-7.
[16]Tamhane UU,Aneja S,Montgomery D,et al.Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome[J].Am J Cardiol,2008,102(6):653-657.doi:10.1016/j.amjcard.2008.05.006.
[17]New JP,Middleton RJ,Klebe B,et al.Assessing the prevalence,monitoring and management of chronic kidney disease in patients with diabetes compared with those without diabetes in general prac⁃tice[J].Diabet Med,2007,24(4):364-369.
[18]Zhang YP,Significance of urinary albumin excretion rate and glo⁃merularfiltration rate for diagnosis of early diabetic nephropathy[J]. Journal of Qiqihar Medical College,2006,27(11):1294-1295.[张耀平.尿白蛋白排泄率和肾小球滤过率在早期糖尿病肾病的诊断价值[J].齐齐哈尔医学院学报,2006,27(11):1294-1295].
(2014-07-03收稿2014-10-10修回)
(本文编辑闫娟)
Clinic significance of neutrophil-iymphocyte ratio in the early-stage diabetic nephropathy
HUANG Wanjing,LIU Qingxing,LIAO Yongkang,HUANG Jinhua,ZENG Zhenhua,HE Zhihao,HE Lei△
Department of Endocrinology,Zhujiang Hospital,Southern Medical University,Guangzhou,510282,China
△Corresponding Author E-mail:765139701@qq.com
ObjectiveTo investigate neutrophil lymphocyte ratio(NLR)in early-stage diabetic nephropathy and its clinic significance.MethodsThe 145 subjects were divided into two groups:the healthy control group(n=54)and early stage diabetic nephropathy group(n=91).The numbers of neutrophils(N)and lymphocytes(L)as well as the NLR values of peripheral blood and other biochemistry index were examined.Factors of early stage diabetic nephropathy were calculated us⁃ing variance and logistic regression analysis.ResultsCreatinine(Cr),total cholesterol(TC),triglyceride(TG),LDL-C,neu⁃trophils number and CRP in DN group were significantly higher than those of the control group and lymphocytes numbers of DN group were significantly lower than that of the control group(P<0.05 respectively);NLR values were significantly higher in diabetic nephropathy group compared with those of healthy control group(2.52±0.57 vs 1.82±0.60,t=6.997,P<0.01).Lo⁃gistic regression analysis showed that the risk factors of DN include NLR,TG and total cholesterol.NLR(P<0.001,OR= 8.951,OR 95%CI:3.595-22.287)was significantly associated with DN.ConclusionHigh NLR values may be a predic⁃tive and reliable marker ofearly-stage DN.
diabetic nephropathies;inflammation;diabetes mellitus,type 2;neutrophil-lymphocyte ratio
R587.1
ADOI:10.11958/j.issn.0253-9896.2015.02.027
广东省医学科研基金(B2013253)
广州,南方医科大学珠江医院内分泌科(邮编510282)
黄婉静(1992),女,本科双语班在读
△E-mail:765139701@qq.com
