急性心肌梗死急诊PCI再灌注后适应疗法疗效研究
2015-05-30睢勇李润堂
睢勇 李润堂

[摘要] 目的 探討缺血后适应疗法对急性ST段抬高心肌梗死细胞因子的影响和心肌细胞的保护作用。 方法 选择2011年7月~2012年10月首次发生急性ST段抬高心肌梗死病例45例,随机分为缺血/再灌注后适应组(25例)和对照组(20例)。缺血/再灌注后适应组在梗死相关血管获得再灌注后,分别以PTCA球囊阻断前向血流使再灌注时间分别达到60、120、180 s后,再恢复持续灌注并完成支架术;对照组常规完成支架植入术。测定并比较两组术前术后丙二醛(MDA)、超氧化物歧化酶(SOD)、肿瘤坏死因子-α(TNF-α)和白介素-6(IL-6)。 结果 缺血后适应组CK峰值较对照组明显更低(P<0.05);术后两组MDA、TNF-α、IL-6较术前显著升高(P<0.05),SOD较术前显著降低(P<0.05);术后适应组MDA、TNF-α、IL-6低于对照组(P<0.05);SOD高于对照组(P<0.05)。 结论 缺血/再灌注后适应疗法能够抑制心肌缺血/再灌注所引起的SOD水平下降,抑制MDA、TNF-α、IL-6水平升高,可以减轻急性心肌梗死急诊PCI再灌注后的再灌注损伤。
[关键词] 缺血/再灌注后适应;再灌注损伤;心肌梗死;急诊经皮冠状动脉介入
[中图分类号] R542.22 [文献标识码] B [文章编号] 1673-9701(2015)30-0074-04
Research on the efficacy of adaptation therapy after emergency PCI reperfusion in treating acute myocardial infarction
SUI Yong1 LI Runtang2
1.Department of Cardiology, Liaocheng Traditional Chinese Medicine Hospital in Shandong Province, Liaocheng 252000, China; 2.Department of Cardiology, Manchuria Hospital in Inner Mongolia Autonomous Region, Manchuria 021400, China
[Abstract] Objective To investigate the effect of adaptation after ischemic on acute ST segment elevation myocardial infarction cytokines and the protective role of myocardial cells. Methods A total of 45 cases of patients with first occurrence of acute ST-segment elevation myocardial infarction from July 2011 to October 2012 were selected and randomly divided into the adaptation after ischemia/reperfusion group (with 25 cases) and the control group (with 20 cases). The adaption after ischemia/reperfusion group received reperfusion after infracting related artery, and the blood flow was blocked by PTCA balloon so that the reperfusion time reached 60, 120 and 180 seconds respectively. Continuous infusion recovered and stenting was completed. The control group completed routine stent implantation. Preoperative and postoperative malondialdehyde(MDA), superoxide dismutase(SOD), tumor necrosis factor-α(TNF-α) and interleukin-6(IL-6) were determined and compared. Results The adaptation after ischemic group had significantly lower CK peak than the control group(P<0.05). MDA, TNF-α, IL-6 in the two groups after operation were significantly higher than those before operation(P<0.05). SOD in the two groups after operation was significantly lower than that before operation(P<0.05). Compared with those in the control group, MDA, TNF-α, IL-6 in the adaptation after reperfusion group decreased significantly(P<0.05) and SOD in the adaptation after adaptation group was significantly higher(P<0.05). Conclusion The post-adaptation can inhibit the drop of SOD levels caused by myocardial ischemia/reperfusion, and inhibit the increase of MDA, TNF-α and IL-6 levels. Adaptation after ischemia/reperfusion can reduce reperfusion injury after emergency PCI reperfusion adaptation therapy in treating acute myocardial infarction.
[Key words] Adaptation after ischemia/reperfusion; Reperfusion injury; Myocardial infarction; Emergency percutaneous coronary intervention
急诊经皮冠状动脉介入治疗(percutaneous coronary intervention,PCI)在临床上已取得巨大成功,是急性ST段抬高心肌梗死的首选治疗方法。尽管如此,因再灌注损伤普遍存在,不同程度降低缺血心肌再灌注治疗的疗效。减少再灌注损伤必然会改善再灌注治疗效果,并有可能降低急性心肌梗死(acute myocardial infarction,AMI)的死亡率。缺血预适应(ischemic preconditioning,IP)的心肌保护机制可能是通过抑制氧化应激反应、保护内皮细胞功能、减少中心粒细胞聚集、抑制心肌细胞凋亡[1-7]。本研究通过观察急性心肌梗死急诊PCI时,当靶血管获得再灌注后通过球囊附加缺血后适应时所引起的CK峰值,通过研究SOD、MDA、TNF-α、IL-6的水平变化初步探索缺血后适应的心肌保护作用和机制。现报道如下。
1 资料与方法
1.1 一般资料
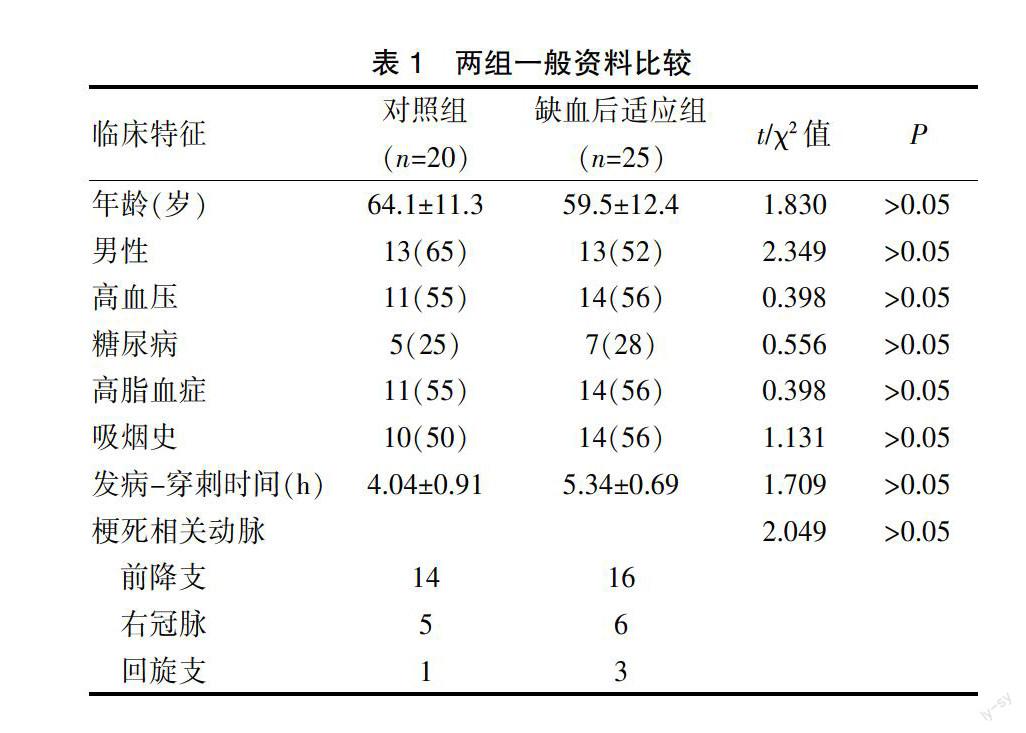
2011年7月~2012年10月,根据参考文献[8]连续入选急性ST段抬高心肌梗死(ST segment elevation myocardial infarction,STEMI)患者45例,其中男26例,女19例,年龄36~79岁,平均(61.5±12.0)岁。入选标准:符合急诊PCI适应证,并同意急诊PCI治疗。排除标准:①合并室间隔穿孔、乳头肌或二尖瓣腱索断裂、心脏破裂等机械并发症;②合并心源性休克;③梗死相关动脉血栓负荷过重;④梗死相关动脉为左主干病变或者为其他冠脉闭塞合并左主干严重狭窄;⑤梗死相关血管已自发再通的(TIMI血流≥2级);⑥梗死的相关动脉开通后发生慢血流或者无复流现象;⑦至梗死相关血管侧支开放充分(Rentrop分级[5,7]≥2级);⑧合并感染、结缔组织病、全身免疫性疾病、肝肾功能不全、恶性肿瘤等;⑨梗死前心绞痛。根据随机数字表将入选病例随机分为缺血后适应组(Post-con)和对照组(Control)。两组患者的一般资料及合并冠心病患者的易患因素相当,差异无统计学意义(P>0.05),见表1。
表1 两组一般资料比较
1.2 方法
根据随机数字表将入选病例随机分为缺血后适应组(Post-con)和对照组(Control)。
1.2.1 缺血后适应组 经PTCA球囊扩张,梗死相关血管开通并获有效再灌注后(前向血流TIMI≥2级),再灌注开始60 s时,扩张PTCA球囊阻塞IRA 30 s;排空球囊并撤出,再灌注120 s时,扩张球囊阻断IRA 30 s;排空球囊并撤出球囊,再灌注180 s时,扩张球囊阻断血流30 s时排空球囊并将球囊撤出体外;随后常规行支架植入术。
1.2.2 对照组 经PTCA球囊扩张,梗死相关血管开通并获有效再灌注后(前向血流TIMI≥2级),常规行支架植入术。
1.3 标本采集
在靶血管再灌注前和再灌注后4 h、12 h分别采静脉血3 mL,3000转/min离心10 min,取上清液置于-20℃冰箱中保存。
1.4 MDA、SOD、TNF-α、IL-6的測定
分别测定两组术前和术后4 h血清MDA、SOD的含量及两组术前和术后12 h血清TNF-α、血清IL-6含量。SOD含量检测采用黄嘌呤氧化酶法,MDA含量测定采用硫代巴比妥酸法,TNF-α含量、血清IL-6含量采用双抗体夹心ELISA法。方法严格按照试剂盒操作说明书进行操作。
1.5 统计学分析
使用SPSS15.0统计学软件进行统计分析,计量资料以(x±s)表示,采用t检验;计数资料采用χ2检验,P<0.05为差异有统计学意义。
2 结果
2.1 两组CK峰值比较
缺血后适应组CK峰值较对照组低[(2931.66±1089.56) vs (3919.97±1304.10)U/L,t=19.348,P<0.05]。
2.2 两组血清MDA、SOD、TNF-α、IL-6含量比较
术前两组MDA、SOD、TNF-α、IL-6差异无统计学意义(P>0.05)。术后两组MDA、TNF-α、IL-6较术前显著升高(P<0.05);SOD较术前显著降低(P<0.05);术后适应组MDA、TNF-α、IL-6低于对照组(P<0.05),SOD高于对照组(P<0.05)。见表2。
3 讨论
心肌缺血/再灌注损伤与其过程中氧自由基的大量产生、活化并引发心肌细胞氧化损伤密切相关[9,10]。活性氧自由基可作用于细胞膜、DNA、关键性蛋白导致细胞功能紊乱和死亡。正常细胞中存在抗氧化系统,包括抗氧化酶和抗氧化小分子。抗氧化系统可以清除细胞内的活性氧自由基,防止细胞发生氧化损伤。超氧化物歧化酶(SOD)是抗氧化酶系统中的关键酶。心肌缺血/再灌注会引起心肌细胞内SOD含量和活性的下降,因此细胞清除活性氧自由基、应对氧化损伤的能力下降[11-14]。1986年,Murry等[1]首先发现持续性缺血导致的损伤和梗死程度,会因之前反复短暂缺血发作而减轻,并定义这一现象为缺血预适应(ischemic preconditioning,IP)。2005年,Staat等[8]首先证实了缺血后适应的心肌保护作用。目前研究认为细胞MDA水平的高低可以间接反映细胞收到氧化损伤的程度。心肌缺血/再灌注过程中,活性氧自由基大量产生以及包括SOD在内的抗氧化酶合成减少并且活性降低,两者互相影响产生恶性循环,导致心肌细胞严重损害并产生大量MDA。
本研究結果显示,术后两组血清MDA含量均较术前显著升高,而血清SOD水平较术前显著降低。这一结果与之前国内外的研究结果一致,均表现为缺血/再灌注时心肌细胞损害增加,并且SOD的抗氧化损害水平降低。缺血/再灌注后适应组MDA水平低于对照组(P<0.05),而SOD水平高于对照组,表明缺血/再灌注后适应减少再灌注后血清SOD水平的下降程度,缺血/再灌注后适应可以使细胞抗氧化能力增强。同时,降低的血清MDA水平反映心肌细胞氧化损害程度减轻,也间接反映缺血/再灌注后适应的保护作用。CK峰值代表心肌梗死数量的大小,缺血/再灌注后适应组CK峰值显著低于对照组。缺血/再灌注后适应具有减少缺血心肌再灌注损伤的保护作用。依据上述,缺血后适应的心肌保护作用的机制可能与其能干预SOD的减少有关。
肿瘤坏死因子-α(TNF-α)是机体在应激情况下由单核巨噬细胞所产生的一种多肽,与细胞的炎症反应紧密相关。有观点认为,心肌缺血/再灌注损伤本质上也是一种强烈的炎性损伤[15,16]。研究证实[17,18],TNF-α参与心肌缺血/再灌注损伤中对心肌的损伤作用,且其表达水平在缺血/再灌注时显著增高。IL-6是促炎症细胞因子之一,参与心肌细胞缺血/再灌注损伤过程。IL-6可诱导肝脏产生大量急性反应产物,如hs-CRP,这已被认为是冠脉综合征的发病机制之一[19,20]。
本研究结果还表明,术前两组TNF-α、IL-6无显著差异(P>0.05)。术后两组TNF-α、IL-6较术前显著升高(P<0.05);术后适应组TNF-α、IL-6低于对照组(P<0.05)。缺血后处理可以减少急性心肌梗死急诊PCI再灌注后TNF-α、IL-6的生成,从而减轻心肌缺血/再灌注损伤的程度。
综上所述,后适应能够抑制心肌缺血/再灌注所引起的SOD水平下降,抑制MDA、TNF-α、IL-6水平的升高;缺血/再灌注后适应可以减轻急性心肌梗死急诊PCI再灌注后的再灌注损伤。这可能也是后适应方法可以保护缺血心肌的机制之一。
[参考文献]
[1] Murry CE,Jennings RB,Reimer KA. Preconditioning with ischemia:A delay of lethal cell injury in ischemic myocardium[J]. Circulation,1986,74(5):1124-1136.
[2] Yang JJ,Kettritz R,Falk RJ,et al. Apoptosis of endothelial cells induced by the neutrophil serine proteases proteinase 3 and elastase[J]. Am J Pathol,1996,149(5):1617-1626.
[3] Jolly SR,Kang WJ,Bailie MB,et al. Canine myocardial reperfusion injury:Its reduction by the combined administration of superoxide dismutase and catalase[J]. Circ Res,1984,54(3):277-285.
[4] Reimer KA,Lowe JE,Rasmussen MM,et al. The wava-front phenomenon of ischemic cell death.1.Myocardial infarct size vs duration of coronary occlusion in dogs[J]. Circulation,1977,56(5):786-794.
[5] Zhao ZQ,Nakamura M,Wang NP,et al. Dynamic progression of contractile and endothelial dysfunction and infarct extension in the late phase of reperfusion[J]. J Surg,2000,94(2):133-144.
[6] Metzstein MM,Stanfield GM,Horvitz HR. Genetics of programmedcell death in C. elegans:Past,present and future[J].Trends Genet,1998,14(10):410-416.
[7] Gottlied RA,Burleson KO,Kloner RA,et al. Reperfusion injury induces apoptosis in rabbit cardiomyocytes[J]. J Clin Invest,1994,94(4):1621-1628.
[8] Staat P,Rioufol G,Piot C,et al. Postconditioning the Human Heart[J]. Circulation,2005,112(14):2143-2148.
[9] Rentrop KP,Cohen M,Blanke H,et al. Changes in collateral filling after controlled coronary artery occlysion by an angioplasty balloon in human subjects[J]. J Am Coll Cardiol,1985,5(1):587-592.
[10] Tan J,MA Z,Han L,et al. Caffeic acid phenethyl ester possesses potent cardioprotective effects in a rabbit model of acute myocardial ischemia-reperfusion injury[J]. Am J Physiol Heart Circ Physiol,2005,289(5):2265-2271.
[11] Liu R,Tao L,Gao E,et al. Anti-apoptotic effects of rosiglitazone in hypercholesterolemic rabbits subjected to myocardial ischemia and reperfusion[J]. Cardiovasc-Res,2004, 62(1):135-144.
[12] 王世華. 急性心肌梗死患者肿瘤坏死因子和超氧化物歧化酶水平的研究[J]. 徐州医学院学报,2005,25(5):839-842.
[13] Bucciarelli G,Kaneko M,Ananthakrishnan R,et al. Receptor for advanced-glycation end products:Key modulator of myocardial ischemic injury[J]. Circulation,2006, 113(9):1226-1234.
[14] Chen K,Chow E. Antioxidants and myocardial ischemia:Reperfusion injuries[J]. Chang Gung Med J,2005,28(6):369-377.
[15] Li D,Qu Y,Tao L,et al. Inhibition of iNOS protects the aging heart against beta-adrenergic receptor stimylation-induced cardiac dysfunction and myocardial ischemic injury[J]. J Surg Res,2006,131(1):64-72.
[16] Tao L,Gao E,Bryan S. et al. Cardioprotective effects of thioredoxin in myocardial ischemia and reperfusion:Role of S-nitrosation[J]. Proc Natl Acad Sci,2004,101(31):11471-11476.
[17] Razavi M,Hamtilton A,Feng Q. Modulation of apoptosis by nitric oxide:Implications in myocardial ischemia and heart failure[J]. Pharmacol Ther,2005,106(2):147-162.
[18] Ji S,Yue H,Wu M,et al. Effects of phytoestrogen genistein on myocardial ischemia/reperfusion injury and apoptosis in rabbits[J]. Acta Pharmacol Sin,2004,25(3):306-312.
[19] Okumura H,Nagaya N,Itoh T,et al. Adrenomedullin infusion attenuates myocardial ischemia/reperfusion injury through the phosphatidylinositol 3-kinase/Akt-dependent pathway[J]. Circulation,2004,109(2):242-248.
[20] Heinrich PC,Castell JV,Andus T. Interleukin-6 and the acute phase response[J]. Biol Chem J,1990,265(3):621-636.
(收稿日期:2015-09-01)
