老年慢性血栓栓塞性肺动脉高压患者的心肺运动试验研究
2015-04-21奚群英柳志红赵智慧马秀平熊长明倪新海
奚群英,柳志红,赵智慧,顾 晴,罗 勤,马秀平,熊长明,倪新海
老年慢性血栓栓塞性肺动脉高压患者的心肺运动试验研究
奚群英,柳志红*,赵智慧,顾 晴,罗 勤,马秀平,熊长明,倪新海
(中国医学科学院北京协和医学院阜外医院心内科,国家心血管病中心心血管疾病国家重点实验室,肺血管病中心,北京 100037)
明确老年慢性血栓栓塞性肺动脉高压(CTEPH)患者与年轻患者相比心肺运动试验(CPET)指标的变化。2011年1月至2014年5月在阜外医院肺血管病房住院的57名CTEPH患者行CPET。按年龄是否≥60岁分为老年组(19例)和青年组(38例)。两组间性别、既往深静脉血栓形成(DVT)病史的概率、接受肺动脉高压靶向药物治疗的概率、基于核素肺通气/灌注显像计算的肺血管阻塞率、世界卫生组织(WHO)功能分级差异无统计学意义(>0.05)。与青年组相比,老年CTEPH患者运动心率反应减慢,一秒用力呼气量(FEV1)、用力肺活量(FVC)下降,峰值分钟通气量(VE@峰值)、峰值潮气量(VT@峰值)更低,峰值氧脉搏(VO2/HR@峰值)占预计值的百分率增高,无氧阈(AT)时的生理死腔通气与潮气量比值(VD/VT)增高,峰值时的潮气末氧分压更低。老年CTEPH患者有特殊的CPET表现。
慢性血栓栓塞性肺动脉高压;心肺运动试验;老年人
慢性血栓栓塞性肺动脉高压(chronic thromboembolic pulmonary hypertension,CTEPH)是肺血栓栓塞症少见而严重的结局。患者因右心衰竭反复住院,甚至死亡。心肺运动试验(CPET)能客观、精确地评估人体心肺储备功能,为心血管、肺疾病患者提供有价值的诊断和预后信息。研究显示,CTEPH患者的通气效率不仅显著低于近端肺血管血栓阻塞程度相同但不合并肺动脉高压(pulmonary artery hypertension,PAH)的慢性肺血栓栓塞症患者[1];也显著低于特发性PAH的患者[2]。异常增高的生理死腔量可能是CTEPH患者通气效率显著降低的原因[2]。我们既往的研究比较了CTEPH患者与慢性肺血栓栓塞症患者CPET各指标的差异,发现每分钟通气量(minute ventilation volume,VE)/二氧化碳生成量(CO2production,VCO2)最低值是预测急性肺血栓栓塞症后发生CTEPH的敏感指标[3]。而老年人随着其年龄的增长,细胞组织结构的改变和功能的退化,在CPET中形成有规律的改变。本前瞻性研究的目的旨在明确老年CTEPH患者与年轻患者相比CPET指标的变化。
1 对象与方法
1.1 研究对象及分组
筛选对象为2011年1月至2014年5月在阜外医院肺血管病房住院的CTEPH患者。CTEPH的诊断标准依据2009年欧洲心脏病学协会/欧洲呼吸协会(the European Society of Cardiology/the European Respiratory Society,ESC/ERS)PAH诊治指南[4]。排除标准:(1)有肺动脉血栓内膜切除术史;(2)有并发的胸廓或肺部疾病;(3)超声心动图提示患者左心功能不全;(4)患者不能完成CPET;(5)年龄≤14周岁。最终纳入57例患者。按年龄是否≥60岁分为老年组(19例)和青年组(38例)。研究经阜外医院伦理委员会批准,患者均签署知情同意书(伦理号2012BJYYEC-050-02)。
1.2 心肺运动试验
患者经过静息肺功能测试,在医师监督下进行症状限制的功率递增式直立踏车运动试验[5]。气体交换采用逐次呼吸测量系统;功率递增幅度的选择根据对患者病史包括日常运动量和运动强度、体格检查和肺功能状况综合决定。递增方案为10~15W/min。无高危性生命体征(如严重心律失常、低血压等)出现时,尽量鼓励患者运动。CPET过程中,如出现症状(如胸闷、心慌、疲劳等),则停止运动,监测生命体征至恢复正常生理状态。测定VE、生理死腔通气与潮气量比值(physiologic dead space fraction,VD/VT)、潮气末二氧化碳分压(end-tidal partial pressure of CO2,PetCO2)、VCO2、潮气末氧分压(end-tidal partial pressure of O2,PetO2)、氧耗量(oxygen consumption,VO2)、功率、血压、心率、血氧饱和度等,计算出峰值氧耗量(VO2@峰值)、氧脉搏(oxygen consumption /heart rate,VO2/HR)、无氧阈(anaerobic threshold,AT)、VE/VCO2最低值、VE/VCO2斜率等参数。
1.3 核素肺通气/灌注显像
患者住院期间完成核素肺通气/灌注显像。血管阻塞率(percentage of vascular obstruction by ventilation-perfusion lung scanning,PVO)以既往文献报道的方法[6]计算。
1.4 6min步行距离测试
由不了解患者CPET结果、且经专业培训的护士进行6min步行距离(6MWD)测试。
1.5 实验室检测
患者在入院次晨抽血。N端脑钠肽前体(N-terminal pro-brain natriuretic peptide,NT-proBNP)水平以酶联免疫分析试剂盒(奥地利Biomedica Medizinprodukte GmbH& Co KG公司)测定。血气分析以血气分析仪(美国Nova Biomedical公司)检测。
1.6 统计学处理
采用SPSS16.0软件进行统计学分析。计量资料以均数±标准差表示;计数资料以例数及百分率表示。计量资料的组间差异采用检验;计数资料的组间差异采用卡方检验。年龄与心肺运动各指标间的关系采用相关关系分析;VO2/HR@峰值占预计值的百分比、VD/VT@AT、PetO2@峰值与各指标的关系采用多元线性回归分析。以<0.05为差异有统计学意义。
2 结 果
2.1 两组患者临床资料比较
表1结果表明,性别比例在两组间分布均衡。青年组患者的体质量指数比老年组更高(<0.01)。老年CTEPH患者有更高的NT-proBNP水平(<0.05)。两组之间的既往深静脉血栓形成(deep venous thrombosis,DVT)病史的概率和接受肺动脉高压PAH向药物治疗的概率差异均无统计学意义(>0.05)。超声心动图检测的右心室舒张末期内径及右室/左室舒张末期内径比值差异均无统计学意义(>0.05)。两组患者之间基于核素肺通气/灌注计算的PVO差异无统计学意义(>0.05)。世界卫生组织(the World Health Organization, WHO)功能分级和6MWD在两组患者之间差异也无统计学意义(>0.05)。

表1 CTEPH老年患者与青年患者的临床资料比较
CTEPH: chronic thromboembolic pulmonary hypertension; BMI: body mass index; WHO-FC: World Health Organization functional class; DVT: deep venous thrombosis; RVEDD: right ventricular end-diastolic diameter; LVEDD: left ventricular end-diastolic diameter; sPAP: systolic pulmonary arterial pressure; PVO: percentage of vascular obstruction by ventilation-perfusion lung scanning; SaO2: oxygen saturation; NT-proBNP: N-terminal pro-brain natriuretic peptide; 6MWD: 6-min walking distance. 1mmHg=0.133kPa. Compared with the elderly group,*<0.05,**<0.01
2.2 老年CTEPH患者的心肺运动试验特点
表2结果表明,两组患者之间的VO2/功率(work rate,WR)斜率、VO2@AT及VO2@峰值(包括占预计值的百分率)差异均无统计学意义(>0.05)。但与青年组相比,老年组患者的VO2/HR@峰值占预计值的百分率显著增高(<0.05)。同时,老年患者在运动中(包括AT点和峰值时)的心率反应较青年组明显减慢(<0.05)。老年患者的1秒用力呼气量(forced expiratory volume in one second,FEV1)和用力肺活量(forced vital capacity,FVC)均低于青年组(<0.01),但FEV1/FVC两组患者之间差异无统计学意义(>0.05)。青年组AT点的呼吸储备(breath reserve,BR)及峰值时的潮气量(tidal volume,VT)显著高于老年组(<0.01)。VD/VT@AT在老年组更高(<0.05),但至峰值时两组间差异无统计学意义(>0.05)。峰值时的PetO2在青年组更高(<0.05),而同时点的PetCO2在老年组有增高的趋势,但差异无统计学意义(>0.05)。VE/VCO2在AT和峰值点的比值、和比值的最低点及其斜率在两组间差异均无统计学意义(>0.05)。
相关关系分析中,与年龄显著相关的心肺运动指标包括FEV1(=-0.636,<0.001)、FVC(=-0.541,<0.001)、VO2/HR@峰值占预计值的百分率(=0.470,<0.001)、VO2@峰值占预计值的百分率(=0.343,=0.009)、VE@峰值(=-0.494,<0.001)、BR@AT(=-0.395,=0.002)、VT@峰值(=-0.406,=0.002)、VD/VT@AT(=0.356,=0.007)、HR@AT(=-0.461,<0.001)、HR@峰值(=-0.649,<0.001)、PetO2@峰值(=-0.281,=0.034)。多元线性回归分析结果显示,决定VO2/HR@峰值占预计值的百分率的指标包括FVC和峰值时的PetO2、HR、VT;决定VD/VT@AT的指标包括年龄和AT点时的VE、VE/VCO2、PetCO2。
3 讨 论
CTEPH以继发于肺血栓栓塞的肺血管重构为病理基础,以渐进的右心衰竭为临床特征[7]。CTEPH患者的CPET表现为显著下降的运动能力(以峰值VO2为代表)和显著下降的气体交换效率(以VE、VCO2的关系和VD/VT为代表)[1]。而老年人随着年龄增长出现的各组织、器官功能的退化,CPET也出现一些规律性的改变。本研究旨在比较CTEPH老年患者与青年患者CPET结果有何不同,并探讨其可能的机制。研究结果显示,CTEPH老年患者与青年患者相比有其特殊的CPET表现。主要体现在:(1)老年组患者的VO2/HR@峰值占预计值的百分率显著增高;(2)VD/VT@AT在老年组更高;(3)CTEPH老年组的PetO2@峰值低于青年组。
研究已证实,人体运动能力随着年龄的增长逐渐减退[8];体育锻炼可逆转运动能力的衰退[9,10]。CPET中随年龄增长而改变的具体的指标包括:VO2@峰值、VO2@峰值/HR随年龄增长逐渐降低;心率、收缩压随运动增高的反应在老年人中减弱;通气和换气效率的指标FEV1、FVC、VD/VT老年人较青年人差[8−14]。本研究显示,老年患者在运动中(包括AT点和峰值时)的心率反应较青年组明显减慢。因此老年组患者的VO2/HR@峰值占预计值的百分率显著增高的结果应主要来自于老年患者心率的减慢,此结果与既往的研究相符合[1]。本研究中老年组的VO2@AT及VO2@峰值(包括占预计值的百分率)与青年组相比差异均无统计学意义,推测是因为CTEPH所致显著下降的运动能力掩盖了年龄的影响。VD/VT@AT在老年CTEPH患者更高,说明亚极量运动时老年患者的肺灌注不足更为显著。老年患者的PetO2@、VT@峰值、VE@峰值均低于青年组,说明老年组潮气末肺泡氧分压的改变与其通气泡氧分压的改变与其通气能力降低有关。有研究者认为,健康老年人的CPET“年龄效应”可归结为FEV1的降低和运动时心率反应的下降[8]。本研究证实老年CTEPH患者的表现与其通气、换气效率降低和心率反应下降有关。
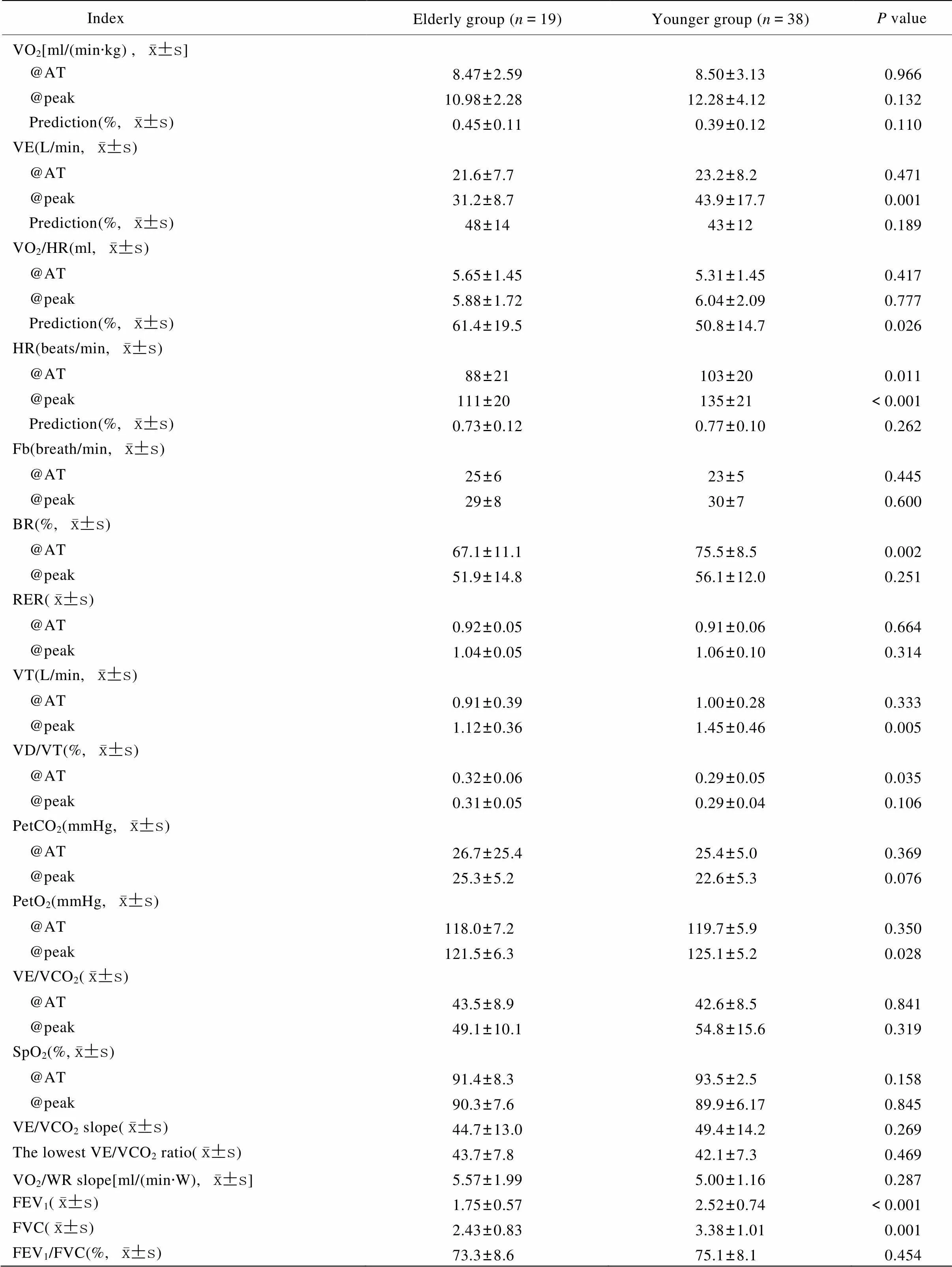
表2 CTEPH老年组与青年组的心肺运动试验比较
CTEPH: chronic thromboembolic pulmonary hypertension; VO2: oxygen consumption; AT: anaerobic threshold; VE: minute ventilation volume; HR: heart rate; Fb: breathing frequency; BR: breathing reserve; RER: respiratory exchange rate; VT: tidal volume; VD/VT: physiologic dead space fraction; PetCO2: end-tidal partial pressure of CO2; PetO2:end-tidal partial pressure of O2; VCO2: CO2production; SpO2: oxygen saturation; WR: work rate; FEV1: forced expiratory volume in one second; FVC: forced vital capacity. 1mmHg=0.133kPa
综上所述,随着CTEPH老年患者运动心率反应的减慢、通气换气效率的减低,与青年患者相比,老年患者的VO2/HR@峰值占预计值的百分率增高,AT时的VD/VT增高,峰值时的PetO2下降。
[1] McCabe C, Deboeck G, Harvey I,. Inefficient exercise gas exchange identifies pulmonary hypertension in chronic thromboembolic obstruction following pulmonary embolism[J]. Thromb Res, 2013, 132(6): 659-665.
[2] Zhai Z, Murphy K, Tighe H,. Differences in ventilatory inefficiency between pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension[J]. Chest, 2011, 140(5): 1284-1291.
[3] Xi Q, Zhao Z, Liu Z,. The lowest VE/VCO2ratio best identifies chronic thromboembolic pulmonary hypertension[J]. Thromb Res, 2014, 134(6): 1208-1213.
[4] Galie N, Hopper MM, Humbert M,. Guidelines for the diagnosis and treatment of pulmonary hypertension: the Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS), endorsed by the International Society of Heart and Lung Transplantation (ISHLT)[J]. Eur Heart J, 2009, 30(20): 2493-2537.
[5] Guazzi M, Admas V, Conraads V,. EACPR/AHA Joint Scientific Statement. Clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations[J]. Eur Heart J, 2012, 33(23): 2917-2927.
[6] Meyer G, Collignon MA, Guinet F,. Comparison of perfusion lung scanning and angiography in the estimation of vascular obstruction in acute plmonary embolism[J]. Eur J Nucl Med, 1990, 17(6−8): 315-319.
[7] Delcroix M, Vonk Noordegraaf A, Fadel E,. Vascular and right ventricular remodeling in chronic thromboembolic pulmonary hypertension[J]. Eur Respir J, 2013, 41(1): 224-232.
[8] Schneider J. Age dependency of oxygen uptake and related parameters in exercise testing: an expert opinion on reference values suitable for adults[J]. Lung, 2013, 191(5): 449-458.
[9] Woo JS, Derleth C, Stratton JR,. The influence of age, gender, and training on exercise efficiency[J]. J Am Coll Cardiol, 2006, 47(5): 1049-1057.
[10] Deley G, Kervio G, Van Hoecke J,. Effects of a one-year exercise training program in adults over 70 years old: a study with a control group[J]. Aging Clin Exp Res, 2007, 19(4): 310-315.
[11] Simoes RP, Bonjorno JC Jr, Beltrame T,. Slower heart rate and oxygen consumption kinetic responses in the on-and off-transient during a discontinuous incremental exercise: effects of aging[J]. Braz J Phys Ther, 2013, 17(1): 69-76.
[12] Hollenberg M, Yang J, Haight TJ,. Longitudinal changes in aerobic capacity: implications for concepts of aging[J]. J Gerontol A Biol Sci Med Sci, 2006, 61(8): 851-858.
[13] Sheikh K, Paulin GA, Svenningsen S,. Pulmonary ventilation defects in older never-smokers[J]. J Appl Physiol (1985), 2014, 117(3): 297-306.
[14] Itoh H, Ajisaka R, Koike A,. Heart rate and blood pressure response to ramp exercise and exercise capacity in relation to age, gender, and mode of exercise in a healthy population[J]. J Cardiol, 2013, 61(1): 71-78.
(编辑: 周宇红)
Cardiopulmonary exercise testing for elderly with chronic thromboembolic pulmonary hypertension
XI Qun-Ying, LIU Zhi-Hong*, ZHAO Zhi-Hui, GU Qing, LUO Qin, MA Xiu-Ping, XIONG Chang-Ming, NI Xin-Hai
(Center for Pulmonary Vascular Diseases, State Key Laboratory of Cardiovascular Diseases, National Center for Cardiovascular Diseases, Department of Cardiology, Fuwai Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100037, China)
To investigate the differences in the indices of cardiopulmonary exercise testing (CPET) between the elderly and young patients with chronic thromboembolic pulmonary hypertension (CTEPH).Fifty-seven CTEPH patients admitted to the Center for Pulmonary Vascular Diseases, Fuwai Hospital during January 2011 to May 2014 were enrolled in this study. They all underwent CPET, and were divided into 2 groups according to their age, that is, the elderly group (≥60 years old,=19), and the younger group (<60 years old,=38).There was no difference in gender, prevalence of deep venous thrombosis (DVT), pulmonary targeted drug therapy, pulmonary vascular occlusion rate detected by ventilation-perfusion lung scanning, and WHO functional class between the 2 groups. Compared with the younger patients, the elderly CTEPH patients had lower heart rate response during exercise, decreased forced expiratory volume in one second (FEV1) and forced vital capacity (FVC), lower peak minute ventilation (VE peak) and tidal volume (VT peak). While the percentage of oxygen uptake/heart rate (VO2/HR) peak to prediction and physiologic dead space fraction (VD/VT) were significantly increased in the elderly patients, along with decreased PetO2peak.The elderly CTEPH patients have their own characteristics in the parameters of CPET.
chronic thromboembolic pulmonary hypertension; cardiopulmonary exercise testing; aged
R543.2; R592
A
10.11915/j.issn.1671-5403.2015.03.039
(2010F11).
2014−12−17;
2015−02−02
中央级公益性科研院所基本科研业务费(2010F11)
柳志红, E-mail: liuzhihong@fuwai.com
