宫颈癌患者血清可溶性Endoglin水平变化观察
2015-05-08钟佳静吴菲远
钟佳静 吴菲远
宫颈癌患者血清可溶性Endoglin水平变化观察
钟佳静 吴菲远
目的 研究宫颈癌患者血清可溶性Endoglin水平变化及其临床价值。方法 应用酶联免疫吸附试验法(ELISA)对31例正常人(正常对照组)及63例宫颈癌患者(宫颈癌组)血清可溶性Endoglin水平进行检测, 并比较38例宫颈癌患者根治手术前后血清可溶性Endoglin水平。结果 宫颈癌组患者血清可溶性Endoglin水平(5.01±1.03)μg/L明显高于正常对照组(3.57±0.30)μg/L (P<0.01), 血清可溶性Endoglin水平与宫颈癌患者临床分期有明显相关, 与宫颈癌组患者年龄和病理类型无明显相关;Ⅳ期宫颈癌血清可溶性Endoglin水平(6.41±0.22)μg/L明显高于Ⅲ期(5.25±0.25)μg/L (P<0.01), Ⅲ期血清可溶性Endoglin水平明显高于Ⅱ期(4.38±0.26)μg/L (P<0.01), Ⅱ期血清可溶性Endoglin水平明显高于Ⅰ期(3.68±0.29)μg/L (P<0.05), Ⅰ期血清可溶性Endoglin水平与正常对照组比较, 差异无统计学意义(P>0.05), 血清可溶性Endoglin在宫颈癌患者根治术后的表达水平(3.85±0.71)μg/L明显低于术前(4.38±0.68)μg/L (P<0.01)。结论 血清可溶性Endoglin表达水平可作为反映宫颈癌患者病情、疗效判断和预后评价的一个参考指标。
可溶性Endoglin;宫颈癌;预后
宫颈癌是妇科三大恶性肿瘤之一, 肿瘤血管新生为促进肿瘤发生、进展、浸润和转移的非常重要因素, 为肿瘤组织的增殖提供了良好的条件[1,2];Endoglin又称为CD105,已有研究表明Endoglin是血管生成必定需要的条件, 而且Endoglin在许多类型肿瘤组织的内皮细胞中表达状况均为上调, 与肿瘤的发生、发展、侵袭和转移密切相关, 是肿瘤血管生成的标志物[3];作者通过检测63例不同病理类型、不同年龄段、不同临床分期宫颈癌患者血清可溶性Endoglin水平, 并且比较38例宫颈癌患者手术前后血清可溶性Endoglin水平的变化情况, 了解及评估血清可溶性Endoglin在宫颈癌的临床价值和应用依据, 增强临床医师对这一指标检测的重视。现报告如下。
1 资料与方法
1.1 一般资料 正常对照组31例为在湛江市中心人民医院进行体检的女性健康查体者;宫颈癌组63例为湛江市中心人民医院住院患者, 均为女性, 其中鳞癌49例、腺癌9例、粘液表皮样癌5例;Ⅰ期13例, Ⅱ期15例, Ⅲ期19例, Ⅳ期16例。两组一般资料比较, 差异无统计学意义(P>0.05),具有可比性。
1.2 实验操作技术及方法 晨起空腹时抽取静脉血2.5 ml,室温下静置3 h后, 3000 r/min离心15 min, 分离出血清1 ml,置于1.5 ml聚丙二醇脂试管内, 放入-20℃冰箱保存, 成批次采用ELISA检测血清可溶性Endoglin水平;31例正常对照组和63例宫颈癌组患者于术前检测血清可溶性Endoglin水平, 其中的38例宫颈癌组患者分别于术前和术后(29±3)d检测血清可溶性Endoglin水平。
1.3 统计学方法 采用SPSS18.0统计学软件进行数据统计分析。计量资料以均数±标准差表示, 采用t检验。P<0.05表示差异具有统计学意义。
2 结果
2.1 正常对照组和不同病期宫颈癌患者血清可溶性Endoglin水平比较 血清可溶性Endoglin水平临床Ⅳ期>临床Ⅲ期>临床Ⅱ期>正常对照组, 差异有统计学意义(P<0.05或0.01);临床Ⅰ期与正常对照组比较, 差异无统计学意义(P>0.05)。见表1。
表1 正常对照组和不同病期宫颈癌患者血清可溶性Endoglin水平比较
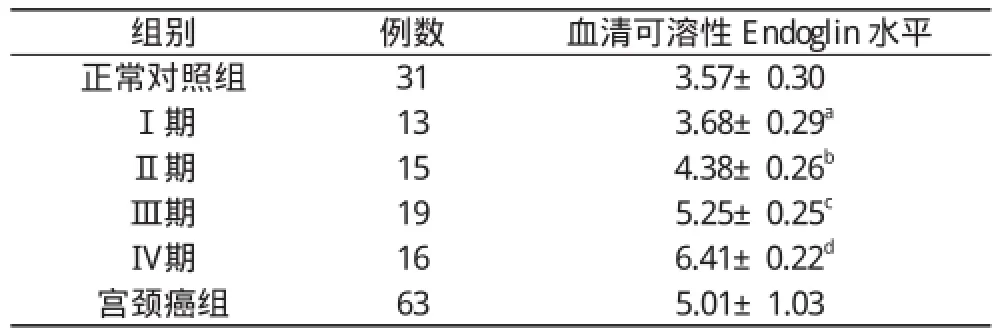
表1 正常对照组和不同病期宫颈癌患者血清可溶性Endoglin水平比较
注:临床Ⅰ期与正常对照组比较,aP>0.05;临床Ⅱ期与Ⅰ期比较,bP<0.05;临床Ⅲ期与Ⅱ期比较,cP<0.01;临床Ⅳ期与Ⅲ期比较,dP<0.01;宫颈癌组与正对照组比较,eP<0.01
组别例数血清可溶性Endoglin水平正常对照组313.57±0.30Ⅰ期13 3.68±0.29aⅡ期15 4.38±0.26bⅢ期19 5.25±0.25cⅣ期16 6.41±0.22d宫颈癌组635.01±1.03
2.2 年龄≥50岁宫颈癌患者血清可溶性Endoglin水平(5.02±0.98) μg/L与年龄<50岁宫颈癌患者血清可溶性Endoglin水平(5.01±1.07) μg/L比较, 差异无统计学意义(P>0.05), 说明血清可溶性Endoglin水平与宫颈癌患者的年龄之间无明显相关性。
2.3 血清可溶性Endoglin表达水平和宫颈癌患者病理类型的关系 腺癌、鳞癌、粘液表皮样癌等类型的宫颈癌患者之间血清可溶性Endoglin水平两两比较, 差异无统计学意义(P>0.05), 提示宫颈癌患者病理类型和血清可溶性Endoglin水平之间无明显相关性。见表2。
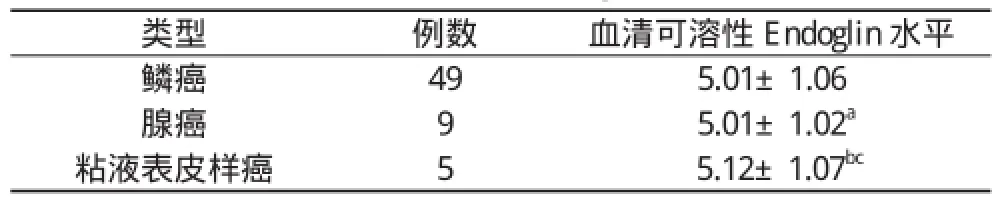
表2 血清可溶性Endoglin表达水平和宫颈癌患者病理类型的关系( x-±s, μg/L)
2.4 38例宫颈癌患者根治手术后测定血清可溶性Endoglin水平(3.85±0.71) μg/L明显低于手术前血清可溶性Endoglin水平(4.38±0.68) μg/L, 两者比较差异有统计学意义(P<0.01)。
3 讨论
恶性肿瘤的浸润、生长和转移均有赖于肿瘤血管不断生成与有效的血液供应, 肿瘤的血液供应是通过与宿主正常血管相互混合从而形成新的肿瘤微循环进而实现的, 抗血管生成疗法是目前全世界治疗肿瘤的研究热点[4-7]; Kopczy ńska等[8]研究发现, 37例Ⅰ期非小细胞肺癌患者手术后7 d血浆可溶性Endoglin 水平明显低于手术前;梁启廉等[9]通过建立动物模型, 研究发现抗Endoglin单克隆抗体可明显抑制人类胰腺癌细胞株PC-3的生长, 有希望作为胰腺癌的生物基因治疗方法。
本研究结果显示63例宫颈癌患者血清可溶性Endoglin表达水平显著高于31例正常对照组Endoglin表达水平, 提示正常人与宫颈癌患者之间血清可溶性Endoglin表达水平有一定的差异性, 临床Ⅳ期宫颈癌患者血清可溶性Endoglin水平明显高于临床Ⅲ期、临床Ⅲ期血清可溶性Endoglin水平高于临床Ⅱ期、临床Ⅱ期血清可溶性Endoglin水平高于临床Ⅰ期, 临床Ⅰ期血清可溶性Endoglin水平与正常对照组比较差异无统计学意义, 提示血清可溶性Endoglin水平可能与宫颈癌的发展程度有一定程度的相关性, 本研究发现血清可溶性Endoglin水平与宫颈癌患者病理类型、年龄无明显相关;本研究检测血清可溶性Endoglin水平在38例宫颈癌患者手术前后的状况, 发现术后宫颈癌患者血清可溶性Endoglin水平较术前血清可溶性Endoglin水平明显降低;结合以上结果可以知道血清可溶性Endoglin表达水平可作为反映宫颈癌患者病情、疗效判断和预后评价的一个参考指标。
[1] Dubinski W, Gabril M, Iakovlev VV, et al.Assessment of the prognostic significance of endoglin(CD105) in clear cell renal cell carcinoma using automated image analysis.Hum Pathol, 2012, 43(7):1037-1043.
[2] Liang QL, Wang BR, Li ZY, et al.Construction of eukaryotic expression vector of TSLC1 gene.Arch Med Sci, 2011, 7(4):579-585.
[3] 梁启廉, 李志东, 吴斌华, 等.抗CD105单克隆抗体对大肠癌生长的抑制作用.中华实验外科杂志, 2009, 26(2):165-166.
[4] Zhuo H, Lyu Z, Su J, et al.Effect of Lung Squamous Cell Carcinoma Tumor Microenvironment on the CD105+Endothelial Cell Proteome.J Proteome Res, 2014, 13(11):4717-4729
[5] Zhang Y, Hong H, Engle JW, et al.Positron Emission Tomography and Optical Imaging of Tumor CD105 Expression with a Dual-Labeled Monoclonal Antibody.Mol Pharm, 2012, 9(3):645-653.
[6] Banerjee S, Dhara SK, Bacanamwo M.Endoglin is a novel endothelial cell specification gene.Stem Cell Res, 2012, 8(1):85-96.
[7] 梁启廉, 陈小东, 李建文, 等.胃癌及癌前病变组织中Endoglin标记的微血管密度表达意义.肿瘤研究与临床, 2006, 18(2):85-86.
[8] Kopczyńska E, Dancewicz M, Kowalewski J, et al.Influence of surgical resection on plasma endoglin (CD105) level in non small cell lung cancer patients.Exp Oncol, 2012, 34(1):53-56.
[9] 梁启廉, 李志东, 吴斌华, 等.抗 Endoglin 单克隆抗体对裸鼠胰腺癌移植瘤生长的影响.第四军医大学学报, 2009, 30(6): 520-522.
Observation of soluble Endoglin level changes in cervical cancer patients
ZHONG Jia-jing, WU Fei-yuan.Zhanjiang Jiuhe Hospital, Zhanjiang 524000, China
Objective To research changes of soluble Endoglin level and its clinical significance in cervical cancer patients.Methods Enzyme-linked immuno sorbent assay (ELISA) was applied for serum soluble Endoglin level detection in 31 normal people (normal control group) and 63 cervical cancer patients (cervical cancer group).Comparison was made on serum soluble Endoglin level in 38 cervical cancer patients before and after radical operation.Results Cervical cancer patients had much higher serum soluble Endoglin level as (5.01±1.03) μg/L than (3.57±0.30) μg/L of the normal control group (P<0.01).Serum soluble Endoglin level was obviously related with clinical stage of cervical cancer patients, while it has no relationship with age and pathological type of cervical cancer patients.Stage Ⅳ cervical cancer had much higher serum soluble Endoglin level as (6.41±0.22) μg/L than (5.25±0.25) μg/L of stage Ⅲ (P<0.01); stage Ⅲ cervical cancer had much higher serum soluble Endoglin level than (4.38±0.26) μg/L of stage Ⅱ (P<0.01); stage Ⅱ cervical cancer had much higher serum soluble Endoglin level than (3.68 ±0.29) μg/L of stage Ⅰ (P<0.05).The difference of serum soluble Endoglin level between stage Ⅰ and normal control group had no statistical significance (P>0.05).Serum soluble Endoglin level in cervical cancer patients after operation was obviously lower as (3.85±0.71) μg/L than (4.38±0.68) μg/L before operation (P<0.01).Conclusion Expression level of serum soluble Endoglin can be used as a referring index for showing disease status, judging curative effect and evaluating prognosis in cervical cancer patients.
Soluble Endoglin; Cervical cancer; Prognosis
10.14163/j.cnki.11-5547/r.2015.17.003
2015-01-23]
524000 湛江久和医院(钟佳静);湛江市中心人民医院妇产科(吴菲远)
