Effect of acupuncture combined with rehabilitation training on walking function after arthroscopic meniscus repair
2015-06-19LiuXinrong刘新荣LiQi李旗
Liu Xin-rong (刘新荣), Li Qi (李旗)
1 Rehabilitation Department, the 2nd Hospital Affiliated to Luohe Medical College, Henan 462000, China
2 College of Traditional Chinese Medicine, Hebei United University, Hebei 063000, China
Effect of acupuncture combined with rehabilitation training on walking function after arthroscopic meniscus repair
Liu Xin-rong (刘新荣)1, Li Qi (李旗)2
1 Rehabilitation Department, the 2nd Hospital Affiliated to Luohe Medical College, Henan 462000, China
2 College of Traditional Chinese Medicine, Hebei United University, Hebei 063000, China
Objective:To observe the effect of acupuncture combined with rehabilitation training on walking function after arthroscopic meniscus repair.
Methods:A total of 60 cases after arthroscopic meniscus repair were randomly allocated into an observation group and a control group, 30 in each group. Cases in the observation group received acupuncture combined with standard rehabilitation training, whereas cases in the control group only received the standard rehabilitation training. The energy, support torque and swing torque of the knee joints in the two groups were measured and compared before treatment, after 1-month and 2-month treatments.
Results:Before treatment, there were no between-group significant differences in the differences of energy, support torque and swing torque of the knee joints (P>0.05). After 1-month and 2-month treatments, there were intra-group and inter-group statistical differences in these parameters (P<0.05).
Conclusion:Acupuncture combined with rehabilitation training can increase the energy, support torque and swing torque of the knee joints of patients after arthroscopic meniscus repair and improve their walking function.
Acupuncture Therapy; Meniscus, Tibia; Gait; Rehabilitation; Arthroscopy; Randomized Controlled Trial
Meniscus tear is a common sports injury and mainly characterized by localized knee joint pain. Some patients may experience leg weakness or knee joint locking and atrophy of quadriceps femoris. Over the recent years, minimally invasive arthroscopy has been widely used in meniscus tear. Today it is attracting more and more attention because of its good effect[1-3]. In this study, we observed the effect of acupuncture combined with rehabilitation training on walking function after arthroscopic meniscus repair. The results are now summarized as follows.
1 Clinical Data
1.1 Diagnostic criteria
This was based on the Criteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine issued by the State Administration of Traditional Chinese Medicine[4]: a history of traumatic injury, alternatively no history of obvious traumatic injury; knee joint pain and swelling following injury, coupled with clicking sounds and joint locking; tenderness on medical and lateral knee joint space; chronic atrophy of quadriceps femoris, especially on the medial side of the muscle; positive signs of McMurray test and patellar grind test; and meniscus tear confirmed by MRI exmination.
1.2 Inclusion criteria
Those who met the above diagnostic criteria; aged between 35 and 70 years; and without gender limitation.
1.3 Exclusion criteria
Those who failed to meet the above diagnostic and inclusion criteria; having injury or fracture of cruciate and collateral ligaments; having complications of major primary medical conditions involving the liver, kidney, hemopoietic or endocrine systems; having mental disorders; and those who failed to cooperate or stick to the treatment protocol.
1.4 Statistical analysis
1.5 General materials
A total of 60 outpatients and inpatients after arthroscopic meniscus repair treated at the Rehabilitation Department of our hospital between January 2012 and December 2013 were randomly allocated into two groups, 30 in each group. There were no between-group statistical differences in age, gender and duration, indicating that the two groups were comparable (Table 1).
2 Treatment Methods
2.1 Observation group
2.1.1 Acupuncture
Points: Dubi (ST 35), Xuehai (SP 10), Liangqiu (ST 34), Zusanli (ST 36) and Xitong (Extra) [locates at 1 cun lateral to Quchi (LI 11)].
Method: After routine sterilization, Dubi (ST 35), Xuehai (SP 10), Liangqiu (ST 34) and Zusanli (ST 36) were first punctured with filiform needles of 0.38 mm in diameter and 65 mm in length. The needles were retained for 30 min upon needling sensation. After the needles were removed, Xitong (Extra) point was punctured perpendicularly with filiform needles of 0.38 mm in diameter and 75 mm in length. The optimal result can be achieved if the local soreness, distension and heaviness sensation radiates down to the buttocks. The treatment was done once a day for 2 months.
2.1.2 Rehabilitation training
Patients were asked to conduct conventional rehabilitation exercise including passive joint motion, knee joint control, stance balance and gait training. The 30-minute exercise was done once a day for 2 months.
2.2 Control group

Table 1. Between-group comparison of general materials
3 Results Observation
3.1 Measurement parameters
The energy, support torque and swing torque of the knee joints were measured using the Lokomat gait assessment system before treatment, after 1-month treatment and after 2-month treatment[5].
3.2 Results
3.2.1 Comparison of knee joint energy
Before treatment, there were no between-group significant differences in knee joint energy (P>0.05). After 1-month and 2-month of treatment, there were intra-group significant differences in both groups in knee joint energy (P<0.05); and there were intra-group significant differences between 1-month treatment and 2-month treatment in both groups (P<0.05). In addition, there were inter-group significant differences after 1-month and 2-month of treatment (P<0.05, P<0.01). This indicates that the knee joint energy was improved in both groups after treatment and the improvement was more significant in the observation group than that in the control group (Table 2).
Table 2. Between-group comparison of knee joint energy
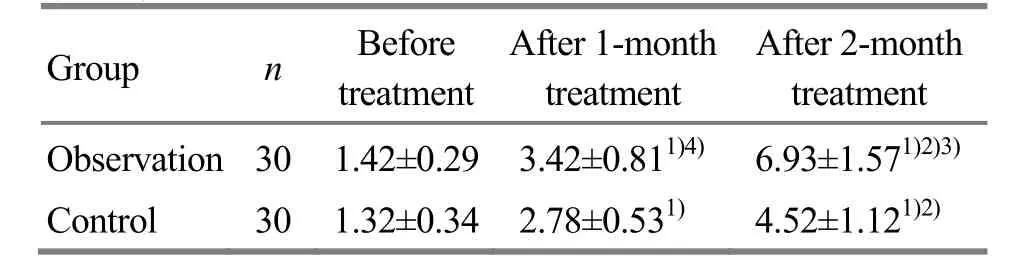
Table 2. Between-group comparison of knee joint energy
Note: Intra-group comparison before and after treatment, 1) P<0.05; intra-group comparison before and after 1-month treatment, 2) P<0.05; inter-group comparison in corresponding period, 3) P<0.01, 4) P<0.05
Group n Before treatment After 1-month treatment After 2-month treatment Observation 301.42±0.293.42±0.811)4)6.93±1.571)2)3)Control 301.32±0.342.78±0.531)4.52±1.121)2)
3.2.2 Comparison of knee joint support torque
Before treatment, there were no between-group significant differences in knee joint support torque (P>0.05). After 1-month and 2-month of treatment, there were intra-group significant differences in both groups in knee joint support torque (P<0.05); and there were intra-group significant differences between 1-month treatment and 2-month treatment in both groups (P<0.05). In addition, there were inter-group significant differences after 1-month and 2-month of treatment (P<0.05, P<0.01). This indicates that the knee joint support torque was improved in both groups after treatment and the improvement was more significant in the observation group than that in the control group (Table 3).
Table 3. Between-group comparison of knee joint support

Table 3. Between-group comparison of knee joint support
Note: Intra-group comparison before and after treatment, 1) P<0.05; intra-group comparison before and after 1-month treatment, 2) P<0.05; inter-group comparison in corresponding period, 3) P<0.01, 4) P<0.05
Group n Before treatment After 1-month treatment After 2-month treatment Observation 30 53±16 171±391)4)274±771)2)3)Control 30 50±17 143±411)211±641)2)
3.2.3 Comparison of knee joint swing torque
Before treatment, there were no between-group significant differences in knee joint swing torque (P>0.05). After 1-month and 2-month of treatment, there were intra-group significant differences in both groups in knee joint swing torque (P<0.05); and there were intra-group significant differences between 1-month treatment and 2-month treatment in both groups (P<0.05). In addition, there were inter-group significant differences after 1-month and 2-month of treatment (P<0.01). This indicates that the knee joint swing torque was improved in both groups after treatment and the improvement was more significant in the observation group than that in the control group (Table 4).
Table 4. Between-group comparison of knee joint swing

Table 4. Between-group comparison of knee joint swing
Note: Intra-group comparison before and after treatment, 1) P<0.05; intra-group comparison before and after 1-month treatment, 2) P<0.05; inter-group comparison in corresponding period, 3) P<0.01
Group n Before treatment After 1-month treatment After 2-month treatment Observation 30 -138±57 11±91)3)72±281)2)3)Control 30 -124±43 -41±51)34±141)2)
4 Discussion
The meniscus is a key component of the knee joint and acts to stabilize and lubricate the joint as well as reduce friction. Meniscus injury can directly affect the motor function of the knee joint[6-7]. Despite the good effect of meniscus arthroscopy, loss of certain motor functions of the knee joint may greatly affect the patients’ daily living and work. As a result, rehabilitation following meniscus arthroscopy has attracted more and more attention. Today, traditional therapy combined with modern rehabilitation training has achieved satisfactory effects in this regard[8-11].
In this study, we’ve observed the effect of acupuncture combined with rehabilitation training on abnormal gait following meniscus arthroscopy. Needling Dubi (ST 35) can remove wind, resolve dampness, dissipate cold and alleviate pain. Needling Xuehai (SP 10) can unblock meridians, resolve stasis and relieve pain. Needling Liangqiu (ST 34) can harmonize stomach qi and dredge meridians and collaterals. Needling Zusanli (ST 36) can regulate the spleen and stomach and supplement spleen qi. Needling the extra Xitong point can relax tendons. The above points combined can supplement qi and blood, remove wind and stop pain.
The study findings have shown that the parameters of the knee joint energy, support torque and swing torque in the observation group were better than that in the control group. This indicates that, compared with rehabilitation training alone, acupuncture combined with rehabilitation training can better improve the patients’ knee joint support and swing torques after meniscus arthroscopy, correct their abnormal gaits, increase their motor function of the lower limb and benefit the balance abilities of their lower limbs during walking.
Conflict of Interest
The authors declared that there was no conflict of interest in this article.
Acknowledgments
This work was supported by Scientific Research Project of Hebei Provincial Administration Bureau of Traditional Chinese Medicine (河北省中医药管理局科研计划项目, No. 2014188).
Statement of Informed Consent
Informed consent was obtained from all individual participants included in this study.
Received: 25 September 2014/Accepted: 28 October 2014
[1] Ge M, Zhu ZJ. Rehabilitation and care of 86 meniscus injury with knee arthroscopy. Med J of Communications, 2012, 26 (6): 657-658.
[2] Zhang HJ, Sun HM, Chai HY. Rehabilitation care for perioperative meniscus injury using knee arthroscopy. Zhongguo Shequ Yishi, 2012, 14(10): 345.
[3] Wang YS, Dong XY, Li N. Prevention and rehabilitation instructions for postoperative complications of meniscus injury under arthroscopy. Zhongguo Shiyong Yiyao, 2012, 7 (11): 233-234.
[4] State Administration of Traditional Chinese Medicine. Criteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine. Nanjing: Nanjing University Press, 1994: 205.
[5] Hao ZW, Li JM, Zhao YN, Shen HT. The effects of Lokomat lower gait training rehabilitation robot on lower limb function in hemiplegic stroke patients. Xiandai Yufang Yixue, 2013, 40(8): 1558-1559.
[6] Guo SM, Li JM, Wu QW, Shen HT. Clinical application of Lokomat automatic robot gait training and assessment system. Zhongguo Yiliao Shebei, 2011, 26 (3): 94-96.
[7] Hu W, Li P, Li PD, Wang D, Yu R, Cheng XH. Effect of early rehabilitation treatment with strengthened balance training on the function of patients with meniscus injury. Hainan Med J, 2014, 25(2): 186-188.
[8] Shao ZH, Zhang YF, Lü H, Bi X, Gao LL, Liu XL, Huang XN. The impact of knee functions and muscles strength of isokinetic for patients with knee meniscus after arthroscopic surgery. Zhongguo Yiyao Xuekan, 2014, 16(4): 612-613.
[9] He LQ, Wang Y. Rehabilitation training and Chinese traditional medicine improves the knee function of athletes after surgical treatment of meniscus injury. Chin J Sports Med, 2013, 32(9): 784-787.
[10] Xiao B, Pang J. Kinesio taping technique for meniscus injury of athlete’s efficacy of early postoperative rehabilitation. Nanjing Tiyu Xueyuan Xuebao: Ziran Kexue Ban, 2013, 12(4): 34-35.
[11] Guo J, Liu XY, Wang JY. Effective analysis of segmented rehabilitation nursing on treating meniscus injury. Sichuan Zhongyi, 2013, 31 (8): 161-162.
Translator:Han Chou-ping (韩丑萍)
针刺配合康复训练对膝关节半月板损伤术后步行功能的影响
目的:观察针刺配合康复训练对膝关节半月板损伤关节镜术后患者步行功能的影响。方法:将 60 例半月板损伤关节镜术后患者按随机数字表法分为两组,每组30 例。观察组予针刺结合常规康复训练治疗,对照组仅采用与观察组相同的常规康复训练治疗。于治疗前及治疗1个月、2个月后对患者膝关节能量、支撑力矩及摆动力矩进行测量比较。结果:治疗前,两组膝关节能量、支撑力矩及摆动力矩差异均无统计意义(P>0.05)。治疗 1个月及2个月后,两组患者膝关节能量、支撑力矩及摆动力矩均明显改善,与本组治疗前有统计学差异
(P<0.05);两组间亦有统计学差异(P<0.05)。结论:针刺配合康复训练可增加膝关节半月板损伤关节镜术后患者下肢运动过程中膝关节能量、支撑力矩与摆动力矩,提高其步行功能。
针刺疗法; 半月板, 胫骨; 步态; 康复; 关节镜检查; 随机对照试验
R246.2 【
】A
the control group only
the same rehabilitation training (same method and time) as the observation group.
Author: Liu Xin-rong, attending physician.
E-mail: tsslw110@126.com
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Professor Tian Cong-huo’s commonly used acupuncture methods and their clinical application
- Electroacupuncture combined with iontophoresis of Chinese medicine for lumbar intervertebral disc herniation
- Effect of row needling in muscle regions combined with seven-star needle tapping on cognitive function and quality of life in patients with post-stroke upper limb spasticity
- Effect of ginger-partitioned moxibustion on immunocytokines in patients with chronic nonbacterial prostatitis
- Triple needling plus moxibustion and Tanbo-plucking tender points for the third lumbar vertebra transverse process syndrome
- Summary of Professor Jin Yi-cheng’s academic thoughts on pediatric tuina therapy